International Journal of
eISSN: 2574-8084


Case Report Volume 2 Issue 5
1Department of Radiology, Teerthanker Mahaveer University, India
2Department of Obstetrics & Gynecology, Teerthanker Mahaveer University, India
Correspondence: Arjit Agarwal, Department of Radiology, Teerthanker Mahaveer Medical College & Research Centre, Teerthanker Mahaveer University, A-46, Gandhi Nagar, Moradabad-244001 (Uttar Pradesh), India, Tel -9012209103
Received: January 26, 2017 | Published: March 31, 2017
Citation: Agarwal A, Agarwal S. Role of imaging and its advances in prediction of preterm birth. Int J Radiol Radiat Ther. 2017;2(5):115-117. DOI: 10.15406/ijrrt.2017.02.00036
Preterm Birth (PTB) is one of the leading causes of neonatal mortality and morbidity worldwide, compared to the term deliveries. The survivors come across long term morbidity in the form of sensory, motor, cognitive and behavioral deficits. Hence, accurate and early prediction of the preterm is important for timely intervention and prevention of the fetal outcome. Contemporary method of assessment relies on the clinical and radiological signs, however still the rate of PTB is nearly constant over the years. This review discusses the role of various Ultrasonographic (USG) parameters & advances in prediction of PTB; based on the current medical literature.
Keywords:preterm, cervix, elastography, adrenal gland, premature delivery
PTB, preterm birth; PTD, preterm delivery; PPROM, preterm premature rupture of meMbranes; USG, ultrasonography; RTE, real time elastography; ARFI, acoustic radiation force impulse; VTQ, virtual touch tissue quantification; HPA, hypothalamic pituitary adrenal; FZE, fetal zone enlargement; cAGV, corrected adrenal gland volume; FZ, fetal zone; TZ, transitional zone; DZ, definitive zone; DHEA-S, dehydroepinadrosterone-sulfate; FZE, fetal zone enlargement
Preterm delivery (PTD) is defined as premature birth prior to the completion of 37weeks of gestation and is responsible for nearly 75% of all neonatal deaths.1 WHO estimation of the preterm births is approx 11%,2 hence the main clinical and diagnostic challenge is to identify high risk patients and to prolong the pregnancy.3
Altered consistency of the cervix can lead to early labour and preterm birth, which is universally evaluated with Bishop’s scoring and USG measurement of the cervical length. Bishop’s score is relatively subjective and clinician dependant where there can be discrepancy in the score and hence defines low predictive value. Similarly the assessment of the uterine cervical length is also unreliable and variable. The correlation of the previous obstetrics, clinical history, fetal fibronectin, Bishop’s score and USG measurement of the cervical morphology (funnelling & shortening) can lead to better prediction of the preterm birth.4,5
Recently, the role of radiologist in the cervical assessment has been enhanced by virtue of the arrival of the elastography and its variable techniques, which will be discussed. An innovative, indirect and relatively less studied parameter for the PTB prediction is assessment of the Fetal adrenal gland volume and dimensions.
PTB prediction is important for both the clinician’s and the patient’s perspective as it can lead to planned management of such cases and reduces the neonatal morbidity. There is 50% increased risk of PTB in a woman who has experienced two or more prior PTBs.6 Clinical evaluation of the cervix is usually done by finger palpation method which measures the length from the level of external os to the cervico-vaginal junction giving the Bishop’s scoring. The cervical isthmus portion could not be assessed; which leads to the underestimation of the length by nearly 12mm compared to the USG in about 80% cases during the second and third trimester.7 Here we will discuss the routine USG assessment of the cervix with role of cervical elastography and fetal adrenal gland biometry in prediction of the preterm birth (Figure 1).

Figure 1 Transabdominal Ultrasound of the cervix. (A) Cervical Length measurement. (B) Funnelling of the cervix (white arrow) and amniotic fluid debris near internal os (asterisk*).
Sonography of cervix
Evaluation of maternal cervix is an integral part of routine obstetrical USG. There are three approaches for cervical scanning which are transabdominal, transvaginal and translabial.8 The translabial and transvaginal approaches are usually avoided in cases of high risk of PTB with procedure related risk of chorioamnionitis, vaginal bleeding and cervical stimulation. However, the transabdominal approach may be less accurate and affected by distention of the urinary bladder and fetal head size.9
Multicentric study by Iams et al.,10 proposed the concept of ‘short cervix’ on USG as less than 25mm (or <10th centile length at 24-28weeks). The earlier in gestation, the shorter the cervix, the greater is the risk of PTB. Rate of cervical change or progressive shortening of the cervix is more important than a single measurement, hence a term ‘short and shortening’ or ‘short but stable’ cervix is described. There are other morphological features like cervical canal dilatation, funneling, sludge or debris in the amniotic fluid which can be combined in support to predict the preterm delivery (Figure 2).
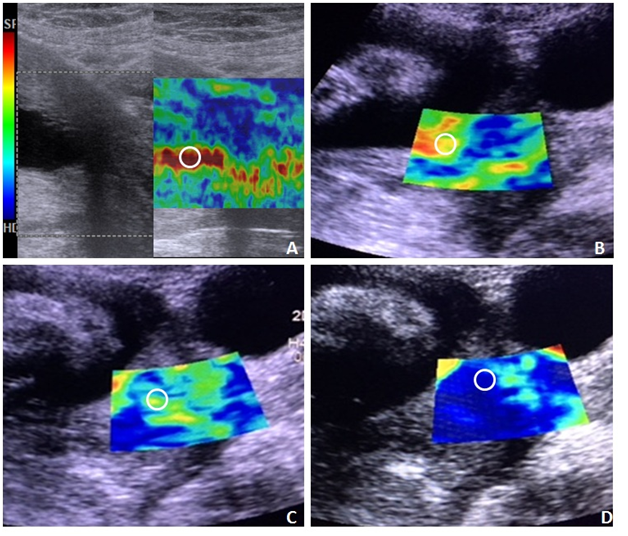
Figure 2 Elastographic images of the cervix at internal os (circles), (A) showing red -soft; (B) red and yellow-medium soft; (C) yellow and green-medium hard and (D) green and blue-hard. The color coding map is shown from the soft (SF) level to Hard level (HD) attached to the image A.
Cervical elastography
Elastography is an USG based imaging technique for assessment of the consistency of the cervical tissue/internal os. It is method of virtual palpation based on the concept of greater compression of the softer tissue on pressure as compared to the harder tissue. The gradient of the strain produced is displayed on color coded and a gray scale map. eSie Touch EI method is provided in Acuson S2000 USG (Siemens Healthcare, Erlangen, Germany) system which generates both gray scale and color coded maps across the soft to hard tissue consistency without application of pressure on the cervix. Most of the studies done previously have stressed on the assessment of the color coding of the region of the internal os.11‒13 Thomas et al.14 has mentioned the grading based on the color map,14 with red indicating soft, yellow (medium soft), green (medium hard) and blue or purple (hard). The grading was done on proportion of the colors on the color map. However, the cervical softening and prediction of the preterm is primarily based on red to yellow colors.11 Cervical elastography is done in the second trimester of gestation on patients presenting with clinical signs and symptoms of preterm labor and preterm premature rupture of membranes (PPROM) for the morphological assessment of the cervix. However, this Real Time Elastography (RTE) method is subjected to inter as well as intra observer variation; hence lacks standardization. Bishop’s scoring, cervical length and RTE of the cervix can be correlated for the assessment of the risk of preterm birth (Figure 3).
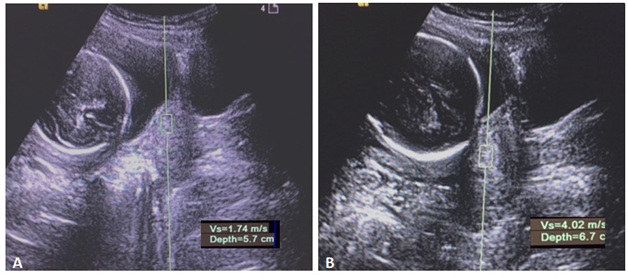
Figure 3 Shear wave elastography of the cervix. (A) Shear wave velocity is reduced indicating soft cervix. (B) increased velocity indicating the hard cervix.
Another recent advancement in the elastographic technique is based on Acoustic Radiation Force Impulse (ARFI) which is a quantitative method for measuring the velocity of the shear waves from the tissue concerned. The technique is better known as Virtual Touch tissue Quantification (VTQ). In this model, the region of interest (ROI) is placed at the concerned site (internal os in this scenario) and the velocity is measured as m/sec.
ARFI ultrasound imaging is currently used for evaluation of tissue elasticity in the liver, pancreas, breast, thyroid and prostate.15,16 The technique is previously utilized in the cases of cervical malignancy17 and there is reasonable dearth of the literature regarding its role in assessment of preterm birth. The ROI box measures 6x10mm with tissue within 80mm depth from the skin surface. Hence, some of the cases with deeper internal os and some with motion artifacts needs to excluded. The study can be extended for standardization of the elastography based on quantified results and lack of observer variability. Hence an average VTQ value in m/sec can be defined for the soft and hard cervix.
Fetal adrenal gland biometry: Fetal adrenal gland is an important but less studied subject for the prediction of the PTB. There is a cross-talk in between the fetal adrenal gland and placental endocrine pathways which are crucial for induction of labor. Fetal hypothalamic-pituitary-adrenal axis (HPA) is activated in response to fetal stress which leads to perpetuation of hormonal based signaling pathway in the form of fetal adrenal enlargement,18 secretion of fetal cortisol, more placenta mediated conversion of the sterols into estrogens, increased placental Corticotropin-Releasing Hormone (CRH) and subsequently Prostaglandins (PGE2 & PGF2α).19,20 This pathway ultimately leads to induction of premature parturition and labor, hence can be correlated with central role of Fetal adrenal gland in prediction of PTB (Figure 4).
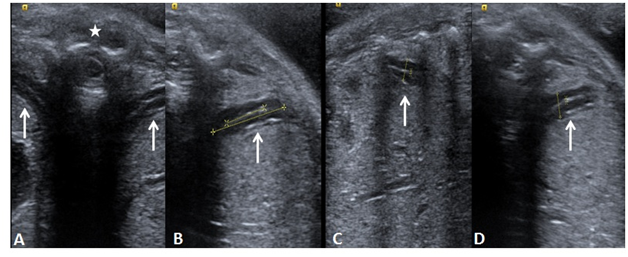
Figure 4 Magnified view of Ultrasound images of the fetal adrenal gland, (white arrows) in all three orthogonal planes, showing measurements of the fetal zone and corresponding widest dimension. (A) both adrenal glands in transaxial plane; (B) adrenal gland length; (C) adrenal gland width and (D) adrenal gland depth in Anterio-posterior axis. Asterisk (*) shows spine in the midline.
The Fetal adrenal gland is divided into 4 zones in the fetal life from inside to outside. They are “Fetal Zone” (FZ), “Transitional Zone” (TZ), “Definitive Zone” (DZ) and finally “fetal adrenal capsule” (C).21 Activation of HPA axis leads to Fetal Zone Enlargement (FZE) and secretion of Dehydroepinadrosterone-Sulfate (DHEA-S). USG can identify the central Fetal zone as hyperechoic area and the length, width and depth of the FZ can be measured and divided by their respective widest dimensions (l/L; w/W and d/D) giving ratio or percentages of the Fetal zone. Similarly, 2D & 3D volumetric assessment of the gland is also noted and divided by the estimated fetal weight giving corrected Adrenal gland volume (cAGV, in mm3/kg).
Assessment of the fetal zone can be done in symptomatic patients for calculation of the cAGV and % of the fetal zone (likely the depth d/D; in coronal plane). The studies have found significant correlation of cAGV and d/D of the gland with increased risk of the PTB.19,22 These two parameters have been found superior to the cervical length measurement in prediction of time to delivery. Two-dimensional measurement of the depth of the adrenal fetal zone offers the potential to accurately predict PTB within 7days and is independent of the clinical signs and symptoms. The study by Turan et al.22 have given the predictive values for identification of the women at risk of PTB viz. cAGV>420mm3/kg and FZE (d/D)>49.7% which have shown 81% and 100% sensitivity respectively with corresponding >85% specificity.
Ultrasonography is still developing in the field of preterm birth prediction and is providing a whole spectrum of reliable as well as quantitative markers, which can be utilized by the obstetrician and correlated with their clinical assessment. Cervical elastography is an advance application of USG and this combined with fetal adrenal biometry, requires standardization by multiple studies. However, the progression rests with a combined and complementary approach of a radiologist and an obstetrician to reach a fruitful outcome.
None.
Author declares that there is no conflict of interest.

©2017 Agarwal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.