International Journal of
eISSN: 2574-8084


Case Report Volume 9 Issue 4
Hospital Municipal de Agudos Dr. Leónidas Lucero, Argentina
Correspondence: Dra. Paula Verónica Gómez Fredes, Hospital Municipal de Agudos Dr. Leónidas Lucero, Bahía Blanca, Buenos Aires, Jose Hernandez 625. Bahia Blanca (8000) Bs As. Argentina, Tel +54 9 291 5770793
Received: September 20, 2022 | Published: November 1, 2022
Citation: Fredes PVG. Retroperitoneal fibrosis - case report. Int J Radiol Radiat Ther. 2022;9(4):138-139. DOI: 10.15406/ijrrt.2022.09.00337
Retroperitoneal fibrosis (RPF) is a rare entity that consists of chronic, non-specific inflammation of the retroperitoneum with proliferation of fibrotic tissue surrounding the aorta, inferior vena cava, iliac vessels, and generally encompasses and compresses the ureters.
It can be primary idiopathic or secondary to drugs, neoplasms, previous radiotherapy among others.
The average age of onset is between 40 and 70 years with a slight male predominance.
The clinical manifestations are non-specific, so it is frequently diagnosed in advanced stages. The initial symptoms consist of low back pain, asthenia, weight loss, arterial hypertension and in advanced stages obstructive renal failure is associated.
MDCT (multidetector computed tomography) is the first line diagnostic method where it is possible to evaluate the extension of the fibrous mass as well as the involvement of adjacent structures, detect hydronephrosis or secondary causes.
Keywords: Retroperitoneal fibrosis, retroperitoneum, renal failure, hydronephrosis
MDCT, multidetector computed tomography; RPF, retroperitoneal fibrosis; HT, hypertension; AF, atrial fibrillation
Retroperitoneal fibrosis is a rare disease characterized by the formation of chronic fibrous tissue surrounding the infrarenal portion of the abdominal aorta, inferior vena cava, iliac vessels, ureters and sometimes it can extend to the pelvis or mediastinum.
Pathophysiologically, its origin could be induced by an autoimmune reaction against an antigen present in the aorta.
It occurs idiopathically or secondary to other processes such as neoplasms, metastasis, previous surgeries, post-radiation therapy, retroperitoneal hematomas, etc.
Diagnosis is difficult and often delayed because it is an incidental and non-specific condition. Imaging studies such as ultrasound, tomography and MRI provide the necessary data, being MDCT the non-invasive method of choice allowing to assess morphology, location and extent of the PRF as well as organ and vascular structures involvement, it is also useful to detect secondary causes.
In patients admitted with renal failure due to obstructive uropathy, MDCT with intravenous contrast cannot be performed, in these cases the finding consists of a well-defined but irregular periaortic soft tissue mass with attenuation similar to that of the psoas muscle.
In cases that can be evaluated with intravenous contrast, such enhancement correlates with the activity of the fibrotic process, being marked in acute stages and almost null in advanced disease. This behavior is also useful to evaluate the response to treatment.
Corticosteroids are the most commonly used therapy with progressive decrease of corticosteroids. In severe cases or in the face of resistance to corticosteroids, other therapies with immunomodulators are used and sometimes it is necessary to resort to surgical interventions for the management of complications.
There is controversy in the literature regarding the use of biopsy for diagnosis, many argue that the response to medical treatment should be evaluated and biopsy should be left for those cases of resistance or progression of the disease.
We present the case of a 69-year-old female patient who consulted for diffuse abdominal pain and general malaise with asthenia of 10 days of evolution. Her pathological history included hypertension, hypothyroidism, AF (atrial fibrillation) and treatment with Dabigatran.
An abdominal ultrasound was requested on admission showing bilateral pyelocaliceal dilatation type II/IV and laboratory values showing renal insufficiency.
A non-contrast MDCT scan was indicated, showing a retroperitoneal periaortic image with soft tissue density, 53 x 8 mm, with irregular margins, surrounding and enveloping the aorta and inferior vena cava, also involving both ureters in the proximal third.
Treatment was started with dexamethasone 8 mg every 8 hours.
He evolved with oliguria, so it was decided to place a left double J catheter. As diuresis was not observed after 2 hours and in view of the possibility of requiring a surgical procedure, a hemodialysis session was performed to achieve Dabigatran clearance, due to risk of hemorrhage.
He evolved with spontaneous diuresis and increased diuretic rhythm, but intercurred with E.Colli bacteremia with origin in urinary focus, so treatment with trimethoprim-sulfamethoxazole was started.
MDCT with contrast was performed, which reported a slight decrease in the retroperitoneal image (Figure 1 and 2), so it was decided to continue with corticosteroid treatment and outpatient follow-up to schedule surgery with biopsy.
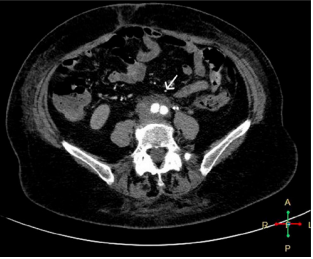
Figure 1 MDCT with intravenous contrast, arterial phase, axial view. There is evidence of dense soft tissue formation surrounding both iliac arteries.
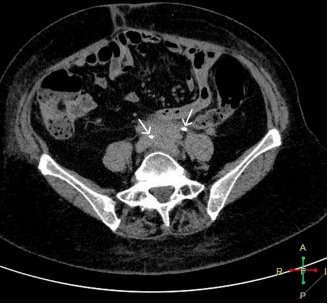
Figure 2 MDCT with intravenous contrast, excretory phase, axial view. There is soft tissue dense formation encompassing both ureters.
The patient's laboratory values improved notably and a new MDCT of the abdomen and pelvis with intravenous contrast was performed 3 months after hospital discharge, where the retroperitoneal image described above was no longer evident (Figure 3 and 4).1-8
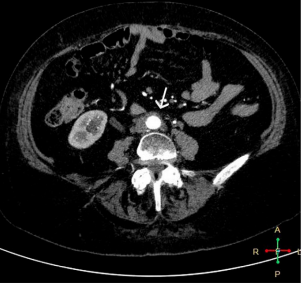
Figure 3 MDCT with intravenous contrast, arterial phase, axial view. There is evidence of free retroperitoneum without formation, aorta with contrast.
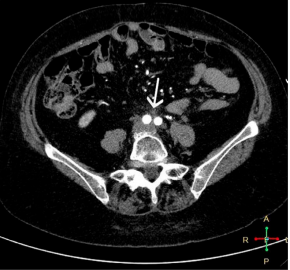
Figure 4 MDCT with intravenous contrast, arterial phase, axial view. Aortic bifurcation is recognized, with slight rarefaction of the retroperitoneal fat.
One year after this hospitalization she underwent check-ups and was diagnosed with rheumatoid arthritis.
Retroperitoneal fibrosis is a pathology that requires multidisciplinary management: nephrologists, rheumatologists, urologists, surgeons, pathologists, radiologists, with the aim of achieving early diagnosis and timely treatment to avoid or reduce potentially irreversible complications.
As mentioned in this article, diagnosis is difficult due to the insidious presentation and non-specific symptoms. Therefore, the urologist should consider this pathology when evaluating patients with low back pain and hydronephrosis.
The differential diagnosis should be made with lymphoma, sarcomas, metastatic adenopathies, retroperitoneal tumors, retroperitoneal amyloidosis, acute retroperitoneal hematomas, infections (TBC).
Glucocorticoids are the first line of medical management since they have demonstrated a favorable response and remission in 75 to 90% of patients.
Since idiopathic retroperitoneal fibrosis has been described as being able to recur, patients should continue to be followed once steroid or immunosuppressive treatment is discontinued. Relapses can occur even several years after the patient has been symptom-free.
To the entire medical clinic ward and the diagnostic imaging service of the Dr. Leónicas Lucero acute municipal hospital of Bahía Blanca, Buenos Aires, Argentina.
There are no conflicts of interest.

©2022 Fredes. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.