International Journal of
eISSN: 2574-8084


Research Article Volume 10 Issue 4
Department of Radiation Oncology, Medical University of South Carolina, Charleston, South Carolina, USA
Correspondence: Jean L. Peng, Ph.D., Department of Radiation Oncology, Medical University of South Carolina, 169 Ashely Ave, Charleston, SC, USA 29425
Received: September 05, 2023 | Published: September 20, 2023
Citation: Peng JL, McDonald DG, Warwick LM, et al. Dosimetric evaluation of accelerated partial breast irradiation (APBI) using volumetric modulated arc therapy (VMAT) technique. Int J Radiol Radiat Ther. 2023;10(4):101-105. DOI: 10.15406/ijrrt.2023.10.00363
Purpose: Five-fraction radiation therapy treatment regimens for accelerated partial breast irradiation (APBI) using intensity modulated radiotherapy (IMRT) have become increasingly used after several phase three trials demonstrated similar or reduced toxicity compared with whole breast irradiation. Improving the treatment efficiency of this technique could significantly improve delivery accuracy and tolerability, especially for treatment plans utilizing deep inspiration breath hold (DIBH) technique. The aim of this study was to determine the optimal technique for APBI, with a focus on volumetric modulated arc therapy technique (VMAT) and flattening-filter free (FFF) delivery.
Methods: Ten APBI cases, five cases each left and right breast, were randomly selected. Each case was contoured following guidelines included in the APBI-IMRT-Florence Trial and planned to use both non-coplanar static-field IMRT with standard flattened-filter (FF) beam and VMAT techniques with both FF and FFF beam. For each VMAT plan, two partial arcs were used with patient-specific start and stop angles. Arc extents emulated opposed tangential fields and were chosen based on target and organ at risk (OAR) locations. Evaluated OARs included the heart, ipsilateral and contralateral lung, and normal breast. All plans were generated using the Eclipse treatment planning system (Version 15.6). A prescription dose of 30Gy delivered in 5 fractions was used for all cases. Plans were compared and evaluated using several dose metrics as well as treatment time.
Results: For targets, VMAT exhibited similar coverage (V95%) but higher Dmax compared to IMRT (105% (IMRT) v.s .111% (VMAT), p=0.002. VMAT provided similar OAR avoidance compared to IMRT for the heart (Dmean, V3Gy, V0.5Gy), ipsilateral lung (V10Gy), contralateral lung (V5Gy) and contralateral breast Dmax within 10cGy/2% (p~0.005). VMAT contributed slightly lower dose outside the target in the ipsilateral breast, with an average difference in V15Gy of approximately 8% (37% (IMRT) v.s. 29% (VMAT)). Finally, because IMRT delivery is non-coplanar, and typically requires at least 5 treatment fields, co-planar VMAT reduced the total treatment significantly. VMAT with FF beam energies also used fewer monitor unites compared to IMRT with FF beam energies. The utilization of FFF beam energies for VMAT further improved delivery time compared to IMRT. Overall, VMAT with FFF beam energies reduced treatment time by approximately 20% compared to IMRT with FF beam.
Conclusions: Co-planar partial-arc FFF VMAT technique produced equivalent target coverage, improved efficiency, better normal tissue sparing, and shorter delivery time compared to non-coplanar IMRT technique. Shorter delivery time also assists in the reduction of patient motion associated with breath hold. VMAT technique with FFF delivery is a suitable replacement for IMRT in APBI.
Great progress has been made in understanding the biology and pathology of breast cancer over the past few decades, resulting in a dramatic shift in management of the disease. The historic a one size-fits-all approach, typically involving Halsted mastectomy, has evolved into a personalized conservative approach, addressing each patient’s individual risk of recurrence. This change in treatment paradigm began with landmark trials1-2 showing equivalent overall survival for patients undergoing breast-conserving surgery followed by whole breast irradiation (WBI) when compared to modified radical mastectomy alone. Breast-conserving therapy has since been established as the preferred treatment option for most early-stage breast cancer. Subsequently, partial-breast irradiation (PBI) was introduced as an alternative treatment approach for selected patients with early breast cancer. Estimated advantages of PBI as compared with WBI included shorter overall treatment course when using accelerated fractionation schemes (APBI), improved adverse events profile, and cost reduction.3 Postoperative APBI can be delivered using a variety of different techniques. These include external beam radiotherapy delivered using three-dimensional conformal RT (3DCRT) or intensity-modulated RT (IMRT), as well as interstitial and intracavitary (balloon-based devices) brachytherapy. Historically, external beam APBI required large planning target volume (PTV) margins to account for setup uncertainty, resulting in increased healthy tissue exposure and inferior cosmetic outcomes relative to whole breast radiotherapy.4 This led to an increase in popularity for brachytherapy APBI. However, recent technical improvements in patient immobilization, imaging, and dosimetry have allowed external beam APBI to be delivered with reduced margins and steeper dose fall-off outside of the target, leading to renewed interest.
Although different APBI treatment techniques and fractionation schedules currently exist, a consistent advantage of APBI, as compared to WBI (conventional or moderate hypo-fractionated schedules), is the reduction in overall RT treatment course time. Shorter fractionation schedules may lead to better compliance and health-related quality of life for affected patients. Worldwide, the impact of APBI in terms of cost-effectiveness and reduction in overall treatment time is heterogeneous and data is still limited. In 2009, the Harvard Radiation Oncology Program published a cost-effectiveness analysis on APBI versus WBI for early-stage breast cancer patients. The authors developed a Markov model to describe health status over 15 years after RT. According to their findings, external beam APBI was the most cost-effective approach for post-menopausal patients.5 Several phase III trials have demonstrated the non-inferiority of APBI versus WBI in terms of local recurrence, and similar or reduced toxicity at 5 years. A landmark phase III APBI trial from the University of Florence published results at both 5 years,6 and long-term results at a median follow-up of 10 years.7 This trial evaluating intensity-modulated radiation therapy (IMRT) APBI with a fractionation schedule of 30Gy in 5 fractions showed no significant difference between APBI and WBI in terms of ipsilateral breast tumor recurrence and survival rates, with significantly improved outcomes in terms of treatment-related toxicity and cosmetic results in favor of the APBI arm. The IMRT-APBI Florence trial showed APBI delivered with external beam IMRT to be a safe and effective treatment option.6-7
Over the past decade, the Florence trial has guided the definition of treatment volumes, and the selection of planning dose constraints, bream arrangement, and treatment technique (non-coplanar IMRT) for external beam APBI.6 Volume-modulated arc therapy (VMAT) is a novel radiation technique, which can achieve highly conformal dose distributions with improved target volume coverage and sparing of normal tissues compared with conventional radiotherapy techniques. VMAT also has the potential to offer additional advantages, such as reduced treatment delivery time compared with conventional IMRT. The clinical worldwide use of VMAT is increasing significantly. Currently the majority of published data on VMAT are limited to planning and feasibility studies, although there is emerging clinical outcome data in several tumor sites.8 Additionally, modern linear accelerators have become capable of delivering both traditional flattened photon beams using flattening-filter (FF), as well as flattening filter-free (FFF) beams. These FFF beams have several advantages like increased dose rate, reduced the head scatter, less beam-on time and reduced out of field dose as compared to flattened beams.9 Despite the increased adoption of VMAT over static IMRT, the utilization of co-planar VMAT combined with FFF as a potential replacement technique for static field IMRT with flattened beam energies in the setting of APBI has not been examined. The aim of this study was to determine the optimal technique for APBI, with a focus on VMAT and FFF delivery (VMATFFF), and to offer support to planners interested in implementing this technique in their clinical practice. This is also the first comprehensive dosimetric report on APBI following the Florence trial6 that includes both co-planar VMATFFF and VMATFF delivery and is not limited to non-coplanar IMRTFF.
Patients
This single institution study was performed as follows: Ten patients previously treated according to the APBI-IMRT Florence trial were selected for evaluation.6 Selected patients included five left- and five right-sided targets. Patients were aged more than 40 years and diagnosed with early breast cancer (maximum diameter 2.5 cm) suitable for breast conserving surgery. Angio vascular invasion, ductal carcinoma in situ and axillary lymph node positive status were not considered exclusion criteria. For this retrospective planning study, the patients were selected randomly, with no selection criterion used, other than treatment type, to differentiate the study group and to avoid selection bias. The median patients’ age was 47 years (range 42–68).
Treatment planning
Patients received simulation CT scans (Somatom Sensation; Siemens, Germany) with a slice thickness of 3mm. The slices extended to completely cover the involved breast, lungs, and a 4 cm margin in the cranial and caudal directions. The targets and organ at risks (OARs), such as the normal lungs, heart, normal breasts, and spinal cord were contoured in respective CT slices based on the APBI-IMRT-Florence protocol. The clinical target volume (CTV) was delineated with a uniform 1-cm three-dimensional margin around the surgical clips. The CTV was limited to 3 mm from the skin surface and 3 mm from the lung–chest wall interface. A second uniform, three-dimensional 1-cm margin was added to the CTV to obtain the planning target volume (PTV). The PTV was allowed to extend maximum 4 mm inside the ipsilateral lung and was cropped 3 mm inside the patient’s surface. The ipsilateral and contralateral breast, ipsilateral and contralateral lung, heart, and spinal cord were contoured as OARs. No respiratory control was used. All of patients were planned for APBI treatment on a TrueBeam™ linear accelerator (Varian Medical Systems, Palo Alto, CA, USA) using 6 MV photon beams modulated with a multileaf collimator. Treatment plans were generated using inverse optimization planning, in the Eclipse™ planning system (Version 15.6, Varian Medical Systems, Palo Alto, CA, USA), which is the TPS clinically employed in our center for APBI planning. A dose of 30 Gy in five nonconsecutive, once-daily fractions at 6 Gy/fraction was prescribed.
Original, treated plans followed the methodology of the APBI-IMRT-Florence protocol6 and employed five non-coplanar sliding-window IMRT fields with a flattened 6MV beam energy (IMRTFF). Retrospective volumetric modulated arc therapy (VMAT) treatment plans were designed using a partial arc geometry. Arc extents were chosen to emulate an opposed tangential delivery. Specific start and stop angles were chosen per patient, and depended primarily on patient anatomy, including target and OAR locations. Typical beam arrangements for both IMRT and VMAT techniques are shown in Figure 1. Two retrospective VMAT plans were created for each patient. One utilized a flattened 6MV beam energy (VMATFF), while the other utilized a flattening filter free 6MV beam energy (VMATFFF). The Acuros XB algorithm was used for dose calculation, and tissue heterogeneity correction was used in all the treatment plans.
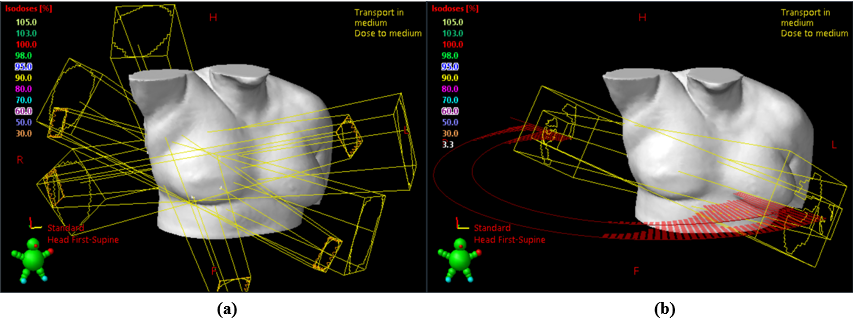
Figure 1 Example beam arrangement for Intensity-modulated radiation therapy (IMRT)(a) and Volumetric modulated arc therapy (VMAT)(b)
The following dosimetric constraints were adopted for plan optimization, matching previously published constraints6 and following departmental guidelines:
All plans were created by experienced medical physicists or dosimetrists. Planners introduced no additional dose control structures during the manual planning process. Sometimes it was not possible to meet the ideal constraint for at least one OAR or for the PTV during planning of clinical cases. In these cases, the patient was considered having to have an unfavorable or challenging anatomy, and a minor deviation from the ideal constraint was accepted by the approving physician (Figure 2&3).
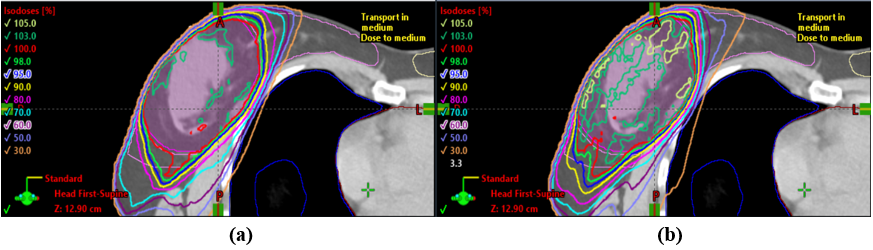
Figure 2 Example transverse plane 2D isodose distributions for the same patient for both IMRT (a) and VMAT (b). The prescription isodose line (30Gy) is show in red. 95% of the prescription isodose line (28.5Gy) is shown in blue. Planning target volume (PTV) is displayed in pink.
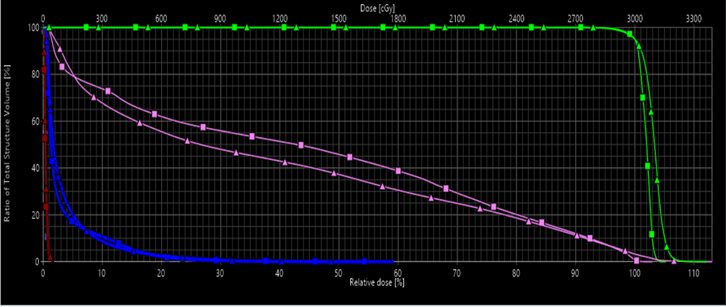
Figure 3 Example of PTV and organ at risk (OAR) dose-volume histogram comparison for IMRT vs. VMAT using flattening-filter (FF) beams. Displayed lines are as follows, green : PTV; pink : Ipsilateral normal breast: blue: ipsilateral lung ; dark red: heart; ▲: VMAT; ■: IMRT.
Plan evaluation and delivery time
The IMRTFF, VMATFF and VMATFFF treatment plans were compared objectively using dose‑volume histogram (DVH) information for the PTV and OARs. For the PTV, the maximum dose (Dmax) and volume receiving at least 95% of the prescription dose (V95%) were calculated. For the heart, the mean dose (Dmean) and the percent of the total volume receiving more than 3 and 0.5 Gy (V3Gy, and V0.5Gy) were compared. For the ipsilateral and contralateral lung, the percent of the total volume receiving more than 10 Gy and 5 Gy (V10Gy and V5 Gy) were compared. For the ipsilateral and contralateral breasts, the percent of the total volume receiving more than 15 Gy (V5Gy) and Dmax were compared, respectively. Treatment efficiency was evaluated by looking at total monitor unit (MU) counts and calculated delivery time. Delivery time was recorded by the machine record-verify system. The student’s t-test paired two sample for means was used to evaluate the significance of the differences seen. The significance level was set at p < 0.05. Statistical analyses were performed using Microsoft Excel®.
A comparison of the dosimetric results for each delivery technique (IMRTFF, VMATFF and VMATFFF) can be found in Table 1. The PTV coverage shows no difference by design because all plans were normalized so that 95% of the PTV volume was covered by 95% of the prescribed dose. However, both VMATFF and VMATFFF slightly increased Dmax for the PTV by approximately 5% of prescribed dose (~1.5Gy) compared with the IMRTFF (p=0.02). For the heart, the Dmean for both VMAT techniques was also slightly increased compared to IMRTFF by 3 and 6 cGy (p=0.07) for VMATFF and VMATFFF, respectively. However, the difference in V3Gy, and V0.5Gy were less than 0.5% and not statistically significant (p=0.23). For the contralateral lung, the entire volume received less than 5Gy for all three techniques. Both VMAT techniques demonstrated a significant 1-2% decrease in V10Gy for the ipsilateral lung compared with the IMRT technique (p=0.05). However, no significant difference was observed when V15Gy and Dmax for uninvolved breast (ipsilateral and contralateral) were compared (p>0.15). The average number of MU per fraction needed to deliver 6 Gy for the IMRTFF and VMATFF techniques was 1455±122 and 1053±83 counts, respectively, demonstrating a significant difference (p= 0.01). VMATFFF plans also showed a decrease in required MU compared to IMRTFF, though at 1123±62MU, the average was slightly higher than VMATFF. Despite this slight increase in total MU compared to VMATFF, the 1400 MU/min maximum dose rate of the FFF beam compared to 600 MU/min for the FF beam made VMATFFF the most efficient modality of those evaluated. Co-planar VMATFFF offered a significant reduction in beam-on time compared to non-coplanar IMRTFF (83±3 v.s. 458±94s, p=0.05).
|
|
Heart |
Lung |
Uninvolved Breast |
PTV |
MU |
Treatment Time (sec) |
||||
|
Ipsilateral |
Contralateral |
Ipsilateral |
Contralateral |
|||||||
|
Dmean (cGy) |
V3Gy(%) |
V0.5Gy(%) |
V10Gy (%) |
V5Gy (%) |
V15Gy (%) |
Dmax (cGy) |
Dmax (%of Rx) |
|||
|
Intensity modulated radiation therapy + flattened beams (IMRTFF) |
17.4±6.6 |
0.3±0.7 |
0.4±0.6 |
4.3±2.7 |
0.0±0.0 |
37.4±6.4 |
29.4±8.2 |
105.1±0.7 |
1455±122 |
458±94 |
|
Volumetric modulated arc therapy + flattened beams (VMATFF) |
20.8±11.8 |
0.1±0.1 |
0.3±0.4 |
2.6±1.4 |
0.0±0.0 |
28.8±5.9 |
24.8±17 |
111.1±3.3 |
1053±83 (p=0.01) |
92±2 (p=0.03) |
|
Volumetric modulated arc therapy + flattening filter free beams (VMATFFF) |
23.5±9.5 |
0.0±0.0 |
0.3±0.4 |
2.9±1.5 |
0.0±0.0 |
28.8±5.9 |
27.4±6.3 |
110.1±2.3 |
1123±62 (p=0.01) |
83±3 (p=0.05) |
|
VMATFF-IMRT-FF (%/cGy) |
6.3±3.5 |
-0.3±0.8 |
-0.2±0.7 |
-1.6±2.3 |
0.0±0.0 |
-8.6±4.7 |
-4.6±16.7 |
6.1±3.3 |
-403±175 |
-366±94 |
|
VMATFFF-IMRT-FF (%/cGy) |
6.1±3.9 |
-0.4±0.7 |
-0.2±0.6 |
-1.4±1.6 |
0.0±0.0 |
-10.0±4.9 |
-6.7±6.6 |
5.3±2.4 |
-333±153 |
-375±87 |
Table 1 Comparison of dosimetric parameters and treatment efficiency of Intensity-modulated radiation therapy (IMRT) using flattening filter (FF) beam and Volumetric modulated arc therapy (VMAT) using both flattening filter (FF) and flatten-filter free (FFF) beam for accelerated partial breast irradiation (APBI)
Abbreviations: PTV, planning target volume; MU, monitor unit; Dmax, maximum dose; Dmean, mean dose; VxGy, organ volume receiving; xGy; Rx, Prescription
For this study, target coverage was ensured for each technique examined by normalizing each plan so that at least 95% of the PTV received 95% of the prescription dose. All plans demonstrated maximum doses less than 110% (33Gy) of the prescribed dose. These constraints were based on the APBI-IMRT-Florence trial protocol.6 The IMRTFF technique achieved the best plan homogeneity of all techniques examined, with an average maximum dose of less than 105%. Both VMATFF and VMATFFF achieved better conformity compared to IMRTFF, however the differences were not significant. This is likely due to the inverse optimization process, which is used for both IMRT and VMAT, allows for improved conformity. These results are like those found by Marrazz et al.10 in their published the updated to the APBI Florence trial. Here they suggest the maximum dose to the PTV be changed from 105% of prescribed dose when using a static IMRT technique to 110% of prescribed dose when using a VMAT technique.
For the 10 patients randomly selected for this study, the median tumor bed size was 17.3 cm3 (5–40 cm3). Tumor bed size is a predictor of outcomes in existing literature examining external beam APBI. It has been previously shown that total target volume (PTV) is a predictor of cosmetic results. This is because it is essential the target volume receives the prescribed dose, which may lead to subpar cosmetic results for large targets.4-7 The dose of ipsilateral normal breast (on the same side, outside the PTV) should be kept low to achieve good cosmetic results. According to APBI-IMRT-Florence protocol the volume of normal ipsilateral breast receiving 50% of the prescribed dose should remain below 50% (V15 Gy <50%).6 A retrospective study by Meattini et al.7 found that for the normal ipsilateral breast, a threshold of V15Gy > 40% was predictive of worse cosmetic results. Our results showed both VMAT techniques performed significantly better than IMRT at minimizing dose to the normal ipsilateral breast. With both VMATFF and VMATFFF showing average V15Gy values of 29%, compared to 37% for IMRTFF (Table 1). This may indicate that, especially for large PTVs, VMAT may offer improved cosmetic results compared to IMRTFF. Minimization of dose to the uninvolved contralateral breast is also of great importance to reduce the risk of secondary malignancy. The Florence trial recommends a maximum dose to the contralateral breast of less than 100cGy.6 In our study, the average maximum dose to the contralateral breast was approximately 5cGy less when using VMATFF or VMATFFF compared to IMRTFF. However, both IMRT and VMAT produced contralateral breast doses well below 100cGy. For the ipsilateral lung, both VMAT techniques were better able to reduce the V10Gy compared to IMRTFF. Both IMRTFF and both VMAT techniques were able to reduce the V5Gy of the contralateral lung to 0%. Cardiac doses for each technique were satisfactory. To better determine the effect of technique on cardiac dose, right and left-sided cases were examined separately. IMRTFF, VMATFF, and VMATFFF produced similar results for heart Dmean, D3Gy and D0.5Gy. At the low cardiac doses described in our study, both early and late cardiac side effects are not described in the literature.4-7 Overall, VMAT was shown to improve or maintain the doses delivered to all examined organs at risk compared to IMRT, including the ipsilateral normal breast, contralateral breast, ipsilateral and contralateral lung, and heart. This echoes a previous study,4 which demonstrated that VMAT is a good technique for APBI compared to 3D conformal radiotherapy (3DCRT), improving PTV dose conformity and delivering lower doses to the ipsilateral breast and lung, at the cost of a slight but acceptable increase in the contralateral breast dose. Moreover, VMAT was shown to reduce cardiac dose if mean heart dose exceeded 0.5Gy.
While plan quality is an important aspect of treatment technique selection, practically important factors, such as the number of monitor units (MUs), treatment time, deliverability, and patient comfort are also critical to ensure successful delivery. In terms of the number of monitor units, both VMAT techniques proved to be significantly superior to IMRT (approximately 25% less) (Table 1). A reduction in MUs improves treatment efficiency and may reduce out of field radiation scatter dose to uninvolved areas of the patient. Static field IMRT also requires couch rotations to create an acceptable dose distribution. Unfortunately, the introduction of couch rotations has serious practical disadvantages. Treatment time is increased. Furthermore, because additional table motions may cause the patient’s body to react involuntarily, the possibility of intra-fractional patient displacement also increases. Treatment planning may also be more challenging, as the planner must consider which gantry and table angle combinations may result in patient-gantry or table-gantry collision issues. Additional staff and machine time may be required to verify deliverability prior to patient arrival. The of a VMAT delivery technique significantly shorten in the treatment time compared to IMRT by an average of one and a half minutes. This reduction in treatment time is multi-factorial. As mentioned previously, IMRT must be delivered in a non-coplanar fashion, while VMAT requires no table rotation. Modern accelerators can deliver the required VMAT arcs without interruption. VMAT also requires fewer MUs. Finally, the addition of FFF introduces additional time savings. FFF beam energies boast dose rates significantly higher than traditional flattened beams ((1400MU/min (VMATFFF) vs 600MU/min (IMRTFF &VMATFF)). It should be noted that FFF beam energies are not limited to the VMAT technique and may also offer time savings if incorporated into a non-coplanar IMRT approach. It should also be noted that the use of FFF beam energies may increase the total number of MUs. This is because FFF beam profiles are non-uniform, with a maximum dose rate along central axis, decreasing toward the periphery. As a result, delivery of dose distant from central axis requires additional MUs. FFF beams also require additional modulation to produce a uniform dose distribution over a large volume, further increasing the total number of MUs. However, these increases are typically small compared to the significant increase in dose rate FFF offers. The time-savings afforded using VMATFF and VMATFFF may be especially important for patients treated under breath hold conditions. Patient comfort is increased by decreasing the amount of time required under breath hold conditions. Minimizing the duration and number of breath-holds required may also help improve reproducibility and reduce the probability of both external and internal motion during treatment. This is critical for ensuring appropriate target coverage and OAR avoidance.
Concerning standardization of plan quality for future study in APBI, a reduction in plan variability is also critical factor to maintain the plan quality index. The treatment planning of IMRT and VMAT has become more labor intensive, requiring hours or even days of planner effort to optimize an individual patient case in a trial-and-error fashion. More recently, artificial intelligence (AI) has been utilized to automate and improve various aspects of medical science. Auto-planning with AI will be included the future study of APBI to improve the plan quality standardization.
External beam accelerated partial breast irradiation has been shown to be an effective and efficient course of treatment for appropriate patients. APBI treatment planning offers challenges due to the proximity of OARs, the need for target conformity, and steep dose gradients. Historically, static-field IMRT with flattened beam energies has been used to create these challenging plans. This work provides a comprehensive analysis of the dosimetric parameters observed for IMRTFF in addition to two VMAT techniques (VMATFF and VMATFFF) for right and left-sided APBI. The VMAT techniques allow for similar target coverage with a slight decrease in target dose homogeneity compared to IMRTFF. OAR dose remained similar for all three techniques, with VMATFF and VMATFFF showing a slight decrease in normal ipsilateral breast V15Gy and ipsilateral lung V10Gy. As a result, no difference in side effect profile is expected. However, the co-planar VMAT techniques significantly reduced treatment time and complexity compared to IMRTFF, with VMATFFF offering the greatest reduction in treatment time. As a result, the use of VMATFFF may lead to improved setup reproducibility and a reduction in intra-fractional patient motion, especially for patients treated under breath hold conditions. Co-planar partial-arc VMATFF and VMATFFF techniques produced equivalent target coverage, improved MU efficiency, better or equivalent normal tissue sparing, and shorter delivery time compared to non-coplanar IMRTFF technique and are a suitable replacement for non-coplanar IMRTFF for the treatment of external beam APBI.
No financial support was provided for this study. All authors have no disclosures or conflicts of interest to declare.
None.
None.

©2023 Peng, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.