International Journal of
eISSN: 2574-8084


Research Article Volume 6 Issue 4
1CT Department, Elpis General Hospital, University of West Attica, Greece
2CT & MRI Department, General Children Hospital Agia Sofia, Athens University of West Attica, Greece
3Radiography & Diagnostic Imaging, School of Medicine, University College Dublin, Ireland
4Blood Center and National Centre for Congenital Bleeding Disorders, Laiko General Hospital and Faculty of Social Sciences, Department of Health Management, Hellenic Open University, Greece
5Associate Professor TEI of Thessaly, 404 Military Hospitals, Tutor Hellenic Open University, Greece
6Nursing Department, School of Health Sciences, Cyprus University of Technology, and Faculty of Social Sciences, Department of Health Management, Hellenic Open University, Greece
Correspondence: Dousi M, CT Department, Elpis General Hospital, University of West Attica, Greece, Tel 6973926302
Received: June 26, 2019 | Published: July 12, 2019
Citation: Dousi M, Syrgiamiotis V, McNulty JP, et al. Diagnostic reference levels as a tool to identify differences in practice among Greek computed tomography departments. Int J Radiol Radiat Ther. 2019;6(4):121-126. DOI: 10.15406/ijrrt.2019.06.00231
Purpose: To identify differences in practices across CT departments for the same examinations based on the diagnostic reference levels (DRLs).
Methods: Data from 420 patients, seven participating public hospitals, which had multi-slice CTs, ranging from 2 to 128 slices and three types of examinations were collected during a 6-month period. A statistical analysis was performed between the centers that had the same CT scanner. 75th percentile of CTDIvol and DLP of each hospital were calculated in order to determine Local DRLs.
Results: Abdomen/pelvis examination had the largest difference between the minimum and maximum mean doses, of 312% for the CTDIvol index and 296% for the DLP. The chest examination was recorded a difference of 163% for the CTDIvol and 166% for the DLP, and the head examination was last with a 127% difference for the CTDIvol index and 157% for the DLP. There is a statistically significant difference in the dose indexes CTDIvol and DLP between the same 128 slice units for the examination of Head (CTDIvol: p=0.000, DLP: p=0.000) and Chest (CTDIvol: p=0.000 DLP: p=0.001) but not for the examination of Abdomen/Pelvis (CTDIvol: p=0.709 DLP: p=0.747) and between the same 16 slice
units for the examination of Chest (CTDIvol: p=0.000, DLP: p=0.000) but not for the examination of Head (CTDIvol: p=0.517, DLP: p=0.685) and the examination of Abdomen/Pelvis (CTDIvol: p=0.808, DLP: p=0.417).
Conclusion: Based on local DRLs, for the three CT examinations, the dose variations between departments, with similar CT scanners, suggest great potential for optimisation.
Keywords: computed tomography, diagnostic reference levels, optimisation, dosimetry
The most important source of radiation from medical applications is CT, which represents about 7% of all radiological processes worldwide, while accounting for 40% of the collective effective dose of the population.1 CT is associated with relatively high doses of radiation, leading to a corresponding increase in cancer risk factor.2 It has been suggested that 20-50% of radiation exposure for medical reasons may not be necessary and the level of training of doctors for correct referral is linked to excessive use.3 Calculations suggest that CT scans, for example in the US in 2007, can cause up to 29,000 cancers in the future, about 6% of them in the breast and the rest in the lungs, brain and other organs.4 Although this risk for an individual patient may be small, the increasing number of people exposed to this radiation, combined with an increasing exposure per exam, could be translated into many cancer cases, due exclusively to exposure to radiation by CT.5 The typical dose of radiation in a CT scan is associated with a risk of developing lethal cancer of approximately one per 2,000 CT scans. In a few decades the rate of carcinogenicity from CT could reach up to 2% of all cancers, as opposed to the currently estimated 0.4%. Radiation exposure from three or four CT scans is roughly equivalent to that experienced by survivors of the atomic bomb in Japan, who were 1-2 miles away from the "zero point".5
The European Council, taking into account the International Basic Safety Standards (BSS) for Protection against Ionising Radiation and for the Safety of Radiation Sources,6 introduced the concept of diagnostic reference levels (DRLs).7 DRLs are an important tool for radiation protection of patients and refer to dose values, which are recommended as the highest possible, within which the optimisation principle can be achieved. There are several techniques for optimising CT protocols.8,9 Optimisation aims to reduce the dose of radiation by maintaining a diagnostically acceptable result with the lowest radiation dose through the gradual modification of exposure parameters to reduce exposure to radiation, but without compromising the quality of imaging.10 DRLs can contribute to recognition situations where the patient's dose levels are unusually high.11 DRLs defined in radiological practices to standard-sized groups of patients or standard phantoms. Computed tomography dose index (CTDI) and dose length product (DLP) for different types of examinations are used to express the DRLs.9 The importance of DRLs is emphasised in the new European Basic Safety Standards Directive (Council Directive 2013/59/Euratom), which requires that the age and gender distribution of the exposed patient population be taken into account.12,13 DRLs are usually set to the third quartile or 75th percentile. This makes a compromise between an excessively stringent and an overly low value. Essentially, if the average doses exceed a dose level of a reference level, a check may be made to ascertain the cause and take corrective action if the dose was not clinically justified.14 DRLs may result in dose reduction to the patient among different scanners and prevent systematic radiation overexposures from CT examinations, as has occurred at other studies.15,16 It has been shown that the use of DRLs reduces the overall dose in clinical practice.17,18 In Greece,DRLs have been incorporated into Greek Law and amended to national DRLs in 2014.19 This study aims to identify differences in practices across CT departments for the same examinations based on the DRLs.
Α total of seven hospitals (a total of 3.855 beds) were investigated (23,3% from public adult hospitals of Athens), including four general hospitals (20% of general hospitals of Athens), two oncology centres (75% of public oncology centers of Athens) and one adult university teaching hospital (50% of university teaching hospital of Athens) and data were collected from a total of 420 patients. These hospitals have multi-slice CT scanners and data were collected for six months period, from June 2017 to December 2017. The data were collected using a form based on the UK DRLs CT dose survey data acquisition form.14 Parameters for at least 20 mean patients for each CT scan over the six-month period were recorded. Patients were deemed of average size if they weighed 60–80 kg. Therefore, adult patients weigh 70 (±10 kg) who underwent the routine CT scan (head, chest, abdomen/pelvis), were enrolled in the study. The weight of the patients was measured before the examination, using electronic scales found in all computed tomography departments. The sample of patients was randomized. 73% were collected during the morning shift and involved patients with scheduled examinations, while the remaining 27% was collected during the afternoon and night shifts and related to incidents considered urgent.
All CT scanners perform daily calibration. All CT units are subjected to the necessary annual quality control procedures. Five out of seven CT units (A, B, E, F, G) are subjected to the appropriate monthly and weekly quality controls tests. Two (C, D) out of seven follows the testing procedure twice a month. None of the units perform daily quality control apart from detector calibration. Athens was chosen because it is the capital of Greece and the largest urban center in the country, where half its population live. Consequently, these hospitals receive large volumes of patients annually. All hospitals have CT scanners that incorporate modern dose reduction technologies and provide information on exposure to patients. Multiphase studies with or without the use of contrast media were excluded from the study. This study concerns tests that included only one scan phase. There was no adaptation to the scan protocols used by all hospitals prior to this study. This was to ensure that the study reflects daily practice in all hospitals. The data recorded concerned the type of CT, the type of examination, the use of contrast media, the demographics of the patients (sex, weight, age), the use of reduction dose methods (specifically the use of tube current modulation) and the CTDIvol and DLP indexes.
The eligibility criteria for the study are as follows:
All hospitals gave permission for data to be collected and used for this study. Confidentiality was ensured by making sure patient identifiers and the hospital name was not included in the data form. Statistical analysis was performed using SPSS (Version 23). 75th percentile for dose indexes CTDIvol and DLP was used to calculate DRL for each of the seven participating centres and then compare this data in order to determining local DRLs for differences. Quantitative variables were expressed by descriptive analysis to summaries and show data variability for study at mean value, median value, range, and standard deviation. For the two hospitals (C and F) with 128 slices scanners and the examination of Head, the Kolmogorov-Smirnoff and Shapiro-Wilk tests showed that both the CTDIvol and DLP variables follow a normal distribution for a 5% significance level. Therefore, the parametric control of t-test was used. Additionally, for the Chest examination, the Kolmogorov-Smirnoff and Shapiro-Wilk tests showed that CTDIvol variable does not follow a normal distribution but DLP variable follows a normal distribution for a 5% significance level. Therefore, the non-parametric control of Mann–Whitney was used for CTDIvol and t-test was used for DLP. Finally, for the examination of the Abdomen/pelvis, the Kolmogorov-Smirnoff and Shapiro-Wilk tests showed that both CTDIvol and DLP variables follow a normal distribution for a 5% significance level. Therefore, the parametric control of t-test was used.
For the two hospitals (B and G) with 16 slices scanners and the examination of Head, the Kolmogorov-Smirnoff and Shapiro-Wilk tests showed that both the CTDIvol and DLP variables do not follow a normal distribution for a 5% significance level. Therefore, the non-parametric control of Mann–Whitney was used. Additionally, for the Chest examination, the Kolmogorov-Smirnoff and Shapiro-Wilk tests showed that CTDIvol variable does not follow a normal distribution but DLP variable follows a normal distribution for a 5% significance level. Therefore, the non-parametric control of Mann–Whitney was used for CTDIvol and t-test was used for DLP. Finally, for the examination of the Abdomen/pelvis, the Kolmogorov-Smirnoff and Shapiro-Wilk tests showed that both the CTDIvol and DLP variables do not follow a normal distribution for a 5% significance level. Therefore, the non-parametric control of Mann – Whitney was used.
47.1% of the patients were female and 52.9% were male. The weight of the participants ranged from 60 to 80 kg, and the average weight was 72.6 kg. Individual hospitals are denoted by letters A, B, C, D, E, F (Table 1). Of the 420-patient data collected, 140 were head examinations (33.3% of data), 140 were chest examinations (33.3% of data) and 140 were abdomen/pelvis examinations (33.3% of data). The age of the patients enrolled in the study ranged from 18 to 103 years, with a mean of 67.3 years for head routine exam, 63.7 years for chest routine exam and 62.81 for Abdomen/pelvis routine exam. All hospitals perform a helical examination technique on the head, except for the hospital, with the two slice CT scanner, where both axial and helical scanning techniques are performed. For reasons of uniformity of comparisons and accuracy of data, axial head examinations were excluded from this hospital. Therefore, this study investigated the helical scan technique for examining the head. The median CTDIvol and DLP per CT examination were calculated for each hospital and used to compare doses between them. The examination of abdomen/pelvis had the largest difference between the minimum and maximum average doses, of 312% in the CTDIvol index and 296% in the DLP index. The chest exam was followed, which recorded a difference of 163% for the CTDIvol index and 166% for the DLP index, and the head examination was last with a 127% difference for the CTDIvol index and 157% for the DLP index. The results of the CTDIvol and DLP values are summarized in Table 2. As can be seen from the data (Figures 1&2), the two slices CT scan recorded the lower CTDIvol and DLP for all types of examinations. There are large differences between CTDIvol and DLP indexes in the sample hospitals.
|
Hospital |
Type of hospital |
Number of beds |
Number of scanners |
Scanner name/model |
Collimation (mm) |
|
A |
General Hospital |
260 |
01-Jan |
Siemens Somatom Emotion Duo |
2×1 |
|
2 slice |
|||||
|
B |
General Hospital |
760 |
01-Jan |
Philips |
16×0.75 |
|
Brilliance 16 slice |
|||||
|
C |
General Hospital |
600 |
01-Jan |
Siemens Definition AS Plus |
128x0.6 |
|
128 slice |
|||||
|
D |
General Hospital |
550 |
01-Jan |
Toshiba Aquilion Prime |
128x0.5 |
|
128 slice |
|||||
|
E |
Oncology Centre |
450 |
02-Jan |
Toshiba Aquilion 64 slice τομών |
64x0.5 |
|
F |
Oncology Centre |
500 |
01-Jan |
Siemens Definition AS Plus |
128x0.6 |
|
128 slice |
|||||
|
G |
University Teaching Hospital |
735 |
02-Jan |
Philips |
16x0.75 |
|
Brilliance 16 slice |
Table 1 Hospitals and CT scanners included in the study
|
Head |
Chest |
Abdomen/Pelvis |
||||
|
CTDIvol |
DLP |
CTDIvol |
DLP |
CTDIvol |
DLP |
|
|
n |
140 |
140 |
140 |
140 |
140 |
140 |
|
Mean |
46,98 |
790,28 |
6,52 |
231,56 |
11,02 |
509,16 |
|
SD |
16,89 |
309,32 |
3,08 |
109,51 |
6,13 |
274,54 |
|
Min |
26,63 |
326,44 |
2,99 |
87,00 |
2,14 |
81,87 |
|
Maχ |
104,60 |
1888,30 |
14,80 |
545,20 |
29,90 |
1848,80 |
|
75th percentile |
50,10 |
919,30 |
9,08 |
309,50 |
13,19 |
646,20 |
Table 2 Summary of CTDIvol and DLP results for the selected examinations
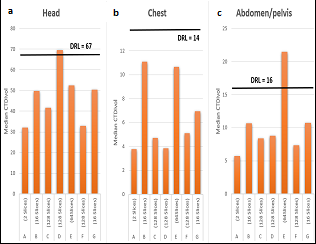
Figure 1 Distribution of the CTDIvol dose index for the CT scan examinations for each CT Unit. (A) Distribution of Median CTDIvol for head CT scan. (B) Distribution of Median CTDIvol for chest CT scan. (C) Distribution of Median CTDIvol for abdomen/pelvis ventricular CT scan. National (Greek) DRLs are shown for each.
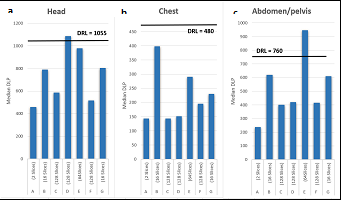
Figure 2 Distribution of the Median DLP dose index for the CT scan examinations. (A) Distribution of Median DLP for head CT scan. (B) Distribution of Median DLP for chest CT scan. (C) Distribution of Median DLP for abdomen/pelvis ventricular CT scan.
(Greek) DRLs are shown for each
Also, in one hospital (Hospital D), dose ratios are exceeded in relation to the National DRLs of Greece for head examination and in another hospital (Hospital E) the dose indexes for abdomen/pelvis examination are exceeded. Only the dose values of chest examination in all the hospitals examined were within the National DRLs that Greece has instituted. There are two groups of hospitals (B, G with 16 slices CT scanner and C, F with 128 slices CT scanner), which have identical type of scanners in the study and this allows for a rough comparison between the protocols used in Greece, from exactly the same model but in different centers. We conducted a statistical analysis to investigate whether the differences between the two groups of hospitals were statistically significant. For two hospitals (C and F) with 128 slices scanners and the examination of Head, the statistical analysis with t-test showed that there are statistically significant dose differences between the two hospitals (CTDIvol: p=0.000, DLP: p=0.000). Additionally, for the Chest examination, the statistical analysis of Mann – Whitney test for CTDIvol and t-test for DLP showed that there are statistically significant dose differences between the two hospitals (CTDIvol: p=0.000, DLP: p=0.001). Finally, for the examination of the Abdomen/pelvis, the statistical analysis with t-test showed that there are no statistically significant dose differences between the two hospitals (CTDIvol: p=0.709, DLP: p=0.747).
For the two hospitals (B and G) with 16 slices scanners and the examination of Head, the non-parametric control of Mann – Whitney showed that there are no statistically significant dose differences between the two hospitals (CTDIvol: p=0.517, DLP: p=0.685). Additionally, for the Chest examination, the statistical analysis of Mann – Whitney test for CTDIvol and t-test for DLP showed that there are statistically significant dose differences between the two hospitals (CTDIvol: p=0.000, DLP: p=0.000). Finally, for the examination of the Abdomen/pelvis, the non-parametric control of Mann – Whitney showed that there are no statistically significant dose differences between the two hospitals (CTDIvol: p=0.808, DLP: p=0.417). The 75th percentile was calculated from dose indexes for all 7 hospitals in order to defined Local DRLs. Table 3 shows local DRLs values for seven CT units from this study compared to those from other studies, while Table 4 shows scan parameters for CT departments of the sample hospitals.
|
ACR (2016) |
EU (2014) |
UK (2014) |
Greece (2014) |
Local DRL of participating hospitals |
|||||||
|
Head |
|||||||||||
|
A |
B |
C |
D |
E |
F |
G |
|||||
|
CTDIvol |
56 |
60 |
60 |
67 |
35 |
50 |
44 |
102 |
52 |
34 |
51 |
|
DLP |
962 |
1000 |
970 |
1055 |
525 |
847 |
653 |
1641 |
1052 |
583 |
943 |
|
Thorax |
|||||||||||
|
CTDIvol |
12 |
10 |
12 |
14 |
5 |
11 |
6 |
4 |
12 |
6 |
9 |
|
DLP |
443 |
400 |
610 |
480 |
161 |
410 |
203 |
175 |
388 |
221 |
298 |
|
Abdomen/pelvis |
|||||||||||
|
CTDIvol |
16 |
25 |
15 |
16 |
6 |
11 |
10 |
15 |
29 |
11 |
13 |
|
DLP |
781 |
800 |
745 |
760 |
280 |
644 |
575 |
637 |
1.07 |
571 |
656 |
Table 3 Comparison of Local DRLs from each hospital in this survey with other major surveys worldwide
|
Head |
|||||||
|
A |
B |
C |
D |
E |
F |
G |
|
|
Rotation Time |
1 |
0.75 |
1 |
1 |
1 |
1 |
0.75 |
|
Collimation |
2X2.5 |
16X0.75 |
128X0.6 |
128X0.5 |
64X0.5 |
128X0.5 |
16X0.75 |
|
KV |
130 |
120 |
120 |
120 |
120 |
120 |
120 |
|
Mean mAs |
147 |
200 |
180 |
300 |
250 |
157 |
192 |
|
Pitch |
1 |
0.9 |
0.5 |
0.813 |
0.828 |
0.5 |
0.5 |
|
Slice Thickness |
3 mm |
3 mm |
6 mm |
0.5 mm |
0.5 |
6 mm |
3 mm |
|
AEC (TCM) |
on |
on |
on |
on |
on |
on |
on |
|
Chest |
|||||||
|
A |
B |
C |
D |
E |
F |
G |
|
|
Rotation Time |
0.8 |
0.75 |
0.5 |
0.35 |
0.35 |
0.5 |
0.75 |
|
Collimation |
2X4.0 |
16X1.5 |
128X0.6 |
128X0.5 |
64X0.5 |
128X0.6 |
16X1.5 |
|
KV |
110 |
120 |
120 |
120 |
120 |
120 |
120 |
|
Mean mAs |
112 |
235 |
128 |
150 |
200 |
186 |
156 |
|
Pitch |
2 |
1 |
1.2 |
0.813 |
0.641 |
0.6 |
1.2 |
|
Slice Thickness |
5 mm |
5 mm |
6 mm |
0.5 mm |
0.5 mm |
6 mm |
5 mm |
|
AEC (TCM) |
on |
on |
on |
on |
on |
on |
on |
|
Abdomen/Pelvis |
|||||||
|
A |
B |
C |
D |
E |
F |
G |
|
|
Rotation Time |
0.8 |
0.75 |
0.6 |
0.75 |
0.75 |
0.6 |
0.75 |
|
Collimation |
2X5.0 |
16X1.5 |
128X0.6 |
128X0.5 |
64X0.5 |
128X0.6 |
16X1.5 |
|
KV |
110 |
120 |
120 |
120 |
120 |
120 |
120 |
|
Mean mAs |
160 |
187 |
170 |
180 |
350 |
176 |
176 |
|
Pitch |
2 |
1.2 |
0.6 |
0.813 |
0.828 |
0.6 |
1.2 |
|
Slice Thickness |
6 mm |
5 mm |
8 mm |
0.5 mm |
0.5 mm |
6.0 mm |
5 mm |
|
AEC (TCM) |
on |
on |
on |
on |
on |
on |
on |
Table 4 Scan parameters for CT departments of the sample hospitals
DRLs are an important tool for controlling the practices of radiology departments and, in particular, CT departments and contributing to the optimisation of radiation doses.3,19−22 The use of DRL has been shown to reduce the radiation doses in clinical practice, such as done in the UK, where the value of DRLs in 2005 for radiography and fluoroscopy was about 16% lower than the value of DRLs in 2000 and about half that seen in the mid-80s.20 The values of DRLs must reflect current practices, but also must take into account the evolution of technology.23 The study highlights the importance of dosimetry of CT scan departments at regular intervals, and stresses that the practical execution of the examinations should be based on the technology, the type of examination, the probable disease being investigated and the characteristics of the individual patient. The three examinations selected to be included in this study represent the most common tests performed in the daily clinical practice worldwire.5 The study confirmed the findings of previous studies suggesting that two slices CT scanners appear to provide the lowest dose to patients compared to single-slice and multi-slice CT scanners.22,24
The results have led to the finding that for the same type of examination, in order to answer the same clinical question, each CT scan department performs a protocol with different parameters. Depending on where each patient performed the exam, the dose he received could significantly exceed the mean. Certain variants in screening protocols may be indicated by the clinical question and the dimensions of the patient's body (e.g. obese patients). However, the differences in the dose indexes are large. The same conclusions have been reached by other studies from other countries.23 This is implying a need for optimization among hospitals. All hospitals studied were using the dose reduction methods and in particular Tube Current Modulation included in the systems, which have been shown to reduce the dose to as much as 40%.25,26 Not all CT scans had iterative reconstruction ability and those who had not used it for the routine protocols of these examinations.
The comparison of this study results with UK27 and EU,21 reveals that the levels of Local DRLs in sample hospitals are smaller except two cases. Hospital D for head exam that has a much higher value than all studies (LDRL CTDIvol = 102, LDRL DLP = 1641).16,17 Thereafter, Local DRLs for E hospital for the abdomen exam have a much higher value than it does in all other studies (LDRL CTDIvol = 29, LDRL DLP = 1070). Local DRLs based on this study for Chest exam seems to have lower values than other studies and National DRLs of Greece. The results showed a wide variety of CTDIvol and DLP values, which may be due not only to the specifications of CT systems but also to scan protocol settings and differences in examination practices. This study shows that there is room for optimization of the dose across these CT departments. Implementing systematic controls can help achieve this goal. This combined with greater awareness by health professionals, by the public, and commitment to the implementation of DRLs, can ensure that radiation doses are kept as low as reasonably achievable in all centers.
This study was based on data from only seven hospitals and only one city. Although Athens is the largest city in Greece and its capital, the individual study of DRLs from CT scans cannot produce results with a high degree of generalization, even if these hospitals receive a large volume of patients per year. Including more data would reinforce the study. The study also relied on the accuracy of the CTDIvol and DLP indexes as they are displayed on the console of each CT scanner. Although these indicators are regularly checked for accuracy by manufacturers, it does not always mean they are absolutely accurate. A study28 has reported that deviations of up to 20% may occur between the measurements displayed on each scanner, which may lead to inaccuracies in the final results. Ιmages was not examined and accepted as having the necessary quality because they led to a diagnosis and there was no need to repeat any of the exams.
None.
Author declares that there is no conflict of interest.

©2019 Dousi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.