International Journal of
eISSN: 2574-8084


Case Report Volume 11 Issue 5
1Senior Consultant, Department of Radiology, Marengo Asia Hospitals, India
2Head of Department, Department of Radiology, Marengo Asia Hospitals, India
3Head of Department, Department of Neurology, Marengo Asia Hospitals, India
4Research Manager, Department of Radiology, Marengo Asia Hospitals, India
5Consultant, Department of Radiology, Aster Mims Hospital, India
6MBBS Candidate, GKT School of Medicine, King’s College London, London, UK
Correspondence: Dr Nikita Jajodia, Department of Radiology, Marengo Asia Hospitals, Gurugram, Golf Course Ext Rd, Sushant Lok II, Sector 56, Gurugram, Ghata, Haryana, India, 122011, Tel +91 7875983200
Received: July 29, 2024 | Published: September 13, 2024
Citation: Mittal S, Jain KK, Agarwal K, et al. Gluteal metastasis on both sides from Esophageal Carcinoma. Int J Radiol Radiat Ther. 2024;11(5):116-118. DOI: 10.15406/ijrrt.2024.11.00397
Hematogenous metastasis of esophageal carcinoma is not uncommon however esophageal carcinoma metastasis to skeletal muscles is a rare entity. Here, we report the case of metastasis in gluteus muscles on both the sides in a known case of Ca Esophagus (Adenocarcinoma). Early diagnosis of the possibility of metastasis in muscles in a cancer patient can increase the life expectancy and can reduce the rate of complications.
Keywords: metastasis, gluteus maximus muscle, esophageal carcinoma, magnetic resonance imaging
Esophageal cancer is histologically a squamous cell carcinoma (SCC). Adenocarcinoma type of carcinoma is an aggressive cancer;1,2 and it is the eighth most common type of cancer posing to be the major cause of death in cancer patients (sixth in position). World-wide the prevalence of squamous cell carcinoma of esophageal carcinoma is higher as compared to Adenocarcinoma. However, in developed countries it is the prevalence of adenocarcinoma3,4 of the Esophagus which is higher. The most common sites of metastasis of esophageal carcinoma include liver, lungs, adrenals, bone, pleura, peritoneum or pericardium. The lesser common site involves thyroid, pancreas, spleen, ovary, kidney, heart, skin, gallbladder or small and large bowel.
Skeletal muscle involvement as metastasis is a rare entity & the reason for this is not yet fully understood, while some authors have suggested that it is the rich supply of blood, high systolic fluctuations in the skeletal muscles which could be a reason for lower spread of metastasis in the muscles. Most frequent location of muscle metastasis is thigh muscles, paravertebral muscles, the extra ocular muscles and the gluteal muscles. Most common malignancies which lead to muscle metastasis are lung cancer (25.1%), gastrointestinal tumours (21.0%), and urological tumours (13.2%).5,6
A 73-year-old male was referred to our Radiology Department for MRI gluteal region left side. He was a known operated case of adenocarcinoma of CA oesophagus 4-5 years back. He first visited the Neurology department with complaints of tingling/numbness and pain in the left gluteal region.
The patient was undertaken for Contrast MRI to rule out the abscess MRI was performed at 3-T (ACHIEVA, Philips Medical Solutions) including T1-weighted, axial T2-weighted, coronal T1-weighted, and sagittal T2-weighted turbo spin echoes and coronal Short Tau Inversion Recovery (STIR) sequences. A soft tissue lesion measuring 9.8 x 5.9 x 9.5 cm was seen in left Gluteus Maximus muscle with mild surrounding oedema and heterogeneous enhancement with non-enhancing areas on post contrast images. Neurovascular bundle was intact. Incidentally, similar appearing lesion measuring 19 x 25 x25mm is also seen in right Gluteus Medius muscle (Figures 1a&1b). There was no haemorrhage or calcification within the lesion. A provisional diagnosis of neoplastic aetiology was considered. For confirmation, Ultrasound-guided biopsy was performed which confirmed the features of metastasis from esophageal adenocarcinoma. Sections from Trucut biopsy showed malignant tumor arranged to form sheets, islands and cords of tumor cells which were round to oval with plemorphic, hyperchromatic nuclei and prominent nucleoli. Cytoplasm was moderate and pale. Tumor was seen to be infiltrating the fibrous stroma, Occasional mitotic figures were also seen along with large area of necrosis (Figure 2). The patient was eventually managed with chemotherapy for muscle metastasis.
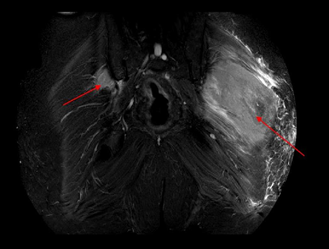
Figure 1a A soft tissue lesion measuring (AP *ML * SI) 9.8 x 5.9 x 9.5 cm seen in left Gluteus Maximus muscle (on MRI STIR coronal images).
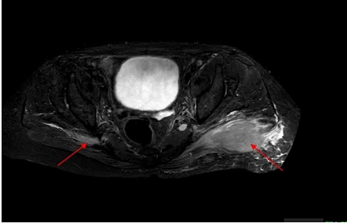
Figure 1b A soft tissue lesion measuring (AP *ML * SI) 19 x 25 x25mm is seen in right Gluteus Medius muscle (on MRI STIR axial images).
MRI Gluteal region PD SPAIR PDW SPAIR (Proton Density Weighted Spectral Attenuated Inversion Recovery), a) Coronal images b) axial images showing large hyperintense soft tissue lesion in left gluteus maximus muscle (red arrow) with surrounding edema and lesion seen on right side in gluteus medius muscle.
Both, primary and metastasis is rare in skeletal muscles. The cited factors for such occurrence is the muscular contractility, local biochemical conditions, local changes in PH, local temperature and high resistance present in the blood vessels.7 Muscle metastatis can present as local pain, clinically palpable mass, firm hard subcutaneous swelling as well as neuropathy (as seen in our case). Generally, metastasis in the muscles is seen at an advanced stage having poor prognosis.
Few Primary malignancies which can cause muscle metastasis are bronchogenic carcinoma, melanoma, renal cell carcinoma, thyroid, colon, and sarcoma. Esophageal Carcinoma to skeletal muscle metastasis is relatively uncommon. In totality, metastasis from Adenocarcionoma over squamous cell carcinoma type of Esophageal Carcinoma is more common accounting for over 75% of all cases.7-10 Also, histopathologically adenocarcinoma are more common type of carcinomas as compared to others.8
Risk factors of Esophageal cancer are different for adenocarcinoma and squamous type. Squamous carcinoma is gender and race specific (Squamous cell carcinoma is the most frequent in black individuals and white women), while adenocarcinoma is predominant in white men.3 Various environmental factors predispose and individual for cancer including smoking, alcohol, diet and nutrients, genetics (Tylosis, an autosomal dominant disease, familial aggregation in population of high incidence of esophageal carcinoma).
Adenocarcinoma’s occurrence differs in gender and race specificity as compared to Squamous cell carcinoma. Adenocarcinomas are more common in men than in women and more common in whites than in blacks in the United States). Gastroesophageal reflux disease and Barrett’s esophagus, obesity, tobacco, alcohol consumption, nutritional deficits, Drugs (non-steroidal anti-inflammatory drugs (NSAIDs), proton pump inhibitors (PPIs) and statins in patients with BE and genetic may increase the chance of adenocarcinoma.3,4
The root cause of the spread to the muscle may either be the arterial route, venous plexus, or intramuscular lymph nodes.6 The distant muscle metastasis from esophageal carcinoma is extremely rare with few articles reporting such cases.
In a study done by Cincibuch et al.5 from a cohort of 205 patients he reported five cases of muscle metastasis with esophageal carcinoma involving the quadriceps femoris, gluteus minimus, subscapularis, iliacus, and one was multiple. Two were metachronous and three were synchronous.
Geukens et al.9 described a case of adenocarcinoma of the esophagus metastasis in gluteus maximus muscle (as observed in our study).
Muscle metastasis in adductors from adenocarcinoma of esophagus was reported in a case by Sohda et al.10 Similarly, an ossifying metastasis in hamstring muscles were seen in a case of adenocarcinoma of the esophagus reported by Freer et al.7
As discussed skeletal muscle metastasis is rare and muscle metastasis from gastrointestinal system is even rarer. The most commonly involved muscles in adenocarcinoma of the esophagus are the diaphragm, rectus femoris muscle of the abdomen, deltoid, psoas, intercostal, spinal muscles, thigh muscles and lastly the gluteal muscles.9 Few studies have stated that the MRI shows ossification within them and the ossifying muscle are seen in primary mucinous adenocarcinomas involving the colon, stomach, small bowel and more rarely the breast, ovary, prostate, balder and skin.9,11 The only method to confirm the diagnosis is a biopsy. However, PET-CT and MRI with contrast does help in suspicion of a neoplastic aetiology. While, the plain CT and conventional radiographs may help in identifying the calcification or heterotopic ossification in the muscle/soft tissues but fails in differentiating primary ossifying lesions from the metastatic ones.
Here, MRI, helps in raising suspicion of neoplastic characters of the soft tissue lesions but lacks the required specify, which later needs to be confirmed by a biopsy. The role of MRI in soft tissue lesion is superior over CT/conventional studies. In tumor hypointensity on T1- weighted images, high signal intensity on T2- weighted images, and intense signal enhancement on post gad T1-weighted images may be seen in many tumoral and inflammatory conditions.9,12 The differential diagnosis of muscular lesions one must consider metastasis, soft-tissue sarcoma, myositis ossificans and muscle injury.
Metastasis in skeletal muscle is uncommon, but patients presenting with soft tissue swelling in a known case of carcinoma should be investigated with PET-CT/MRI keeping in mind the possibility of metastasis and in case of suspicion of malignancy a biopsy should be considered. As METS in skeletal muscle is considered as an advanced stage, its quick and early diagnosis can help in improving patient’s life expectancy.
Ethical clearance: Since the study is a retrospective case report and didn't require ethics approval.
None.
Authors declare that there is no conflicts of interest.

©2024 Mittal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.