International Journal of
eISSN: 2574-8084


Technical Paper Volume 11 Issue 5
GenesisCare Oncology, Australia
Correspondence: Thulani Nyathi, GenesisCare Oncology, South Australia, Adelaide, 5000, Australia
Received: September 13, 2024 | Published: September 24, 2024
Citation: Ho T, Edwards R, Nyathi T, et al. Implementation of the HexaPOD™ evo RT system for conventionally fractionated head and neck radiotherapy. Int J Radiol Radiat Ther. 2024;11(5):120-124. DOI: 10.15406/ijrrt.2024.11.00398
Introduction: Head and neck cancer (HNC) treatments often involve long treatment fields whose treatment accuracy can be impacted by rotational and translational inconsistencies. Studies have demonstrated that even small rotational setup errors can result in large displacements at the ends of the target. One method for correcting the treatment position in six dimensions (6D) is to use a robotic couch. This study aimed to determine if using one to facilitate the correction of the treatment position was feasible for HNC patients treated in our centre and to report on the implementation experience.
Methods: This two-phase study involved a retrospective review of 100 pre-treatment registration images to establish the magnitude of the rotations followed by a prospective analysis of daily pre-treatment images for 20 patients.
Results: The mean difference of the vector shift for the first phase, was statistically significant (p-value < 0.05) between image registrations with 6D compared with those in three dimensions. The post imaging rotational shifts for the second phase, ranged as follows: pitch (-1.1° to 2.0°); roll (-0.9° to 1.7°) and yaw (-1.1° to 1.8°). The pitch reported the greatest average shift (30% >1°). 23% of the average rotational shifts were > 1° and ≤ 2°.
Conclusion: Centres that are equipped with the HexaPOD™ system can consider its use in head and neck treatment to improve set up and treatment accuracy.
Keywords: 6 degrees of freedom, head and neck radiotherapy, image matching, image guidance, rotational shifts
CT, computed tomography; CBCT, cone beam computed tomography; DoF, degrees of freedom; FDK, feldkamp-davis-kress; HNC, head and neck cancer; MMI, maximising mutual information; VMAT, volumetric modulated arc therapy; XVI, x-ray volumetric imaging
Radiotherapy is an ever-changing field with the continual introduction of new technologies to improve upon traditional imaging and treatment techniques.1 Such improvements include increasing treatment accuracy, organ at risk dosimetry and therefore less toxicity.2 Head and neck patients can experience particularly intense side effects.2 Toxicities develop due to the proximity of treatment volumes to normal critical structures in the head and neck region that inevitably receive significant mid to low dose radiation. Patients are immobilised to ensure accurate dosing of the clinical target volumes while minimising dose to healthy tissue. Accuracy improves with minimisation of the discrepancy between the treatment and baseline planning images.3 In an ideal scenario, the treatment image would perfectly overlay with the planning CT scan requiring no corrections. The head and neck anatomy is mechanically flexible which adds to the uncertainties in the reproducibility of patient set-up.4 To compound this, typical HNC treatment volumes are elongated in the superior–inferior direction with the inclusion of the cervical lymph nodal chains, which tend to be relatively superficial, non-spherical and often greater than 20 centimetres in length.5,6 These long volumes may contribute to positional discrepancy, which can cause the delivered dose distribution to deviate from the treatment plan.6,7
Traditionally, setup error corrections are only applied using the three translational directions with rotational corrections often overlooked. Studies have demonstrated that in the treatment of elongated targets, such as HNC, even small rotational setup errors can result in large displacements at the ends of the target.8 When reduced treatment margins are used, as is typically the case for HNC, the risk of geographical displacement becomes more significant.9
One technological advancement that aims to improve the inherent problems with radiotherapy reproducibility is the introduction of robotic couches. Robotic couches allow for six degrees of freedom (6 DOF) and can apply rotational isocentre corrections (roll, pitch, and yaw) alongside the three traditional translational shifts. The utilisation of robotic couches has traditionally been limited to stereotactic treatments, as evidence has shown a positive correlation with applying 6 DOF for small, highly conformal treatment volumes which are sensitive to changes in tissue depth and patient contour.3 Prior to this study our clinic only utilised the robotic couch for small field cranial and extra-cranial stereotactic treatments. There is limited research and evidence for utilising robotic couches in conventional radiotherapy to extra cranial sites and the amount of expected rotational couch movement for HNC treatments is not reported.10
The aim of this study was to firstly retrospectively assess verification images to quantify the degree of rotational shifts for a HNC patient cohort and confirm the feasibility of implementing a robotic couch for treatment. The second phase was to report the experience of implementing a robotic couch on the first 20 HNC patients treated at our clinic.
Ethics Approval
This study had research ethics approval granted by the St Vincent Hospital, Human Research Ethics Committee (HREC 2022/ETH00247: GenesisCare Oncology Outcomes).
First phase
The oncology information system, MOSAIQ™, was interrogated for head and neck patients who had been treated utilising a robotic couch. Pre-treatment image registration data was reviewed for the ten most recent patients. For consistency, this review was performed by a single radiation therapist with over 20 years of clinical experience. For each patient, the cone beam CT (CBCT) was rematched with the planning CT, including both translational and rotational shifts and the mismatch was compared to the original recorded translational shifts.
Second phase
Patient selection: Patients undergoing volumetric modulated arc therapy (VMAT) to the head and neck were prospectively recruited onto the study, between February 2023 and October 2023. Eligibility criteria included patients diagnosed with primary head and neck cancer who were treated with a Type -S™ couch overlay (CIVCO RT Legacy Products, Iowa, USA) in combination with the 2.4 mm Klarity® head and shoulder masks (Klarity Medical & Equipment Co, Guangzhou, China) on a robotic couch, receiving between 20 and 35 fractions. Each patient had a CBCT acquired daily prior to treatment and isocentre corrections applied in six dimensions.
Pre-treatment imaging protocol: A daily CBCT was acquired using the onboard X-ray Volumetric Imaging (XVI) imaging technology. A half-arc / rotation was acquired for the CBCT. The Feldkamp-Davis-Kress (FDK) cone-beam back-projection algorithm was utilised for image reconstruction. Automatic bone matching followed by manual registration was performed using an online image guided radiation therapy strategy prior to treatment. Patient positioning was performed using the robotic HexaPOD™ evo RT system (Medical Intelligence, Schwabmünchen, Germany). The HexaPOD™ evo RT system consists of the HexaPOD™ robotic couch top and the iGUIDE® software which translates the positional error values into movement commands for the robotic couch top.
The work instructions for cranial stereotactic radiosurgery/ radiotherapy which utilises the HexaPOD™ couch was adapted and customised to suit the conventionally fractionated head and neck patients. The work instruction had routine technical and governance review before approval for use in the clinic. In addition, a credentialling checklist was developed for radiation therapists to assist in practical training in the use of the HexaPOD™ system. The linac used in this study was already delivering stereotactic treatments and therefore the pre-existing quality assurance procedures were deemed sufficient by the medical physics team.
The reference CT dataset was imported into the XVI database via DICOM. Processing of the reference dataset included positioning of the correction reference point at the isocentre, defining a clipbox which determined the voxels to be included in the image registration. Encompassed in the clipbox were the target volumes and organs at risk. All data sets in this study were imported and referenced using the same method. As per the clinic work instructions, the clipbox was adjusted to include the target PTV and adjacent vertebrae. The mandible was only included in the clipbox if the PTV was situated anteriorly. Pre-treatment image registration was performed using the XVI software with the bony landmarks used for matching while both translation and rotation corrections were active. Two radiation therapists reviewed images online and the treating radiation oncologist approved the images offline once per week.
Based on the analysis of the data collected in phase 1 of the study and clinical experience, a decision-making matrix was developed to aid online image registration. Table 1 describes the decision-making matrix used for the second phase of the study.
|
Couch shift direction |
Magnitude |
Action required |
|
Translations and / or Rotations |
Shift ≤ 1 .0 cm |
Apply shift from treatment console Proceed with treatment after shift applied |
|
Shift ≤ 2.0° |
||
|
|
|
|
|
Translations and / or Rotations |
1.0 cm ≤ Shift ≤ 2 .0 cm 2.0°≤ Shift ≤ 3.0° |
Apply shift from treatment console Repeat imaging to confirm shifts Proceed with treatment after shift applied |
|
|
|
|
|
Translations and / or Rotations |
Shift > 2 .0 cm |
Re do patient set-up Proceed with imaging again |
|
Shift > 3.0° |
Table 1 Image registration decision-making matrix
Statistical analysis: All numerical data analysis was conducted in Microsoft Excel™ (Microsoft Corporation, USA) to derive both descriptive and analytic statistics. A test of normality on the collected data was determined.
First phase
One hundred pre-treatment CBCT images from ten HNC patients were reviewed to ascertain the magnitude of the couch shifts. The original couch translations were obtained from MOSAIQ™. To obtain the couch rotations, the 100 CBCT images were rematched with 6DOF applied within MOSAIQ™ using the Maximising Mutual Information (MMI) image registration algorithm. To facilitate comparison of the original 3D match with the 6DOF match, the mean displacement vectors for the translations and the L2 -norm of the rotations was computed. The mean displacement vector is defined as the shortest distance from the setup point to the isocentre.
The distribution of the mean translations and rotations is shown in Figures 1 and 2.
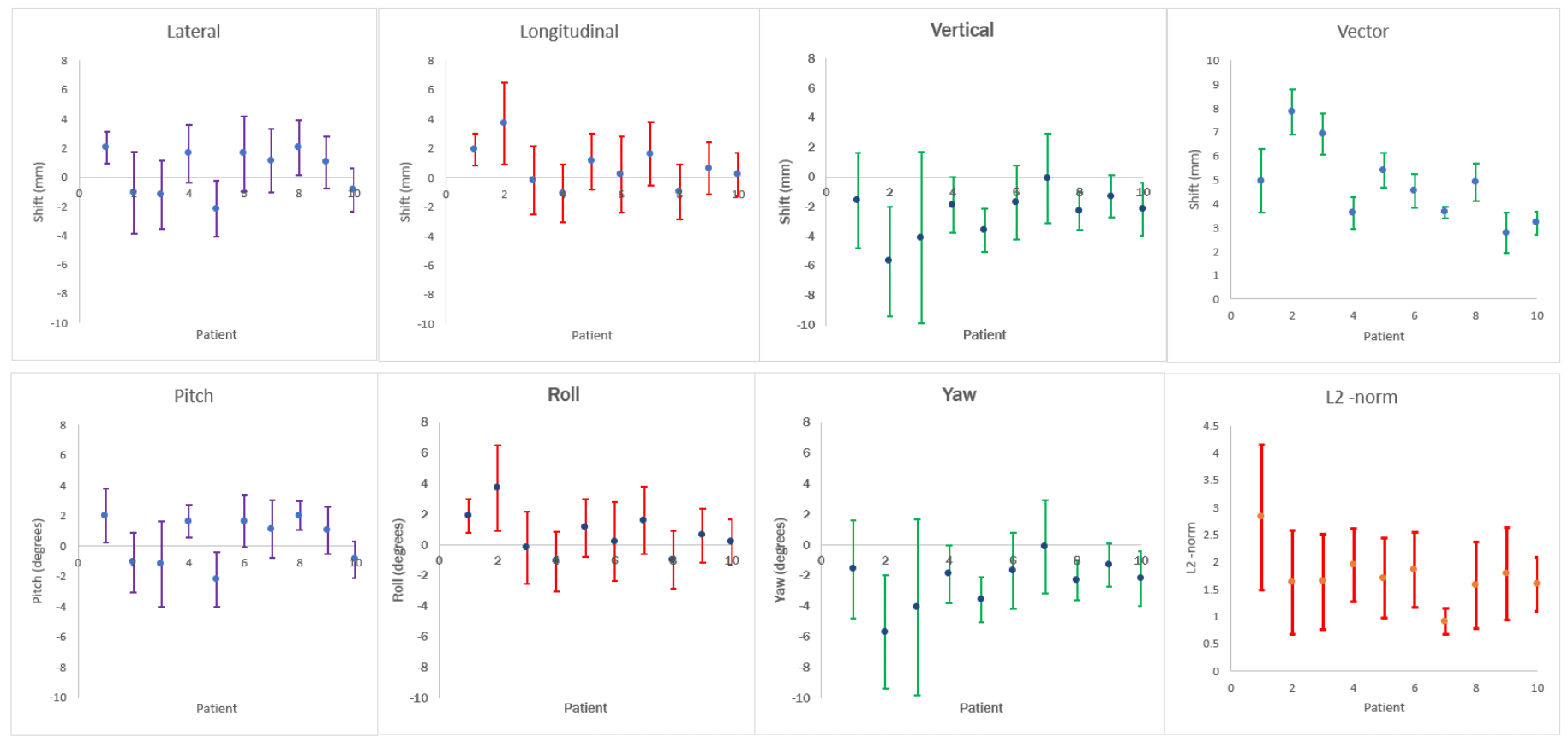
Figure 2 Average translations, vectors, rotations and the L2 -norm for the first phase after introducing rotations in the image registration.
The statistical significance of the mean difference in the translations was determined using the t-test methodology. Results of the t-test are shown in Table 2.
|
|
Lateral (mm) |
Longitudinal (mm) |
Vertical (mm) |
Vector (mm) |
|
Mean difference |
-0.3 |
0.1 |
0.2 |
-0.3 |
|
Standard Deviation |
0.6 |
0.6 |
0.8 |
0.5 |
|
p - value |
0.07 |
0.29 |
0.28 |
0.04 |
Table 2 Average displacements and standard deviation of translations
Only the mean difference of the vector was found to be statistically significant.
In addition to the statistical evidence, it was evident clinically, that introduction of rotation corrections in the image registration led to a better image match and anecdotally, greater satisfaction by the radiation therapist performing task. Figure 3 demonstrates the effect of introducing rotation correction in a typical head and neck case.
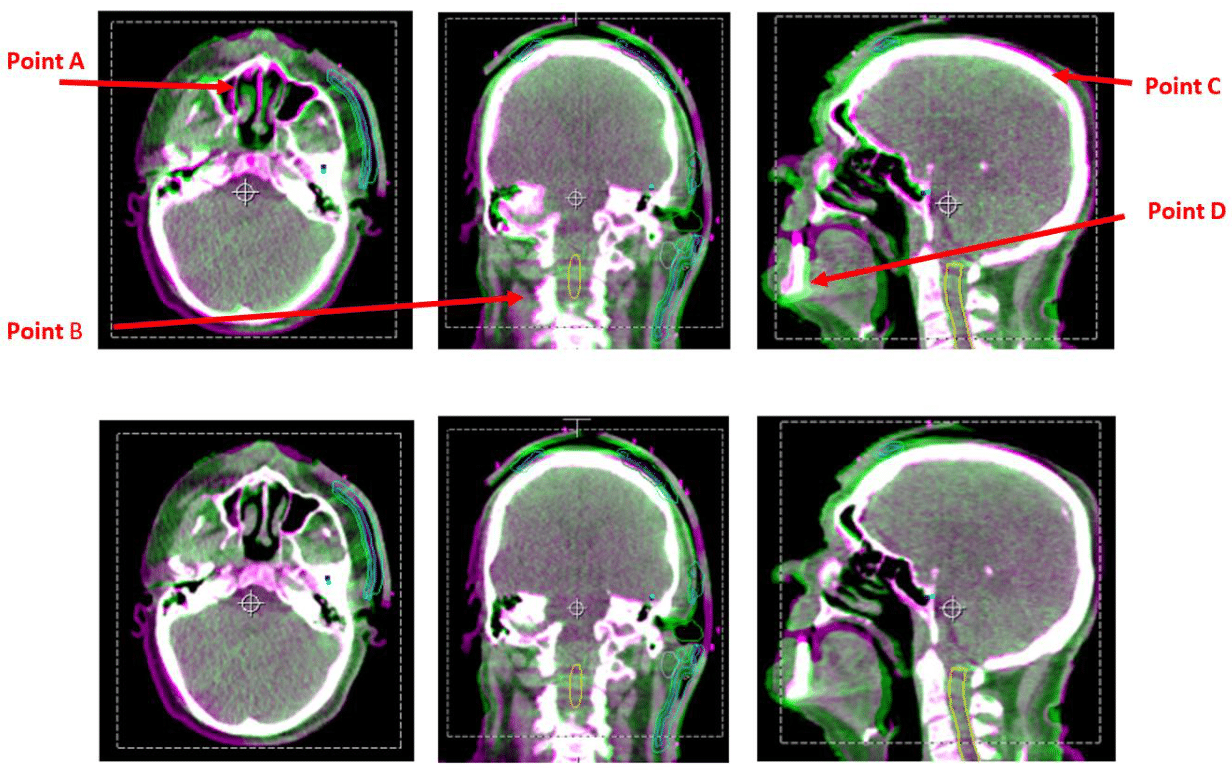
Figure 3 Illustrations demonstrating the impact of including rotations in the image registration – bottom row of images has both translation and rotation corrections applied (6D).
The greatest discrepancies can be seen at points A, B, C and D where the anatomy is not perfectly overlayed. From this example, introduction of rotational corrections led to superior image registration.
Second phase
Twenty patients, 16 male and 4 female, ranging in age from 33 to 98 years, undergoing high dose radiotherapy for HNC were enrolled into this study. The number of fractions ranged from 20 to 35 with 90% of patients receiving between 30 – 33 fractions. The treatment field length was ≥ 20cm for 70% of patients (range 10 to 30 cm).
In total, 622 partial arc CBCT scans were acquired and registered against the reference CT dataset. The CBCT imaging presets were optimised for both image quality and dose, always terminating at a gantry geometry consistent with the gantry start position for the treatment beam.
Figure 4 represents the average translations and rotations for each study participant. The post imaging shifts ranged from: lateral (-3.5 mm to 2.5 mm); longitudinal (-4.0 mm to 3.1 mm); vertical (-4.5 mm to 2.5 mm); pitch (-1.1° to 2.0°).; roll (-0.9° to 1.7°). and yaw (-1.1° to 1.8°).
Standard deviation as a measure of inter-fraction setup fluctuation for rotations was the least for yaw and highest for roll, however, the pitch recorded the greatest magnitude of average rotation. Optimal reproducibility was achieved in the sense that for both translations and rotations average shifts were within a single standard deviation.
An analysis of the average rotational shifts showed that 97% of all CBCTs required a rotation ≥ +/- 0.5°. Sixty percent of the patient cohort required a rotation ≥ +/- 0.5° in any direction for every fraction. Also 60% of the patient cohort would have had a pitch rotation ≥ 2°in one or more of the prescribed fractions. A 2° rotation equates to a 3.5 mm mismatch at the periphery of a 20 cm long field.
The greatest shift was recorded for pitch (100% > 0.5° and 30% > 1°), followed by roll (70% > 0.5° and 15% > 1°) and yaw (35% > 0.5° and 10% > 1°). For this cohort only a single study participant had an average rotational shift of more than 1° in more than one rotational axis (pitch and roll).
As a measure of workflow efficiency, the treatment episode time was recorded for each fraction. For this cohort, the treatment time varied from 9 to 12 minutes. During the early stages of this study, an 18-minute time slot was allocated for each treatment. After an initial learning period, 12-minute treatment slots were allocated, and this was found to be optimal. For comparison, this is the same time allocated to head and neck patients being treated on platforms without a robotic couch at our clinic.
The results from this study are in line with others, demonstrating that long HNC treatment fields (>20cm) benefit from applying rotational corrections.5,7 Seventy percent of the phase 2 study participants had long fields (>20cm) and 100% of images required a rotation of at least 0.5° and 30% > 1°. This was most significant for pitch. This finding coincided with the literature which noted the imaging displacement for HNC experienced with rotation is most amplified at the superior and inferior extremes.5
The strengths of this study are also in part, its limitations. The first being a single experienced radiation therapist was used for the pilot study image registration with the aim of achieving consistency. However, this approach also carries potential bias. Furthermore, the matching algorithms are different between MOSAIQ™ and the XVI so it’s plausible that the image registration could be different between the two platforms. Even if this is the case, the visible difference between 3D versus 6D corrections is still present.
Another limitation was the study did not include post treatment scans to measure intrafraction stability. This has been commented on in other studies that noted with increased tilting from rotation comes the potential for patient drift within the thermoplastic mask. However, this was only observed when a rotation of > 3° degrees was applied.10 Our study did not allow for rotations > 3° to be applied due to hardware limitations.
This study has intentionally not investigated the dosimetry impact of ignoring couch rotations in this patient cohort Numerous studies, including the one conducted by Fu et al 2012, have demonstrated that rotational corrections have a significant impact on the dosimetry.7 Notwithstanding, despite these limitations the overall outcome of this study remains valid.
This study has proven that a robotic couch can be efficiently used in a busy metropolitan clinic for conventionally fractionated head and neck radiotherapy.
This study reported on successful implementation of the HexaPOD™ evo RT system for treatment of HNC. This implementation has proven to be efficient both in terms of the clinical workflow and technological resource utilisation. Clinics should consider implementing 6 DOF when treating patients with HNC.
None.
The authors declare no competing interests.

©2024 Ho, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.