International Journal of
eISSN: 2574-8084


Research Article Volume 10 Issue 6
Department of maxillo-facial Surgery, School of Medicine, University of Marrakech, Morocco
Correspondence: Zahira Benzenzoum, Department of maxillo-facial Surgery, School of Medicine, University of Marrakech, Morocco
Received: December 15, 2023 | Published: December 29, 2023
Citation: Benzenzoum Z. Place of surgery in the treatment of plexiform nevroma of the face plexiform nevroma of the face: about 09 cases of von recklinghausen disease. Int J Radiol Radiat Ther. 2023;10(6):150-154. DOI: 10.15406/ijrrt.2023.10.00372
Neurofibromatosis 1 (NF1) is the most common neurofibromatosis. It’s a genetic disorder defined by the development of heterogeneous nerve tumors, neurofibromas. 40% of NF1 are revealed by a facial damage. The aim of our work is to present the current knowledge of NF1 and report, from the analysis of clinical cases, surgical indications of plexiform neurofibroma. This is a retrospective study conducted at the department of maxillofacial and aesthetic surgery CHU Mohammed VI Marrakech. Our study included 9 patients with plexiform neurofibroma of the face. The average age was 26.5 years (15 to 36 years). The sex ratio M / F was 1.The neurofibroma was unilateral in all patients. Dysplasia of the sphenoid greater wing was found in 2 patients, causing in a patient a cranial orbit, meningo-encephalocele and pulsatile exophthalmos. 6 patients were operated. And 2 refused. Surgery was iterative with an average of two interventions, and it was to reduce the tumor volume. The aesthetic result was satisfactory and allowed a rehabilitation of patients. There was a recurrence in a patient with a decline of 3 years. Surgery has an important place in the treatment of plexiform neuroma of the face. Its purpose is twofold, aesthetic and functional. It is only palliative because it does not change the evolution of the disease. Two problems arise during surgery: hemorrhagic and invasive nature of these tumors. The resections are often incomplete and intra-tumoral. There is no standardization of the timing and importance of surgery to effector especially in children. The degeneration of neurofibroma in neurofibrosarcoma is a rare but dangerous
Keywords: neurofibromatosis 1, plexiform neurofibroma, face, treatment, surgery
Neurofibromatosis 1 or Recklinghausen's disease (NF1, MIM 162200) has been known for over a century, thanks to Von Recklinghausen's original observation (1882) which gave it its name. It is a frequent genetic disorder affecting between 1/4000 and 1/3000 individuals, with a homogeneous worldwide distribution and an estimated incidence of 1/2500 births.1
It is an autosomal dominant disorder, with almost complete penetrance by the age of eight. It is the most common neurofibromatosis, characterized by skin manifestations such as café-au-lait stains, lentigines and neurofibromas, which may be associated with other manifestations such as maxillofacial, ocular, bone and gastrointestinal involvement.2
The great variability of clinical expression, the risk of tumors and the totally unpredictable course of the disease mean that neurofibromatosis sufferers need regular follow-up and multidisciplinary management.3
Since the 1988 National Institute of Health (NIH) consensus conference, neurofibromatosis, an entity that encompasses several manifestations, has included at least two well-identified diseases, NF1 and NF2. Diagnostic criteria have also been established for both conditions. A patient is a carrier of NF1 if he or she has at least two of these diagnostic criteria. The validity of the diagnostic criteria has been confirmed by molecular biology.4
Its morbidity and mortality are linked to the occurrence of multi-systemic complications, brain tumors, malignant nerve sheath tumors and vasculopathies,4 vital and functional prognosis.
We conducted a retrospective study of 9 patients with plexiform neurofibromas of the face, followed and managed at the Maxillofacial and Aesthetic Surgery Department of Ibn Tofail Hospital, CHU Mohamed VI of Marrakech over a period of 6 years.ci-joint un tableau résumant les caractéristiques des 09 malades reçus et pris en charge dans notre formation.
Neurofibromatosis 1 or Recklinghausen's disease is a frequent genetic disorder affecting 1/4000 to 1/3000 individuals with a homogeneous worldwide distribution and an estimated incidence of 1/2500 births.1
It is an autosomal dominant disorder, with almost complete penetrance by the age of eight. The NF1 gene responsible for the disease is located on the long arm of chromosome 17 at 17q11.2.
NF1 is characterized by great variability in clinical expression, even within the same family.
In most cases, a clinical examination by a physician familiar with the disease is sufficient to make the diagnosis. The great variability of clinical expression, the risk of tumors and the totally unpredictable evolution of the disease mean that NF1 subjects must be followed up regularly.
The consensus conference of the National Institute of Health in Bethesda (USA) specified seven cardinal criteria for the diagnosis of NF1 (Table 1). The diagnosis of NF1 is made if two of these signs are present in the same individual.5
In adults, NF1 is usually easily diagnosed on the basis of clinical examination. In children, however, café-au-lait spots (TCL) may remain the only sign for a long time, and in the absence of a family history of NF1, the diagnosis is sometimes left open.6
Some authors believe that characteristic signs such as TCL, iris hamartomas and benign neurofibromas are always present.7
Neurofibromas of the face are often associated with other orbitofacial.4 and extrafacial manifestations,4,8 which must be investigated to establish the diagnosis of NF1.
Clinically, damage can be classified into 2 categories: cardinal signs and complications. (Tables 2-4)
|
An affected first-degree relative (parent, sibling or child). At least 6 cafe-au-lait spots (TCLs) Axillary or inguinal freckles Or Optic nerve glioma
At least 2 Lisch nodules (iris hamartoma) A characteristic bone lesion |
> 1.5 cm after puberty > 0.5 cm before puberty At least two neurofibromas regardless of type At least one neurofibroma Plexiforme Pseudarthrosis Sphenoid dysplasia Thinning of the cortex of the long bones
|
Table 2 NF1 diagnostic criteria - Consensus Conference on Neurofibromatosis (NIH - Bethesda, 1988).5
|
|
Frequency age (In %) |
|
|
Skin Coffee and milk stains Freckles Cutaneous neurofibromas Neurofibromes nodulaires Neurofibromes plexiformes El Nodules de Lisch Optic glioma Symptomatic gliomas Skeleton Sphenoid dysplasia Pseudarthrosis Scoliosis requiring surgery |
99 to 100 50 to 80 100 15 to 24 30 to 39
67 to 82 15 2 to 4
3 to 4 3 to 4 2 to 4.4 |
< 5 years < 6 years < 30 years Childhood, adult < 5 years
> 6 years Early childhood
Childhood Childhood Childhood, adolescence |
Table 3 Frequency of different neurofibromatosis 1 diagnostic criteria according to mean age of onset.
|
Complications |
% |
Age |
|
|
Skin |
|
|
Neurofibrome plexiforme Juvenile xanthogranuloma
|
30 to 39 Tto2. |
<5 years childhood |
|
|
Cell |
|
|
Optic pathway glioma sympromatique |
15 2 to 4 |
Early childhood
|
|
|
Skeleton |
|
|
Pseudarthrosis 3to4 Scoliosis requiring the 2 to 4.4 surgery |
|
Childhood Childhood, adolescence |
|
|
The nervous system |
|
|
Learning difficulties 33 to 70 Epilepsy 6 to7 Hydrocephalus 1.5 to 2.6 |
|
Childhood Childhood childhood |
|
|
Cancers |
|
|
MPNSTs Leukemias Carcinoid tumor |
3 to 4 <0.1 0.6 to 1.5 |
Adolescence, adult |
|
High blood pressure Phéochromocytome Renal artery stenosis |
5 <1 1 |
Adult Adult Childhood, adolescence |
Table 4 Frequency of complications requiring follow-up in NF1 patients according to age.4
Symptomatology evolves with age, and disease penetrance is almost complete by the age of eight (Table 2).9
In 1988, an NIH consensus conference determined the diagnostic criteria for NF1. Affected individuals present with at least two of the following criteria.4,10,11
In our series, the patients consulted were adults, and their reason for consultation was the highly suggestive giant soft-tissue mass; the simple observation of TCL was sufficient to evoke the diagnosis of NF1 according to NIH criteria.
Imaging is used to assess lesions: standard X-rays highlight bone involvement; CT and MRI scans clarify the extent of lesions and their relationships, and look for central involvement.
Ophthalmological examination remains fundamental to the therapeutic management of Von Recklinghausen disease.
Determining persistent visual acuity in the damaged eye has implications for the reconstruction strategy. In addition, it enables the detection of synchronous optic tract tumors such as gliomas or meningiomas.
All our patients underwent a preoperative ophthalmological examination.
Treatment of NF1 continues to be symptomatic, with several drugs tried in phase I and II studies, such as antihistamines, retinoic acid, anti-angiogenetic agents, farnesyl transferase inhibitors and cytokine modulators, such as Pirfenidone.12
Radiotherapy and chemotherapy have no indication in benign lesions, and are only marginally effective in cases of degeneration.11,13 In addition, untimely radiotherapy can lead to malignant degeneration.10,14
Surgery is of prime importance, as there is no other treatment, either preventive or curative, for the disease.11 This surgery is only palliative, as it in no way alters the overall course of the disease.11,15-17
Plexiform neuroma is a special case, as its tumoral excision is conditioned by its benign nature, ineluctable recurrence, significant intraoperative hemorrhage, the fact that its surgery must not be mutilating, either aesthetically or functionally, and its topography.
In principle, exeresis is complete if it respects these imperatives, without risk, otherwise intra-lesional exeresis is accepted by the majority of authors.
It is currently assured that surgery does not entail any risk of malignant transformation. Surgical excision is not without its difficulties. The tumour is often highly haemorrhagic, sometimes leading to operative mortality.10,18 19,20
With regard to the age of surgical management, we were not faced with the problem of choosing the right time for treatment, since all our patients consulted us at an adult age. This is in line with studies carried out by Abouchadi et al, Needle mn et al.10,21 Unlike some authors who recommend early intervention before the onset of major deformities to avoid morphological or functional repercussions (amblyopia).
It is often necessary to complete tumour removal with the cure of a frontotemporal meningoencephalocele and repair of the loss of bone substance of the greater wing of the sphenoid and the roof of the orbit with an appropriate plasty using either the external table of the cranial vault, an iliac graft or a titanium plate.10,19,22,23
Incomplete excision of the neurofibroma exposes the patient to the risk of recurrence, hence the importance of iterative, modelling, non-mutilating surgery, given the benign nature of neurofibromas, on the one hand, and their haemorrhagic and infiltrative nature, on the other.22-25
Malignant degeneration is a rare but formidable complication of NF 1.11 Also called malignant schwannoma, erogenous sarcoma, or MPNSTs, it is an exceptional tumor in the general population, with a minimal risk estimated at 0.001%.26 In our series, we observed malignant transformation in one case, confirmed by anatomopathological study of the resection specimen.
However, in the literature, the incidence of malignant transformation in NF1 patients ranges from 5% to 8%.1,14 At present, it seems that this degeneration occurs spontaneously in initially benign tumours, without any surgical factor.
Patients with NF1 and plexiform neurofibromas must therefore be carefully monitored, even more so if they are numerous or extensive. However, plexiform neurofibromas can present periods of rapid growth, followed by periods of relative quiescence. Progressiveness is not synonymous with malignancy.27
Post-operative follow-up is carried out at a rhythm specific to each team, but generally at 1 month, 3 months, 6 months, 1 year, then annually, to look for recurrences, deterioration of the result or visual function. We must always bear in mind the possibility of the occurrence of NF1-related conditions such as glioma, pheochromocytoma or even MPNSTs(Figures 1-14).
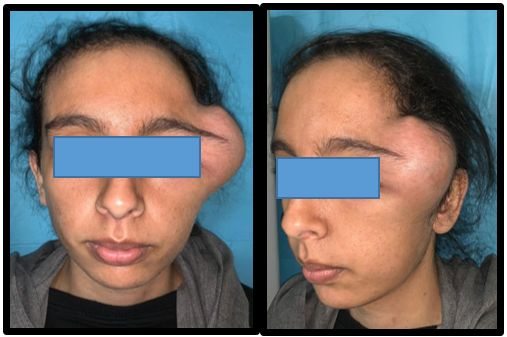
Figure 1 Front and ¾ photo of a left temporo-palpebral plexiform neuroma responsible for significant morpho-functional dis Figurement.

Figure 2 Axial section showing a rounded temporal lesion with significant enhancement after injection of PDC, extending into the deep spaces of the face without bone lysis.
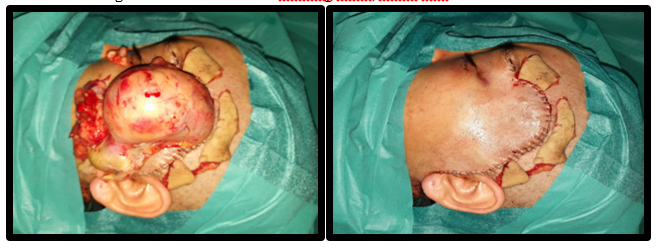
Figure 4 Intraoperative view of the surgical approach, and the tumour after excision and reduction of excess skin.
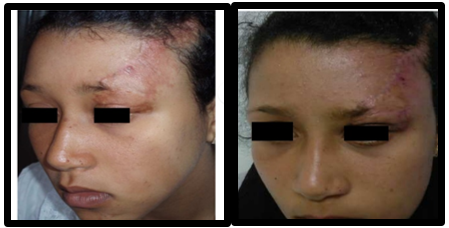
Figure 12 Pre- and post-operative appearance of a patient with a left fronto-palpebral cutaneous plexiform neuroma.
NF1 is the most common of the phacomatoses and neurofibromatoses. It can affect any region of the body, but particularly the face. The damage can be discrete or disfiguring, and may threaten visual function. This so-called benign disease presents a real local malignancy.
The expected benefits of surgery are morphological (aesthetics are paramount in these patients, who tend to shun the gaze of others and withdraw into themselves), functional (particularly in the case of eyelid involvement), psychological and social.11
Whatever the stage of the disease and the technique used, the stability of the results is controversial,26 and it is a real challenge to ensure that the results are long-lasting.
None.
Author declare there is no conflicts of interest.

©2023 Benzenzoum. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.