International Journal of
eISSN: 2574-8084


Case Report Volume 1 Issue 2
Department of Radiology, Turkey
Correspondence: Ali Koç, Department of Radiology, Kayseri Training and Education Hospital of Medicine, Kayseri, Turkey, Tel +90 506 545 6744
Received: December 12, 2016 | Published: December 30, 2016
Citation: Koç A. Osteochondroma-related distal tibiofibular synostosis with an isolated subtalar joint degeneration and flexor hallucis longus tendon entrapment. Int J Radiol Radiat Ther. 2016;1(2):43-45. DOI: 10.15406/ijrrt.2016.01.00010
Osteochondroma (exostose)-related distal tibiofibular synostosis was noticed in a 69year-old male patient with a previously known Hereditary Multiple Exostosis (HME). He had chronic complaints of right ankle pain with a hard shin swelling. Radiography, Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) exams revealed an osteochondroma-related distal tibiofibular synostosis complicated with subtalar joint arthritis and flexor hallucis longus tendon entrapment.
Keywords: osteochondroma, subtalar arthritis, synostosis
HME, hereditary multiple exostosis; CT, computed tomography; MRI, magnetic resonance ımaging; T1W, T1 weighted; T2W, T2 weighted; FOP, fibrodysplasia ossificans progressive
Osteochondroma is the most common benign tumor or tumorlike lesion of bone. The radiographic appearance is often diagnostic, that is, a lesion composed of cortical and medullary bone with a cartilage cap. These lesions may be solitary or multiple, with the latter associated with the syndrome HME. Complications are commonly associated with its exophytic nature and include cosmetic and osseous deformity, fracture, vascular compromise, neurologic sequelae, overlying bursa formation, and malignant transformation. These complications are more common in patients with multiple lesions (HME) rather than solitary osteochondromas.1 Although related complications are mostly about the exophytic nature of tumor itself, Frances H. Gannon Search for articles by this author we present a case of distal tibiofibular synostose via an osteochondroma in a HME patient that was complicated with subtalar joint degeneration and flexor hallucis longus tendon entrapment, being the first case in literature.
A 69year-old man with a known HME, admitted to orthopedia clinic for right ankle pain that was serious especially at standing position. At physical examination, he had restricted joint movements during abduction and adduction. There was a hard, fixed swelling localized superiorly to the shin, measuring 3x4x4cm. Patient was subjected to anteroposterior and lateral radiography of ankle joint. Radiography showed a well defined bony lesion superposed to the posterior aspect of distal tibiofibular metaphysis with a thin sclerotic rim and posterior edge calcification (Figure 1). There was also tibitalar tilt (valgus deformity) at AP graphy.

Figure 1 AP and lateral radiographs of ankle showing a well defined osteochondroma with a calcified cap, arising from posterior aspect of both tibia and fibula (white arrow). Cortices of tibia and fibula are indistinct at the tumor level, suggesting a synostosis (black arrows). Tibiotalar tilt is also well depicted on AP graphy.
Because of unusual localization and for showing the relation of tumor with adjacent bony and soft tissue structures, CT and MRI exams were done. At axial and 3D CT images, there was a well-bordered tumor, originated from posterior aspect of distal metaphysis of tibia and fibula, with an own cortical and medullary bone in a continuity with the natives, and presented as tibiofibular synostosis via an osteochondroma (Figure 2). Calcified cartilage cap was seen as amorphous density at CT image and, isointense with bony cortex on T1 weighted (T1W) and T2 weighted (T2W) images.
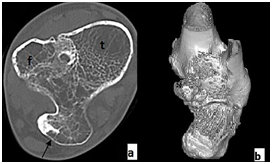
Figure 2A & B Axial (A) and 3D CT (B) images showing an osteochondroma (arrow) origined from both tibia and fibula, resulting in a synostosis. T, tibia, f, fibula.
MRI also revealed subtalar degeneration as narrowing of the joint space, subchondral trabecular edema, and cystic changes on sagittal images (Figure 3). Flexor hallucis longus tendon was displaced and entrapped by the exophytic tumor (Figure 4).
Osteochondromas around the ankle are very uncommon except in cases of Multiple Hereditary Exostoses.2 A small amount of these tumors leads to synostosis. Distal tibiofibular synostosis is usually acquired and mostly secondary to trauma. Iatrogenic causes following syndesmotic procedures or predisposing conditions like subperiosteal haemorrhage, fluorosis, fibrodysplasia ossificans progressive (FOP), and kissing osteochondroma were also reported.3 There are very few case reports of congenital distal tibiofibular synostosis.4
Common osseous deformities around the ankle in HME were reported as tibiotalar tilt (valgus deformity), significant limb length discrepancy, and short stature.1 In our case, tumor was origined from both distal tibia and fibula. Synostosis via the tumor was noticed at AP graphy with a finding of tibiofibular cortical discontinuity at the level of opposing faces. Because of both tibia and fibula involvement, bowing deformity was not found which necessitates asymmetrical force.
Valgus deformity can be attributed to multiple factors, including shortening of the fibula relative to the tibia. Resulting obliquity of the distal tibial epiphysis and medial subluxation of the talus also can be associated with this deformity. Partial compensation may be provided by a developmental obliquity of the superior talar articular surface.5 In our case, deformity was significant on AP graphy and coronal MR images. Lateral malleol had a broad joint surface with talar body, rather than normal. While there was no evident fibular lenght discrepancy, this situation could be explained by changes in share of participation on the distribution of load that caused by tumor-related tibiofibular fusion.
Most of the complications related with osteochondroma were attributed to its exophytic nature and neighbourliness relation. In our case, we additionally presented the synostosing nature of tumor and related complications. These complications were mainly associated with the disturbed joint biomechanics. Isolated subtalar arthritis can result from; trauma (calcaneal/talus fractures), primary talocalcaneal arthritis (instability/deformity), symptomatic residual congenital deformity (talocalcaneal coalition), posterior tibial tendon dysfunction, and inflammatory arthritis isolated to the subtalar joint.6
In this case, subtalar arthritis was associated with a synostosing osteochondroma. This can be explained with the asymmetric forces against the subtalar joint as a result of tibiotalar tilt and related restricted motion of talocrural joint. Flexor hallucis longus tendon entrapment was also an another complication of osteochondroma, which has been classically mentioned in ballet dancers7 and was reported secondary to posterior ossicles (frequently os trigonum), calcaneal, postmalleolar, and medial malleolar fractures.8
Osteochondromas may cause different clinical situations and several abnormalities according to their anatomic localization and tumoral behaviour. Osteochondroma-related distal tibiofibular synostosis can cause subtalar arthritis, tibiotalar valgus deformity and flexor hallucis longus tendon entrapment.
None.
Author declares that there is no conflict of interest.

©2016 Koç. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.