International Journal of
eISSN: 2574-8084


Case Report Volume 5 Issue 3
1Department of Radiology, University of Health Sciences Umraniye Training and Research Hospital, Turkey
2Medical Doctor of Urology Department, Uskudar State Hospital, Turkey
3Associate Professor of Radiology Department, University of Health Sciences Umraniye Training and Research Hospital, Turkey
4Professor of Radiology Department, University of Health Sciences Umraniye Training and Research Hospital, Turkey
Correspondence: Fatma Kulali, Department of Radiology, University of Health Sciences Umraniye Training and Research Hospital, Adem Yavuz street No: 1, Umraniye, 34764, Istanbul, Turkey, Tel +90 (216) 632 1818*1462, Fax +90 (216) 6327124
Received: March 15, 2018 | Published: May 24, 2018
Citation: Kulali F, Kulali SF, Semiz-Oysu A. Magnetic resonance imaging findings in bilateral multicentric testicular seminomas. Int J Radiol Radiat Ther. 2018;5(3):164-166. DOI: 10.15406/ijrrt.2018.05.00156
Seminomas are the most common testicular tumors. But, frequency of bilateral testicular seminomas is about 2-3%. Seminomas can spread and metastasize in a very short time because of short doubling time. For this reason, early diagnosis and management is essential. The tendency of multicentricity and bilateral location in lymphoma is higher than seminoma. The first line treatment of testicular lymphoma is chemotherapy. So, management is different in lymphoma and seminoma. The accurate preoperative diagnosis is important. We report a case of a 25-year-old man with bilateral multicentric testicular lesions who had not yet fathered a child and had malignant findings on magnetic resonance imaging (MRI) and diffusion weighted imaging (DWI). After surgery, histological examination revealed bilateral multicentric testicular seminomas. This case underlines the role of MRI and DWI in the management of patient.
Keywords: diffusion weighted imaging, magnetic resonance imaging, seminoma, testicular cancer
MRI, magnetic resonance imaging; DWI, diffusion weighted imaging; US, ultrasonography; FSH, follicule stimulating hormone; LH, luteinizing hormone; βHCG, beta human chorionic gonadotropin; ADC, apparent diffusion coefficient; ACTH, adrenocorticotrophin hormone
Approximately 95% of testicular tumors are germ cell tumors in young men. Seminomas account for 50% of germ cell tumors.1 But, multicentricity and bilateral locations are rarely observed in testicular lesions.2 We aimed to present magnetic resonance imaging (MRI) findings of a patient who had bilateral and multicentric seminomas and put emphasis on the added value of diffusion weighted imaging (DWI) in the diagnosis.
Twenty five-year-old man who had not yet fathered a child referred to our hospital with the compliant of left inguinal pain. Varicocele was found at physical examination. Scrotal doppler ultrasonography (US) was performed. Multiple hypoechoic lesions with irregular borders were found in bilateral testis. Mild increased vascularity was detected inside the lesions on Doppler US. Microlithiasis was also seen in bilateral testis. He had no previous history of chronic disease. Laboratory findings including follicule stimulating hormone (FSH), luteinizing hormone (LH), beta human chorionic gonadotropin (βHCG) were normal. For differential diagnosis of testicular benign and malignant tumors, contrast enhanced MRI and DWI were performed. There were multiple lesions in bilateral testis. The longest diameters of lesions were ≤1cm. The lesions had intermediate intensity on T1-weighted images and low intensity on T2-weighted images according to normal parenchyma of testis (Figure 1). They showed homogenous contrast enhancement (Figure 2). Diffusion restriction was observed on DWI (Figure 3). The mean apparent diffusion coefficient (ADC) value of lesions was 0.88±0.15x10-3mm2/s. The differential diagnosis was difficult because of multicentricity of lesions in bilateral testis (Figure 4). Due to malignant findings on MRI and DWI, the patient underwent surgery. After surgery, bilateral multicentric testicular seminomas were reported histopathologically. Patient’s informed consent to publication was taken.
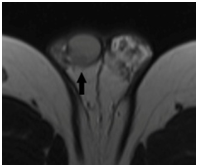
Figure 1 Seminoma in right testis (black arrow) was approximately 1 cm diameter and hypointense on axial T2-weighted image.
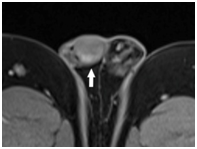
Figure 2 Seminoma in right testis (white arrow) had contrast enhancement on axial fat saturated T1-weighted image.
Testicular cancers can spread and metastasize in a very short time because of short doubling time. For this reason, early diagnosis and management is essential. The first-choice diagnostic imaging modality for testicular tumor is scrotal doppler US. Doppler US is easily achievable, low cost imaging modality with high accuracy. Scrotal Doppler US is generally sufficient for diagnosis of testicular tumor. The differential diagnosis of testicular lesions with imaging modalities is sometimes difficult. There can be overlaps between imaging findings of benign and malignant testicular lesions. The radiological findings should be evaluated together with history, physical examination and laboratory results of patient. When the differentiation of benign and malignant tumor is uncertain on scrotal Doppler US, MRI can be beneficial for the treatment planning of patient.3
Testicular seminoma is the most common testis tumor. Seminoma is usually seen between 15 and 35 years-old man. Seminomas are usually homogenous, hypoechoic lesions with internal hypervascularity on scrotal Doppler US. On MRI, they show contrast enhancement. They are generally low signal intensity on T2-weighted images according to normal testicular parenchyma.3,4 The frequency of bilateral development of seminoma is approximately 2-3%.2 The differential diagnosis of bilateral multicentric testicular lesions firstly includes lymphoma, adrenal rest and sarcoidosis.3 Lymphomas rarely occur in testis and account for approximately 1-9% of all testicular tumors. But, the tendency of multicentricity and bilateral location in lymphoma is higher than seminoma.3,5 The frequency of bilateral involvement is approximately 40% in lymphoma. Lymphoma should be kept in mind in the differential diagnosis of patients with bilateral multiple testicular tumors. Besides, lymphomas mostly occur in elderly patients (≥60 years). The most common type of testicular lymphoma is diffuse B cell non-Hodgkin lymphoma. Lymphomas usually exhibit infiltrative pattern of involvement but, can also be seen as multiple focal lesions. On scrotal doppler US, they are vascular and hypoechoic lesions with hazy margins.3,5 On MRI, they are low signal intensity on T1- and T2-weighted images. They also show low to intermediate degree of contrast enhancement.3,5
Another disease that may present as bilateral testicular involvement is testicular adrenal rest tumor. Adrenal rest tumors are associated with congenital adrenal hyperplasia, Cushing Syndrome and Addison disease which cause excess secretion of adrenocorticotrophin hormone (ACTH). On scrotal Doppler US, they are seen as bilateral hypoechoic lesions with vascularization. On MRI, lesions are intermediate signal on T1-weighted image and mildly low signal on T2-weighted images. They have homogenous contrast enhancement.3 In the diagnosis of adrenal rest tumors, the history of patient is essential. Sarcoidosis is a chronic granulomatous disease. The genital organ lesions of sarcoidosis can occur in 5% of patients with pulmonary involvement. On MRI, they are contrast enhanced, multiple nodular lesions with low signal intensity on T2-weighted images. The epididymal involvement is often seen in sarcoidosis patients with testicular lesions.3
The diagnosis of some testicular lesions cannot be easy. MRI can be problem solving modality for differential diagnosis of benign and malignant lesions. As a supportive imaging, DWI can be used.6 DWI can be helpful in the differentiation of benign and malignant lesions. DWI shows the randomized movement of water. ADC map is performed automatically from DWI. ADC map provides us to estimate the diffusion property of tissue with quantitative measurements. Increased cellularity in the tissue restricts the movement of water and also diffusion of tissue. The high signal intensity on DWI with low signal intensity on ADC map shows restricted diffusion. The ADC value is inversely associated with tissue cellularity.6 In previous studies, significant difference between ADC values of malignant and benign testicular lesions was found.6,7 For prediction of malignant testicular lesion at a cut off ADC value of ≤0.99, the sensitivity, specificity, positive predictive value, and negative predictive value was 93.3%, 90%, 87.5%, and 94%, respectively.6 In another study with a small sample size (n=26), the optimal cut off ADC value was calculated as 0.68x10-3mm2/s for differentiating of seminomas from non-seminomatous germ cell tumors.7 The mean ADC values of seminomas was found significantly lower than non-seminomatous germ cell tumors (0.59±0.009 versus 0.90±0.33, p=0.01).7 Therefore, ADC calculation is important in differentiation of testicular lesions and MRI combined with DWI improves diagnostic accuracy.
In conclusion, to the best of our knowledge, this is the first report to present MRI and DWI findings of bilateral multicentric testicular seminomas. So, seminomas also should be mind in differential diagnosis of multiple lesions in bilateral testis. Because of infertility, the decision of surgery is hard in some patients especially with bilateral multiple testicular lesions. The accurate diagnosis is necessary. Contrast enhanced MRI combined with DWI can be required for accurate diagnosis and planning of surgery in some testicular lesions.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The author declares that there is no conflict of interest

©2018 Kulali, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.