International Journal of
eISSN: 2574-8084


Research Article Volume 4 Issue 6
Department of Radiology, University College London, UK
Correspondence: Muhammad Dharas, Department of Radiology, University College London, 28 Wyndham Road, Birmingham, UK, Tel 7874995780
Received: November 14, 2017 | Published: November 28, 2017
Citation: Dharas M, Santhirasekaram A. Access to inpatient computed tomography pulmonary angiography (CTPA). Int J Radiol Radiat Ther. 2017;4(6):451-454. DOI: 10.15406/ijrrt.2017.04.00114
Introduction : In-patient requests for CTPA should be performed and reported within one working day of receipt and acceptance of the request form, with a target of 90%.
Methods: 400 CTPA scans over a three-month period were retrospectively recorded. We noted: Date and time of the request, vetting, scan and report as well as the presence of a PE, Wells score and d-dimer result.
Results and discussion: Scans were reported within 24hours the request in 51.7% of cases. The target is only reached within 96hours of the request. The average time from request to report, request to vetting, vetting to scan and scan to report, was 35.3, 11.7, 19.39, and 1.66hours respectively. There was no significant difference for scans requested out ofhours between 17.00 and 09.00. A PE was diagnosed in 11.3% of cases. The average time from vetting to scan is the largest portion of the time from request to report. The British Thoracic Society (BTS) guidelines suggest a Wells score ≥ 4 does not require a d-dimer for which we were non-compliant in 56% of cases. It also states a CTPA should not be requested without a positive d-dimer if the Well’s score is <4 for which we were non-compliant in 6.3% of instances.
Conclusion:
Keywords: pulmonary, embolus, CTPA, ct, angiography, d-dimer, wells, score, embolism, PE
CTPA, computed tomography pulmonary angiography; PE, pulmonary embolism; RCR, royal college of radiologists; NICE, national institute for clinical excellence; NHS, national health servicE
The RCR advise that the timeframe between receipt and acceptance of an inpatient CTPA and issuing of the report should be one working day, with a recommended target rate of 90%.1 We sought to determine whether this target was achieved within Sandwell and West Birmingham NHS Trust, specifically within the City Hospital site. Our study focuses on the pathway between request and scan, to determine whether the entire process of handling CTPA requests can become more streamlined and thus improve patient care.
A PE occurs when a blood clot, usually a deep vein thrombus from the leg, travels within the bloodstream and lodges within part of the pulmonary arterial network. Although symptoms can be non-specific, a PE commonly results in acute shortness of breath and/or chest pain, but symptoms can also include tachycardia, tachypnoea, haemoptysis, a sense of apprehension and, more rarely, syncope which suggests a larger clot and a poorer prognosis.2
Due to the non-specific nature of the symptoms, diagnosing a PE is not always possible clinically. Clinical suspicion relies on history, examination, relevant blood tests including D-dimer where appropriate and when a PE is considered likely, further imaging should be considered to establish a definitive diagnosis. The chance of an abnormal clot forming and subsequently lodging in the pulmonary vasculature is more likely when the components of Virchow’s triad are present,3 namely; stasis of blood flow, endothelial injury and hypercoagulability. Hence malignancy, significant immobility, major surgery, recent fracture, pregnancy, blood disorders are among the common causes of abnormal clot formation.
It is for this reason that the Wells score - a clinical prediction rule - takes into account some of these factors in determining the likelihood of a PE which, together with clinical judgement, point toward or away from further investigations. A CTPA is the gold standard imaging modality in patients who have a clinically likely acute PE,4 or a suspected PE with an unlikely Wells score but a positive D-dimer, and according to NICE guidelines it should occur immediately.5 In the interim period while awaiting a scan, treatment with an appropriate anticoagulant should begin.
We initially analysed retrospective data from 400 in patients who were being investigated for possible PE. This was done using CRIS software, chronologically obtaining data from patients who underwent inpatient CTPA across a three month period. The data obtained was: the time of request of CTPA, the time of vetting, the time of scan and the time of report being issued which make up the four main milestones in the scan process, and the requirements outlined by the RCR.
To provide the data with more depth, we also ascertained whether the Wells score was provided as part of the scan request, and based on the Wells score, whether a D dimer was ordered. We obtained this data using CDA software from the hospital intranet. Finally, we read the report in order to prove whether a PE was diagnosed definitively and thus were able to provide an accurate measure of CTPA scans which are actually diagnostic of a PE; in other words, the accuracy of the suspected diagnosis.
To determine whether there was a difference in scans being processed during ordinary workinghours and out ofhours, we separated results obtained from within these timeframes. Workinghours were considered as scans taking place between thehours of 0900-1700, and out ofhours was classified as thehours of 1700-0900.
Following this, the data was subjected to statistical analysis. We initially sought to ascertain lengths of time taken during the reporting pathway, in order to determine timeframes which were promoting or hindering adherence to the RCR target. Additionally, we sought to analyse whether British Thoracic Society guidelines were adhered to especially when requesting a CTPA with a low clinical probability Wells score and associated negative D-dimer, and whether priority was placed on CTPA scans with high clinical probability. We also outlined the timeframe taken for all scans to complete the request to report process, and then separated this data according to Wells score. Finally we ascertained how many pulmonary emboli were actually diagnosed on CTPA, and therefore expressed this as a percentage of the amount of scans ordered.
From the data collected from 400 in patients undergoing CTPA, 51.7% and 68.5% of scans were reported within 24hours of the request and vetting respectively, which fell significantly short of the RCR recommended 90% target. The target was achieved within 72hours of vetting, at a rate of 92.5% while 91.3% of scans were reported with 96hours of the request. It took 192hours for 100% of the scans to complete the process from request to report (Figure 1 & Figure 2).
Average time from request to report, request to vetting, vetting to report, vetting to scan and scan to report, were 35.3hours, 11.7hours, 21.04hours, 19.39hours and 1.66hours respectively. For scans requested between 17.00 and 09.00, average time from request to report, request to vetting, vetting to report, vetting to scan and can to report, was 33.0hours, 14.1hours, 18.6hours, 17.3hours and 1.68hours respectively. Request to vetting, vetting to scan and scan to report times are indicated graphically, with working hours compared to out of hours (Figure 3). It demonstrates that the largest proportion of time is spent between vetting to scan (yellow), both during working hours and out of hours.
Collectively, a PE was diagnosed at a rate of 11.3%. We found a PE present in 15.5% of cases if the Wells score was greater than or equal to 4, and in 6.7% of cases if the Wells score was less than 4. Importantly, there were no cases of PE when the Wells score was less than 4 and D-dimer was negative. A Wells score was not submitted as part of the request in 4.0% of cases and a D-dimer was performed in 56% of cases where the Wells score was greater than or equal to 4; indicating high clinical suspicion of PE. In cases where the Wells score was less than 4, the D-dimer was negative 1.6% of the time. Furthermore, the D-dimer was not noted on the request form in 35% of requests and a D-dimer was not performed in 4.7% of requests.
The average number of hours from request to report if the Wells score is greater than or equal to 4 and less than 4 was 36.2hours and 34.1hours respectively (p<0.05) (Figure 4). This suggests that there is little discrimination in scanning patients who have a higher clinical probability compared to those with low-medium probability. Based on this, we have designed an easy to use algorithm which will highlight an order of priority when scanning patients with CTPA (Figure 5).
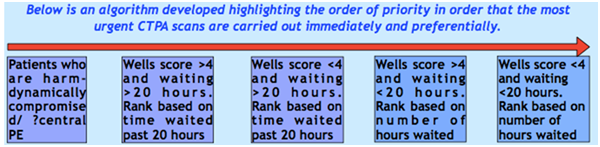
Figure 5 Algorithm highlighting order of priority when using CTPA to investigate patients with suspected PE.
The main outcome of the study was to design an algorithm or pathway which would better enable a Trust to comply with the recommended target outlined by the RCR; for 90% of scans to be reported within one working day of the request. Our Trust was non compliant by 38.3%, with the target only being achieved within 96hours of the request. As our results demonstrate, the main obstacle in achieving this target appears to be logistical in nature. Although reports are carried out relatively quickly after a scan is performed, obtaining a slot for the physical scan itself seems to take the longest time, and hinders compliance of the target. Furthermore, it seems that implementation of algorithms is suboptimal resulting in overuse of CPTA, often incorrectly.6
However, there also appears to be inconsistency in offering CTPA scans. As indicated, 6.3% of patients with a low probability Wells score and a negative or no D-dimer present still underwent CTPA. In low-medium clinical probability, a D-dimer should be performed because a negative result is helpful in excluding PE in these patients.7 Furthermore, when clinical probability is low, offering a D-dimer is part of the most cost-effective strategy in investigating PE.8 Generally, D-dimer sensitivity in low probability PE is high,9 while one study found sensitivity to be 100%.10
Taking this into account, the number of patients exposed to unnecessary radiation and investigation will reduce, as unquestionably, a high index of clinical suspicion coupled with a likely Wells score result - which pertains to a score of 4 or above, with or without a positive D dimer makes a PE much more likely to be diagnosed on CTPA. In these cases, performing a D-dimer is not recommended.11 However, despite guidelines, we carried out D-dimer tests on 56% of patients who did not require this i.e. had a high clinical probability. Furthermore, studies have shown that of those investigated for suspected PE, few are confirmed to have the condition. The yield varies from less than 5% to 30% based on risk stratification and clinical presentation.12 The diagnostic rate of PE in our study was 11.3% which fits within this range. One possible reason for this is not adhering to BTS guidelines as outlined above. It is safe, within an acceptable failure rate, not scan a patient with a low Wells score and negative D-dimer.13 Furthermore, a Wells score of 2 or less can be used alone to reasonably exclude a PE.14
Interestingly, a new clinical calculator, known as pulmonary embolism rule out criteria (PERC) has been piloted to determine its efficacy in replacing D-dimer testing. However, despite high negative predictive value, approximately 8% of confirmed PEs are missed in patients with a low Wells score.15
Simple diagnostic algorithms made readily available and displayed in departments such as A&E have been effective in improving pre-test PE clinical probability documentation, reduced unnecessary D-dimer requests and more importantly reduced the frequency of unnecessary CTPA scans.16 In the same way, we hope to implement our algorithm which will not only filter out unnecessary requests but also make prioritizing them a more systematic and streamlined process.
Furthermore, the study as a whole is intended to prove that when organising any radiological intervention, the patient should always be central to the decision. Clinical suspicion should point towards the diagnosis and the appropriate bedside and minimally invasive tests should be carried out in the first instance. This should minimise patients undergoing unnecessary tests which help preserve resources and minimizes exposure to radiation and adverse effects of contrast media.17 It is not possible for radiologists to act as gatekeepers to the department, so for the responsible team, acquainting themselves with adequate knowledge of a patient’s presentation and background will improve the proportion of appropriate imaging.18
The above algorithm should help to organize and prioritise CTPA requests. However, there is also a logistical requirement of improved efficiency within the department. We recommend that the following improvements will make CTPA requests more likely to impact patient care positively and also help to guide which requests to accept and which to reject, and should also lessen the burden on the department by directing scans in a more organised fashion:
Develop an electronic CTPA-request form which cannot be submitted unless all clinical information including well’s score and d-dimer are provided.
Dr. Khizer Rana (Consultant Radiologist, Sandwell and West Birmingham NHS Trust).
Author declares that there is no conflict of interest.
The written informed consent of the patient was obtained, for the publication of her case.

©2017 Dharas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.