International Journal of
eISSN: 2574-8084


Case Report Volume 2 Issue 2
Neurosurgical Department, Hassan II University, Morocco
Correspondence: Said Hilmani, Neurosurgical Department, Hassan II University, UHC Ibn Rochd, Morocco, Tel 212664440642
Received: October 09, 2016 | Published: February 27, 2017
Citation: Hilmani S, Maati A, Azhari A. Combined intracerebral and cranial epidural hydatid cysts: case report. Int J Radiol Radiat Ther. 2017;2(2):51-53. DOI: 10.15406/ijrrt.2017.02.00021
Background: Hydatid cyst (HC) is a parasitic disease caused by Echinococcus granulosus. Involvement of the central nervous system (CNS) is very rare in this parasitic infection and the association of intracerebral and epidural HC is exceptional.
Patient and method: A 6year-old female who was operated three years ago for a left frontal intracerebral hydatid cyst in Toto without rupture and without medical treatment following the surgery, and who came with the history of headache and vomiting for 4months is reported. Computed tomography of the brain showed a large 5x6x5cm, cystic lesion with a density similar to the cerebrospinal fluid in the left frontal region with another adjacent small cyst in epidural space. The patient underwent left frontal craniotomy. The patient was treated by Dowling technique for intracerebral cyst and by cyst aspiration after rupture.
Conclusion: Hydatid cysts in epidural location are very rare and can be primary or after recurrence. The mainstay of treatment is surgical removal of the cyst. Medical therapy is also important to prevent recurrences during the postoperative period.
Keywords: hydatid cyst, epidural, echinococcus, cranial cyst, intracerebral, postoperative, medical therapy, treatment, surgical, recurrence
Hydatid disease is a parasitic infestation caused by Echinococcus granulosus in Mediterranean countries and is endemic in some regions of the world.1 Hydatid disease has been reported with varying frequency in most body organs. The involvement of central nervous system was reported about 2-4%.2 Cerebral cysts are more common in the paediatric population with a male predominance.3 They are commonly located supratentorially in the watershed regions of the middle cerebral artery.4 Primary or secondary Epidural occurrence of hydatid cysts is very rare and exceptional where it associated with separate intracerebral localisation. Almost always a single lesion is seen, multiple or recurrent hydatid cysts in the brain are rarely reported.5 Here we report an exceptional case of a child diagnosed by two separate intracranial cerebral and epidural hydatid cysts.
An eight-year-old girl underwent surgery for the removal of an intracerebral frontal left hydatid cyst three years ago. She didn’t take any regular medical therapy following surgery. She came with intermittent headaches and vomiting for two months. There was no history of recent trauma. Physical examination revealed a healthy child in no distress. There was no frontal syndrome. Chest X rays and abdomen ultrasonography were normal. CT scan revealed a relatively large left frontal cystic lesion of similar density to cerebro-spinal fluid, with another small separate one in the epidural space in the adjacent region close to the midline, associated to bone exostosis around the cyst without bone defect (Figure 1). No rim enhancement was seen. Laboratory tests were normal. The patient underwent a left frontal craniotomy which revealed intracerebral and epidural hydatid cysts (Figure 2). The intracerebral cyst was completely removed following the Dowling’s technique, whereas the epidural one ruptured because It was seen that the inner part of the cranium overlying the cyst was thickened and the membrane of the cyst was adherent to the cranium. The contents of the cyst aspirated without any contagion and the cavities were irrigated with warm hypertonic saline solution. The epidural cyst membrane removed totally and dura underlying was normal. The dinner table was eroded by the mass without total defect. There was no evidence to suggest that both cysts communicate between each other. The postoperative course of the patient was uneventful. CT scan control showed a complete removal of the two cysts without recurrence (Figure 3). Following the surgery, the patient received oral Albendazole (15mg/kg/day). She is doing well at 6months follow-up.
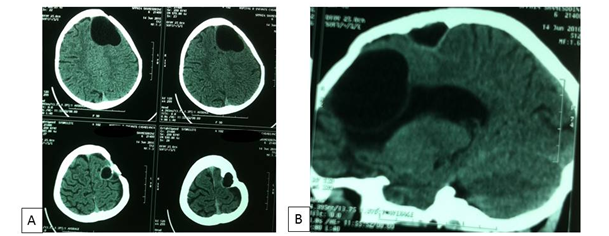
Figure 1 Axial CT scan contrast (A) showing a homogeneous, cystic, no enhanced left intracerebral frontal lesion with an adjacent small one in convex inner margin indicating extradural location, associated to exostosis. The sagittal view (B) shows the extent of the frontal hydatid cyst towards the frontal horn of the left lateral ventricle and a separate epidural cyst.
Echinococcosis Granulosus, the agent responsible for hydatid disease, causes the cyst formation in human.6 Brain (1-3%) is one of the rare involved organs by the haematogenous dissemination.7,8 However, only 2% of hydatid cysts are localized in the skeleton and of these 3 to 4% are found in the skull.1 Three forms of central nerve system hydatid disease occurring in intracranial were described: intracerebral, cranial extradural, and a combined form. In this third form, extradural HC may develop through dura defect as reported in our previous published case9 or with a normal dura. The mechanism may be an embolization of scolices or embryos via blood vessels in primary form with tendency to occur around the midline; may be due to the existence of a rich venous vascularization in this area,10 or secondary to previous cyst rupture. This is most likely in our case. The lesions may cause no symptoms until they become quite large.11,12 Most common symptoms are headache, vomiting, nausea, and focal neurological signs like weakness of extremities.12‒14 Most of the symptoms tend to disappear after successful removal.
Both cranial CT scan and MRI demonstrate the hydatid cysts adequately, revealing solitary, homogeneous, spherical and large parenchymal cysts with well-defined borders, without perifocal oedema or contrast enhancement.12,15 In bone window, CT can show some bone reactions around epidural cyst, like defect2 or exostosis as seen in this case.
To remove unruptured cerebral hydatid cysts, the Dowling technique16 is recommended and safe surgical procedure to avoid ruptures that could result in serious complications such as anaphylactic shock, meningitis or recurrences.14 This technique is also recommended for epidural cyst,4 but could not be performed effectively in our patient as reported by Behari S et al.,10 because the epidural hydatid cysts adhered to dura mater and osseous trabeculae. So bone location is easily ruptured during the surgical procedure.
Medical treatment with Albendazole both pre- and postoperatively was suggested in cases of recurrences, intra-operative cyst rupture, as well as when giant or multiple hydatid cysts are encountered.12 Long-term follow-up in patients with cerebral hydatid cyst disease having surgery without intra-operative cyst rupture has confirmed a very good outcome.17
Hydatid cysts in epidural location are very rare and can be primary or after recurrence. The mainstay of treatment is surgical removal of the cyst. Medical therapy is also important to prevent recurrences during the postoperative period. Epidural HC is extremely rare but it should be considered as differential diagnosis of cranial epidural cystic lesion in endemic countries.
None.
Author declares that there is no conflict of interest.

©2017 Hilmani, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.