International Journal of
eISSN: 2574-8084


Case Report Volume 6 Issue 4
1GenesisCare, Department of Radiation Oncology, St Vincent’s Hospital, Australia
2Department of Dermatology, Melanoma Institute Australia, Australia
3Drummoyne Dermatology, Australia
Correspondence: Gerald B Fogarty, Director, Department of Radiation Oncology, St. Vincents Hospital, 438 Victoria St, Darlinghurst NSW 2010, Australia, Tel +61 2 83025400
Received: July 17, 2019 | Published: July 29, 2019
Citation: Fogarty GB, Ziebell A, Nicholls S, et al. Radiation therapy with superficial x-rays results in long term control and less epilation than megavoltage electron therapy for forehead Bowen’s disease. Int J Radiol Radiat Ther. 2019;6(4):131-133. DOI: 10.15406/ijrrt.2019.06.00233
Bowen’s disease is a type of squamous cell carcinoma (SCC) in situ of the skin usually characterized by slow-growing, red and scaly patches of skin. Bowen’s disease can be symptomatic and can progress to invasive SCC causing morbidity and even mortality. Despite previous treatment, we present a case of worsening Bowen’s disease in a functionally and cosmetically sensitive area. Successive treatments with cryotherapy, photodynamic therapy and a ten-week course of bi-daily local application of 5% fluorouracil cream failed. Two plastic surgeons declined to operate. The patient benefitted in terms of quality of life and oncological outcomes from mapping with reflectance confocal microscopy. The dosimetric advantages of radiation therapy using superficial X-rays over megavoltage electron therapy gave less epilation during treatment. Maintaining hair was important as the patient had a public profile and the hair provided a long fringe that covered the area of Bowen’s disease. The superficial X-ray machine used also facilitated set up. Three years after treatment, there was no sign of disease, nor of any hair loss and cosmesis was excellent.
Keywords: bowen's disease, squamous cell carcinoma, radiotherapy, skin cancer, reflectance confocal microscopy,Xstrahl®
cm, centimetre; CTV, clinical target volume; IVD, in vivo field dosimetry; Gy, gray; HVL, half value layer; MeV, megavoltage electron; mm, millimetre; RO, radiation oncologist; RT, radiotherapy, radiation therapy; RCM, reflectance confocal microscopy; RCT, randomised controlled trial; SCC, squamous cell carcinoma
Bowen’s disease (BD) is a type of squamous cell carcinoma (SCC) in situ of the skin usually characterized by slow-growing, red and scaly patches of skin. It can be symptomatic and can progress to invasive SCC causing morbidity and even mortality.1−3 Treatment methods include topicals, surgery and radiotherapy.4,5 We present here a case of BD in a functionally and cosmetically sensitive area. Reflectance confocal microscopy was used to map the affected area. In this instance, definitive radiation therapy using superficial X-rays was considered appropriate management. Treatment was delivered using an Xstrahl® machine (Xstrahl Ltd, Camberley, Surrey, UK). Quality of life and oncological outcomes benefited from the dosimetric advantages of the Xstrahl® superficial X-ray machine over megavoltage electron therapy. In particular, there was less epilation during treatment. The ability to maintain hair was important to the patient as she had a public profile and her hair provided a long fringe that covered the area of BD.
A 57-year old female had a two-year history of a visible solitary skin lesion in the central forehead that measured two centimeters (cm) with naked eye examination. Symptoms included itch and discoloration. Shave biopsy showed hyperplastic solar keratosis. Successive treatments with cryotherapy, photodynamic therapy and a ten-week course of bi-daily local application of 5% fluorouracil cream failed. Repeat biopsy 20 months after the initial biopsy showed progression to florid BD. Two plastic surgeons declined to operate due to possible functional and cosmetic issues related to tissue loss. A referral for definitive radiotherapy (RT) was made. The forehead lesion was assessed with reflectance confocal microscopy (RCM), a non-invasive instrument that evaluates skin lesions at almost histologic resolution using near infra-red laser.6 Surprisingly, this revealed a multifocal area of BD7 and its area of involvement was identified.8 RCM significantly aided the design of the RT treatment field (Figure 1).
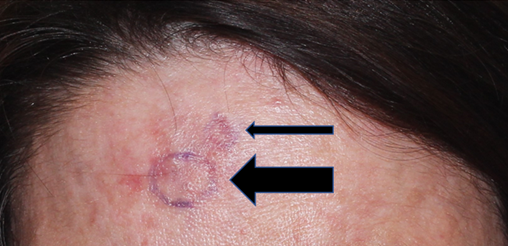
Figure 1 Reflectance confocal microscopy mapping showing multifocal areas of BD.
Thick arrow, 2cm diameter area; Thin arrow, 1cm diameter area
The prescribing radiation oncologist decided on a six-megavoltage electron (MeV) technique as this brought the added benefit of computer planning and adequate depth dose modelling. RT planning was carried out. A six cm circle applicator that enclosed the whole multifocal area was constructed (Figure 2).9 A definitive therapeutic radiation dose of 57 Gray (Gy) in 30 fractions (#s) dosed to the 90 percent isodose line was prescribed. One cm of bolus using Superflab® (Radiation Products Design Inc, Albertville MN USA) covering the whole field was necessary to achieve full dose to the skin. Routine quality assurance with in vivo film dosimetry (IVD) within the first week of RT, recorded on the skin in the middle of the field, confirmed that the planned dose was being delivered. Treatment continued.
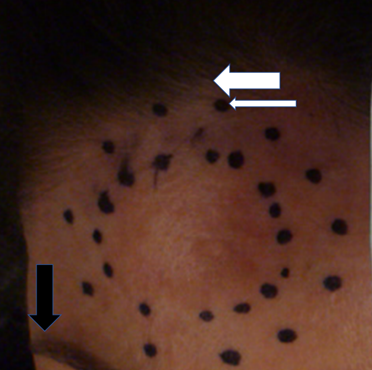
Figure 2 Clinical RT planning marks. The inside dotted line encompasses the BD regarded as positive on RCM. This is the clinical target volume (CTV).9 The outer dotted line, marked with the thin white arrow, is a one cm expansion on the CTV, demonstrating the planned electron field edge. The anterior hair line or fringe is marked with a thick white arrow. The lateral eyebrow is marked with a vertical thick black arrow.
After delivering 28.5 Gy in 15#s, the patient noted the beginning of hair loss from the fringe immediately above the RT field. This hair was important as the patient had a public profile and it provided a long fringe that covered the area of BD. The hair loss was probably due to the electron field edge being close to the hair line as well as other issues with electrons. A treatment break was unacceptable on clinical radiobiological grounds. The patient was immediately swapped to superficial X-ray treatment using an Xstrahl® machine (Xstrahl Ltd, Camberley, Surrey, UK), enabling her to continue therapy the following day when the next fraction was due. Due to better collimation of the radiation beam with superficial X-rays, a five cm applicator could be used to cover the same CTV rather than six cm. The beam quality was chosen using filter 2, with a generating energy of 80kV and a half value layer (HVL) of 2.5 mm of aluminum delivered with 30 cm focus to source distance. Hair loss ceased during the rest of treatment and treatment was completed as prescribed in the same time frame. Three years later, the patient had no sign of disease, nor any hair loss, and she maintained excellent cosmesis.
Bowen’s disease (BD) can be symptomatic and can progress to invasive SCC causing morbidity and even mortality.1−3 BD can be extensive in functionally and cosmetically sensitive areas (e.g. face) so that surgery, which involves tissue loss, can be challenging. BD can represent as a field change called skin field cancerisation (SFC),10 and the preference is to treat all the field4 to avoid future lesions arising in the untreated part of the field. In a recent randomised trial comparing topical therapies, fluorouracil was found to be the best topical treatment.4 It is usually an excellent, easy to use and economical option offering a high cure rate and the ability to treat the clinical area and wide margins with a good cosmetic outcome.5 The lesion in this case, however, was so clinically thick and hyperkeratotic that fluorouracil was unable to be sufficiently absorbed and so it failed. This led to the need for other cosmetically viable treatment options to be sought. Like topical therapies, RT provides tissue conservation,11 but there are no published randomised controlled trials of RT in BD, despite it being common knowledge that definitive RT results in high rates of in-field control12 with minimal morbidity.
Epilation is a major quality of life concern with RT.13 Hair follicles extend to a maximum of 4.5 mm in the human scalp.14 To avoid hair follicle death, the dose of radiation superficial to a depth of five mm needs to be kept under 2 Gy in four fractions to avoid temporary alopecia15 and under 16 Gy in 2 Gy fractions with fractionated therapy to avoid radiation-induced alopecia.16 Care needs to be taken in planning, not only to make sure that all the SFC is treated, but also to minimise the exposure of normal tissue to radiation. The megavoltage electron technique resulted in unacceptable epilation. Electrons require bolus and have an unpredictable belling of the penumbra under the skin.17 This creates uncertainty as to what is the exact dose to hair follicle at depth, despite a reassuring surface IVD result. The superficial X-ray beam produced by the Xstrahl® machine is more highly collimated. It gave a tighter penumbra with less belling into the normal hair bearing tissue. Other advantages over MeV treatment also include a shorter beam time of 1.27 minutes per fraction and less time for RT set up as no bolus is needed. A stabilisation mask is also not required, making overall treatment time quicker and more acceptable, especially for patients who suffer from claustrophobia. Due to ease of planning and delivery, superficial X-ray treatment was able to be deployed immediately. This avoided any radiobiological issue arising from a break in therapy that may have been necessary had a technique with more complex planning (e.g. a brachytherapy mould), been required. The use of superficial X-ray therapy was able to deliver the best outcome for this case.
This case of Bowen’s disease in a functionally and cosmetically sensitive area demonstrated quality of life and oncological benefits from mapping with reflectance confocal microscopy and from the dosimetric advantages of the Xstrahl® superficial X-ray machine over megavoltage electron therapy. Three years after treatment, there was no sign of disease, nor any hair loss, and the patient maintained excellent cosmesis.
None.
Nill.
The authors would like to thank Aileen Eiszele from A&L Medical Communications for editorial review and for overseeing the submission and acceptance process.
The authors have no conflicts of interest to declare.

©2019 Fogarty, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.