International Journal of
eISSN: 2574-8084


Research Article Volume 6 Issue 6
Department of Radiology, Faculty of Medicine Universitas Airlangga, Dr. Soetomo General Academic Hospital, Indonesia
Correspondence: Fransisca Rika Andriani, Department of Radiology, Airlangga University, Perum Galaxi Bumi Permai N4-42, Indonesia, Tel +62 877-0333-0249/+62 815-5313-8138
Received: October 16, 2019 | Published: November 5, 2019
Citation: Utomo SA, Andriani FR. Does tumor size, peritumoral edema, location and necrosis can be used to predict grading of meningioma? Int J Radiol Radiat Ther. 2019;6(6):195-198. DOI: 10.15406/ijrrt.2019.06.00246
Background: Meningioma based on WHO classification divided into grade I (typical or benign, 88-94%), grade II (atypical, 5-7%) and grade III (anaplastic or malignant, 1-2%).1 Treatment of meningioma is tailored to their histological grade.2
Objective: The purpose of this study was to examine whether imaging features included tumor size, peritumoral edema, location and necrosis on conventional MRI could be used to predict grading of meningioma.
Method: We performed a retrospective review of 20 patients which histopathologically confirmed after surgical resection, who where imaged with MRI at our institution from 2016 until 2019. Image features of each sample include tumor size, peritumoral edema, location and necrosis was analysed and correlate with WHO histopathological grading.
Result: In our study from 20 patients, age range from 21 to 67 years old, 16 female, 4 male, 16 classified as WHO grade I, 3 grade II, and 1 grade III, with histopathology mostly transitional type. Tumor volume ranges from 17-252.4cm3 in grade I, 28.5-143cm3 in grade II & 190cm3 in grade III, necrosis present in 44% of grade I, 33% of grade II and 100% of grade III. Based on location from 16 cases of grade I, mostly in convexity, 2 out of 3 grades II in skull base and 1 case of grade III in convexity. In WHO grade I, 44% have severe edema and conversely case of grade III have mild edema.
Conclusion: Imaging features of tumor size, peritumoral edema, location and necrosis broadly varied in each grade of meningioma, Advanced MRI such as DTI should be study to found more promising predictor.
Keywords: meningioma, tumor, peritumoral edema, necrosis
Background
Meningioma based on The World Health Organization (WHO) classification divided into WHO grade I, which are typical or benign (88–94%), WHO grade II, which are atypical (5–7%) and WHO grade III, which are anaplastic or malignant (1–2%). WHO II/III tumors are far more likely to recur than benign meningioma, even when resected completely, and often require adjuvant radiation.1 Patients with radiographically detected meningioma are either observed or undergo surgical resection. Surgical treatment is usually recommended for patients with neurologic symptoms, large tumors, and/or associated cerebral edema. However, patients with more aggressive WHO II/III meningiomas could benefit from early resection even in the absence of these clinical and radiographic features.2 It is quite simple to diagnose meningioma with characteristic imaging findings in conventional MRI. However, the ability of conventional MRI to differentiate low-grade from high-grade meningioma remains uncertain. Some studies have reported that conventional MRI findings are not specific and reliable in identifying meningioma grade.3−5 Previous studies have not found a single specific criterion predictive of atypical meningioma, despite an impressive battery of studies examining clinical presentation, imaging results, and immunohistochemical studies. Thus, a non-invasive diagnostic method that can differentiate between low and high-grade meningioma is required.6 Previous study by Hale et al in 2017 of 128 patients with meningioma, tumor volume was the strongest predictor of atypical meningioma and peritumoral edema as predictor of higher grade meningioma. In that study also found that tumor along the falx and convexity were more often atypical than in skull base or posterior fossa and tumor necrosis was associated with an increased risk for atypical meningioma.7
The purpose of this study was to examine whether imaging features included tumor size, peritumoral edema, location and necrosis on conventional MRI really could be used to differentiate between low and high-grade meningioma.
Patients
We performed a retrospective review of 20 patients which histopathologically confirmed after surgical resection, who where imaged with MRI at our institution from 2016 until 2019. These patients were derived from a retrospective research database, and patients without adequate preoperative imaging were excluded. Predictive factors related to atypical meningioma, including patient age and sex, tumor pathology, and imaging features were collected from the electronic medical record and analyzed. All meningiomas were histopathologically graded after surgical resection by a board-certified neuropathologist according to WHO guidelines.
Imaging techniques
MR imaging studies were performed on MR360 Optima 1.5T GE, TR 5000-7000ms; TE 100-200ms, 5.0 mm section thickness, spacing 5.0 mm and image processing had done with GE advance windows workstation (GE software volume share 5). All patients received intravenous gadolinium contrast (gadopentetate dimeg- lumine, Wayne, New Jersey, USA) administered at 0.1 mmol per kilogram.
Image analysis
MRI images were evaluated for tumor location, the presence and extent of edema surrounding the tumor, volume of tumor, and whether the tumor had central necrosis followed the criteria that were used in Hale et al study. In their study, peritumoral edema was graded using the following scale: (0) No edema: absence of increased T2 signal surrounding the meningioma. (1) Mild edema: rim or crescent of increased T2 signal surrounding the meningioma without mass effect. (2) Moderate edema: more extensive increased T2 signal surrounding the meningioma without mass effect. (3) Severe edema: mass effect from edema and/or tongues of advancing edema. Tumor location was grouped in the following categories: (1) Convexity (including frontal, parietal, temporal, lateral sphenoid wing, and petrous) (2) Skull base (including sellar/suprasellar/anterior clinoid, cavernous/medial sphenoid wing, and fovea ethmoidalis) (3) Falx (4) Posterior fossa (including tentorium, cerebellum, and cerebellar pontine angle). Tumor volume was calculated using manual tracing of multiple planes in the imaging viewer.2
In our study from 20 patients, age range from 21 to 67 years old, 16 female, 4 male, 16 classified as WHO grade I, 3 grade II, and 1 grade III, with histopathology mostly transitional type. The histopathological subtypes of the 20 meningiomas studied were 2 microcystic, 1 anaplastic, 1 microcystic and angiomatous, 2 fibroblastic mixed microcystic, 2 atypical, 1 meningothelial, 7 transitional and 4 fibroblastic type. Tumor volume ranges from 17-252.4cm3 in grade I, 28.5-143cm3 in grade II and 190cm3 in grade III. In study by Hale et al., tumor volume were not graded, in our study we categorised tumour volume samples into more than 50 cm3 and less than 50 cm3. From this study we got 6 (37.5%) of WHO grade I, 2 out of 3 (66.7%) of WHO grade II and 1 sample of WHO grade III is more than 50 cm3 in size. In WHO grade I, 44% have severe edema and conversely 1 case of WHO grade III have mild edema. The rest of WHO grade I, 6 (37.5%) have mild edema, 3 (18.7%) have moderate edema and 3 cases of WHO grade II each varied has mild, moderate and severe edema. Necrosis is present in 44% of grade I, 33% of grade II and 100% of grade III. Based on location from 16 cases of grade I, mostly (37.5%) in convexity, 3(18.75%) in skull base, 4(25%) in falx and 3 (18.75%) in posterior fossa. 2 out of 3 grades II were in skull base, 1 in falx and 1 case of grade III was in convexity. All of the analysed image features was summarized in Table 1.
|
Imaging features |
Meningioma |
||
|
WHO grade I |
WHO grade II |
WHO grade III |
|
|
Tumor size |
17-252.4cm3 |
28.5-143cm3 |
190cm3 |
|
Peritumoral Edema |
44% severe edema |
mild to severe edema |
mild edema |
|
Location |
mostly in convexity |
2 out of 3 in skull base |
convexity |
|
Necrosis |
44% |
33% |
100% |
Table 1 Image features analysed based on meningioma grading
In our study showed that tumor volume as suggested by Hale et al. as the strongest predictor of atypical meningioma, didn’t always correlate with meningioma grade. In our samples there were 6 (37.5%) meningioma WHO grade I with tumor volume more than 50 cm3, with the biggest volume 252.4cm3 (Figure 1) and 1(33%) of atypical meningioma (WHO grade II) with tumor size 28.5 cm3. Hale also suggested that peritumoral edema as predictor of higher grade meningioma. In our study we found 1 case of anaplastic meningioma (WHO grade III) with mild edema and conversely, 44% of meningioma WHO grade I with severe edema (Figure 2). In that study also found that tumor along the falx and convexity were more often atypical than in skull base or posterior fossa. In this study, samples of meningioma WHO grade I mostly (37.5%) located in convexity, 25% in falx and in atypical meningioma WHO grade II turned out 67% located in skull base (Figure 3). That study also found that tumor necrosis was associated with an increased risk for atypical meningioma. In this study, we found 67% of atypical meningioma WHO grade II without tumor necrosis and 44% of typical meningioma WHO grade I with tumor necrosis (Figure 4). 1 case of anaplastic meningioma (WHO grade III) in our study had large tumor volume (>50 cm3), located in convexity and with tumor necrosis although there was one predictor that didn’t suit which in this case had mild peritumoral edema (Figure 5).
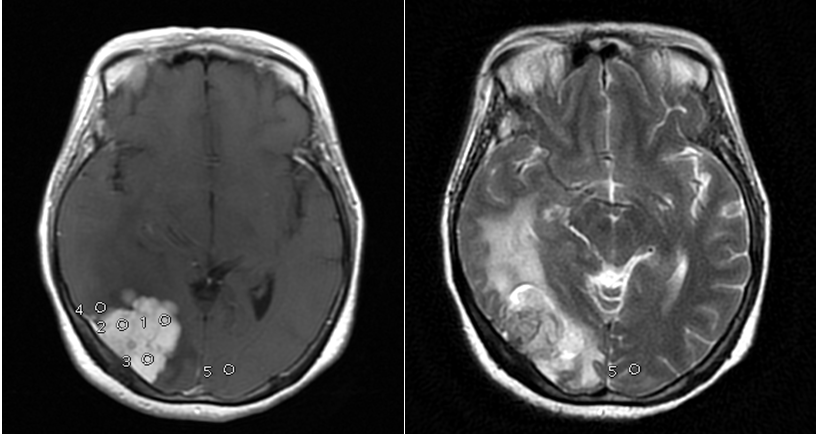
Figure 2 Female, 45 y.o with meningioma at right occipital convexity, tumor vol 26,2 cm3 surround with severe edema turned out as fibroblastic and microcystic type, WHO grade I.
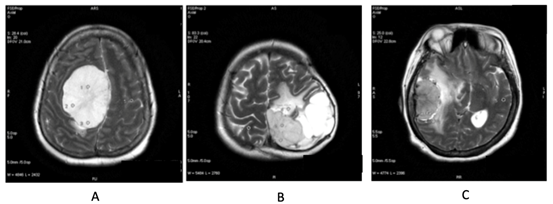
Figure 3 (A) Meningioma at parasagital falx cerebri, fibroblastic type, WHO grade I. (B) Meningioma at left falx cerebri, microcystic type, WHO Grade I. (C) Meningioma at right temporal convexity, turned out to be microcystic type, WHO Grade I.
None.
None.
Author declares that there are no conflicts of interest.

©2019 Utomo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.