International Journal of
eISSN: 2574-8084


Case Report Volume 9 Issue 1
1Radiology, WEBIMAGEM Telerradiologia, Brazil
2Radiology, Irmandade da Santos Casa da Misericórdia de Campo Grande, Brazil
Correspondence: Márcio Luís Duarte, WEBIMAGEM Telerradiologia, Avenida Marquês de São Vicente 446, São Paulo, São Paulo, Brazil., Tel 55xx13981112799
Received: February 12, 2022 | Published: March 7, 2022
Citation: Duarte ML, Abreu BFBB, Lopes DT, et al. Isolated posterior malleolus fracture - magnetic resonance imaging diagnosis. Int J Radiol Radiat Ther. 2022;9(1):35-36 DOI: 10.15406/ijrrt.2022.09.00321
Approximately 7% to 44% of ankle fractures involve the posterior tibial margin. These fractures tend to have a poorer prognosis than fractures without posterior involvement. Recognition of posterior malleolar fracture patterns is more important than fracture fragment size in decision making. Standard ankle radiographs are not effective for diagnosing isolated posterior malleolar fractures. There is consensus that the true size and geometry of the fragment, specifically its medial propagation, and intercalary fragments may be diagnosed only by computed tomography scanning. Magnetic resonance imaging may yield additional information about syndesmotic ligaments, tendons and osteochondral lesions, although it is used only exceptionally. There are controversies about the treatment of these fractures but authors agree that small fragments can be treated conservatively whereas larger fractures that involve more than 25% of articular surface should be fixed to avoid instability and degenerative changes. The authors report a case with a magnetic resonance imaging diagnosis of this fracture.
Keywords: magnetic resonance imaging, tibial fractures, ankle
The posterior tibial margin fractures represent about 7% to 44% of ankle fractures and tend to have a poorer prognosis than fractures without posterior involvement.1 The posterior malleolus fracture happens in approximately 46 % of type Weber B or C ankle fracture-dislocations.2
It is classified into 3 types based on their morphology by Haraguchi and colleagues:1,3,4
A 43-year-old woman with right ankle pain after falling down the stairs three months ago, with progressive worsening. Refers to cast immobilization for 02 days following the injury, removing it on the third day.
She has normal right ankle radiography. Magnetic resonance imaging (MRI) demonstrated a posterior malleolus fracture, type 1 of Haraguchi classification (Figures 1 & 2), with a partial tear of the anterior talofibular and anterior tibiofibular ligaments (Figure 2). The patient underwent surgical treatment with an improvement in the condition and was discharged six months later.
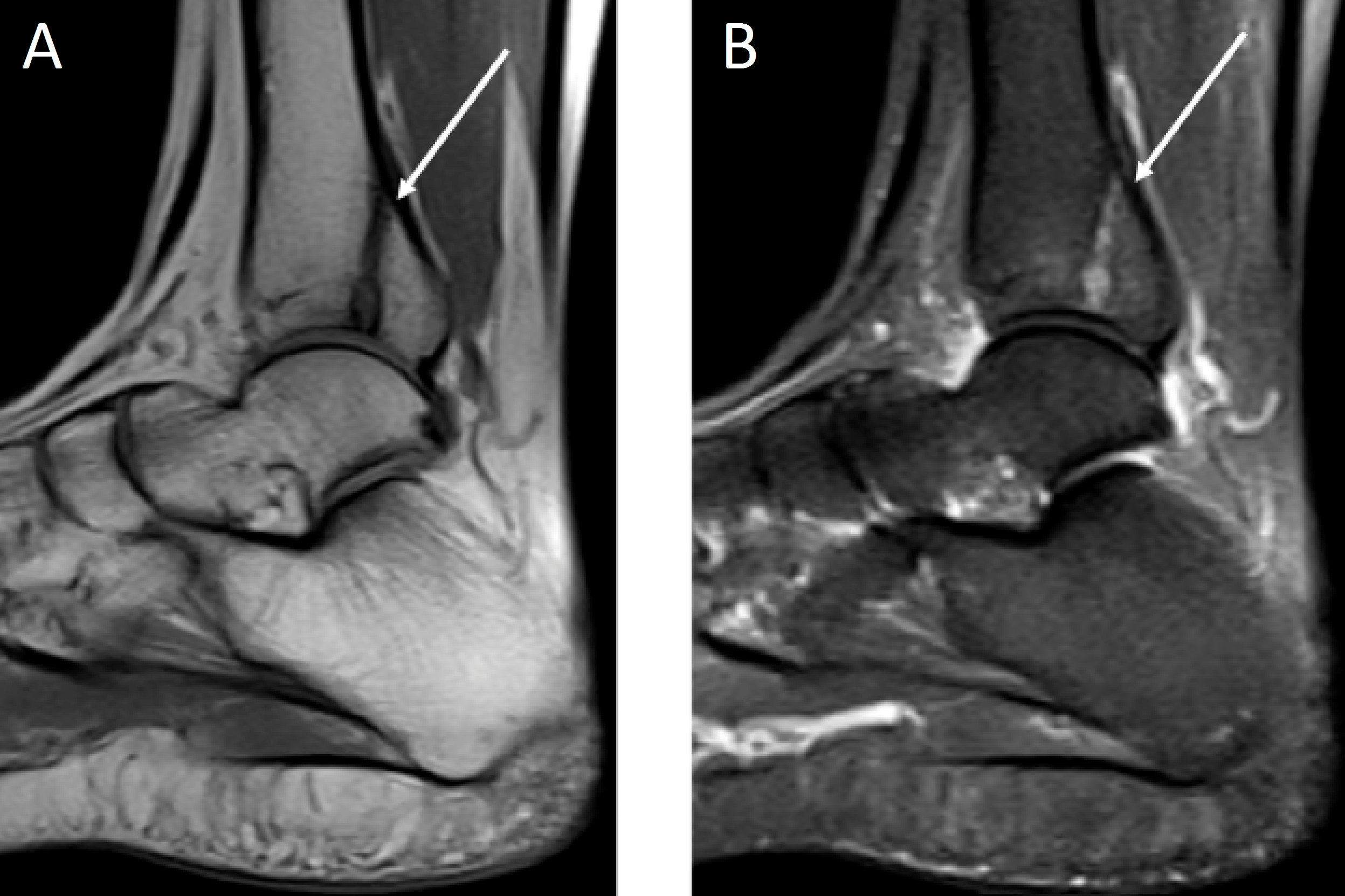
Figure 1 Right ankle sagittal T1 weighted image MRI in A and T2 STIR weighted in B demonstrating posterior malleolus fracture (white arrow).
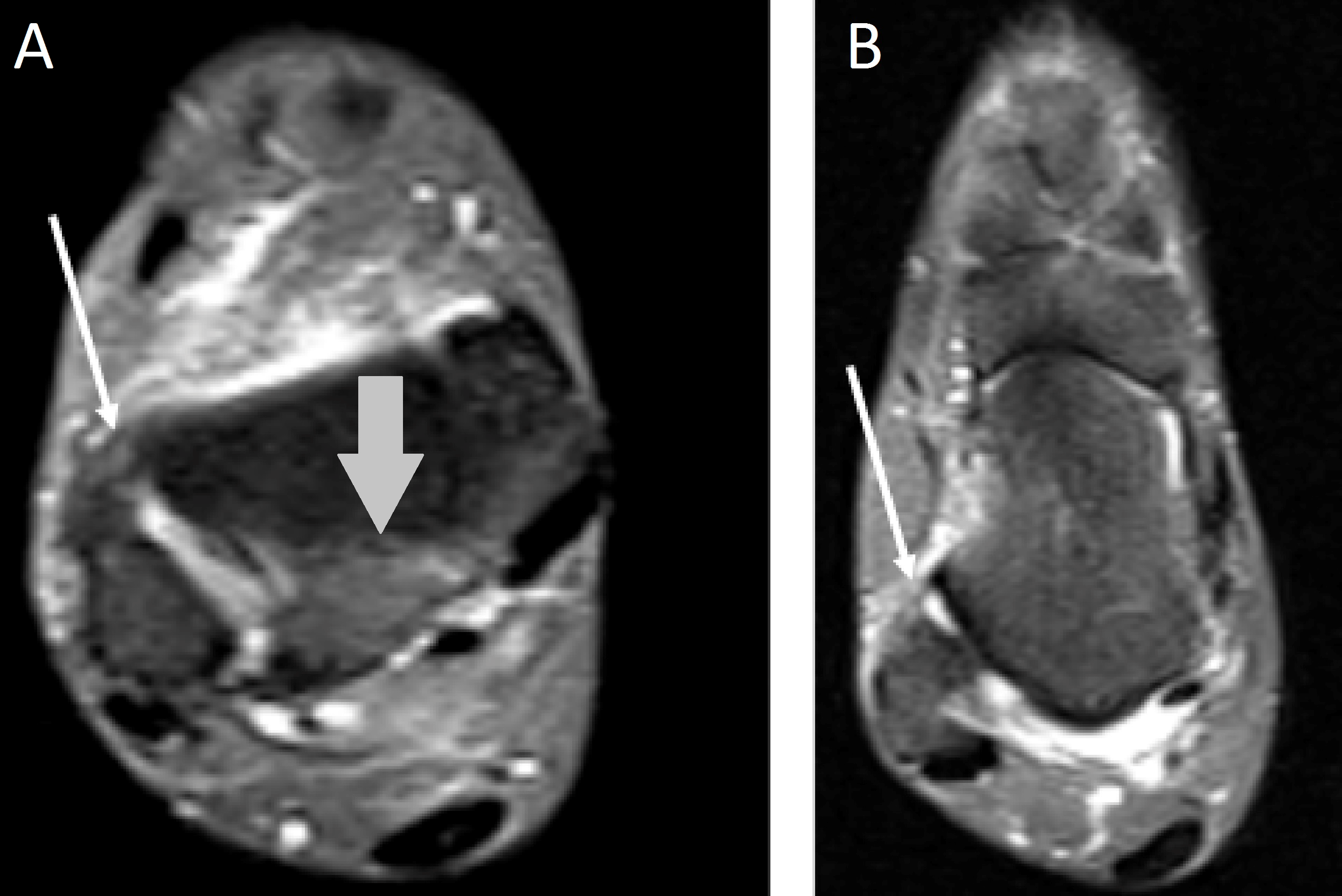
Figure 2 Right ankle axial T2 STIR weighted image MRI of the right ankle in A demonstrating partial tear of the anterior tibiofibular ligament (white arrow) and posterior malleolus fracture (grey arrow). Right ankle axial T2 STIR weighted image MRI in B demonstrating partial tear the anterior talofibular ligament (white arrow).
The patterns of the posterior malleolus fracture are more relevant in comparison with the fracture fragment dimensions in decision making.3 The deep deltoid ligament is the primary source of ankle stability.3 Although Haraguchi type II classification can be tiny in dimension, this fracture is inherently unstable. The failure to recognize this lesion pattern may conduct to unsatisfactory clinical outcomes and persistent talar subluxation.3 During supination or pronation, the excessive traction of the posterior part of the inferior tibiofibular ligament can lead to the posterior malleolus fracture.5,6
Isolated posterior malleolus fractures account for 1% of all ankle fractures and can imitate a simple ankle sprain.3 The patients usually have nonspecific complaints of a typical ankle sprain,3 making, sometimes, difficult to perform the diagnosis. This fact demonstrates the importance of imaging tests.
X-rays are not sufficient for diagnosing isolated posterior malleolus fractures.5 The x-ray test of the injured ankle contains true anteroposterior, mortise (anteroposterior with 15° internal rotation), and lateral views.2 Ebraheim et al. documented that posterior malleolus fractures that could not be elucidated on basic x-ray views were identified on 50° external rotation lateral x-ray.5–7 An atypical (vertical) line of the standard horizontal or lightly oblique medial malleolus fracture in type Danis–Weber B and C fractures can signify a posterior malleolus fracture.2
There is agreement that the true dimensions and geometry of the fragment, specifically its medial part, and intercalary fragments may be diagnosed solely by computed tomography (CT scan). CT scans in the transverse and sagittal planes should be integrated with 3D CT reconstruction to acquire a precise anatomical image. Magnetic resonance imaging (MRI) may deliver more data about syndesmotic ligaments, tendons, and osteochondral lesions. But it´s adopted only exceptionally.2
Functional outcomes of ankle fractures concerning a posterior malleolus fracture are frequently less satisfactory based on the dimensions of the posterior fragment.5 There are controversies regarding the treatment of these fractures, but there is an agreement that small fragments can be treated without surgery, and larger fractures that affect more than 25% of the articular surface should be fixed to avoid instability and degenerative lesions.5 Joint-preserving osteotomies may treat symptomatic malunions or nonunions with joint displacement if no post-traumatic arthritis has developed. Ankle fusion with realignment remains a salvage alternative in cases of arthritis.2
Not applicable.
The authors declare that there is no conflict of interest regarding the publication of this paper.
The written informed consent of the patient was obtained, for the publication of her case.
None.

©2022 Duarte, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.