International Journal of
eISSN: 2574-8084


Case Series Volume 8 Issue 2
Neurology department, Military Hospital Avicenne of Marrakech, Morocco
Correspondence: Prof Jawad Oumerzouk, Neurology department. Military Hospital Avicenne of Marrakech, Gueliz.Marrakech, Morocco, Tel 0614134817
Received: March 20, 2021 | Published: May 3, 2021
Citation: Oumerzouk J. A case series of posterior reversible encephalopathy syndrome. Int J Radiol Radiat Ther. 2021;8(2):61-63. DOI: 10.15406/ijrrt.2021.08.00295
Introduction: The posterior reversible encephalopathy (PRE) is a clinico-radiologic syndrom characterized by seizures, consciousness’s disorder, visual loss, and headache associated with cerebral posterior abnormalities on imaging. It raises often a problem of differential diagnosis with cerebral infarction.
Case reports: We report the case of five patients, the first followed for systemic lupus erythematosus, the second is hypertensive poorly follow-up, the 3 other patients were in postpartum after cesarean delivery. All our patients had generalized tonic-clonic seizures associated with an hypertensive peak without edema syndrome. Laboratory tests were unremarkable. The EEG showed epileptic abnormalities and brain MRI was in favor of a reversible posterior leukoencephalopathy. Evolution under treatment was favorable without recurrence with a decline of 20 months.
Conclusion: Rapid regression clinical and radiolologic abnormalities suggest cerebral vosogenic oedema as mechanism of this disease and confirm its mildness. Nevertheless, PRE may not be reversible without an early control of causes.
Keywords: reversible encephalopathy, high blood pressure, pregnancy, imaging, vasogenic oedema
Posterior reversible encephalopathy (EPR) is a recently described entity1 to designate a clinical-radiological picture that appears relatively stereotyped. Its symptomatology is dominated by headaches and seizures. Often it is a problem of differential diagnosis with cerebral infarction mainly venous. We herein present five case reports discussing the clinical and pathogenesis aspects of posterior reversible encephalopathy and the place of imagery in its management.
Case 1: Patient 30 years old, right-handed, followed for a systemic lupus erythematosus complicated by nephropathy, was admitted for generalized, preceded two hours earlier, by severe headache. Clinical examination noted a blood pressure to 200/130mmhg, a delirium, right hemiparesis and pyramidal syndrome. Computed tomography (CT) brain (Figure 1), showed multiple hypodense lesions, poorly systematized, parieto-occipital, bilateral, evoking venous ischemic stroke (AIC). A treatment with antihypertensive (intravenously calcium channel blocker), anticoagulants (heparin) and anti -epileptic drug (diazepam during the crisis, and then relay by sodium valproate) was started. The magnetic resonance imaging (MRI) brain performed 11 days later doesn’t objectify parenchymal lesion. At angiography MRI, vascular exploration showed a normal patency of the venous sinuses (Figure 2). The diagnosis of reversible encephalopathy was held before the clinical and radiological regression of symptoms, which justified the use of anti- platelet aggregation.

Figure 1 Cerebral CT, axial slice, with injection of contrast product (C +): bilateral posterior hypodensities poorly systematized.
Case 2: patient 44, right handed, hypertensive poorly followed, was hospitalized for occipital headaches associated with visual disturbances and dizziness. The examination in admission 19 hours later, found a blood pressure to 180/90, and a bilateral cortical blindness, without sensory-motor deficit nor coordination disorder or cranial nerves achieving. CT brain was in favor of bilateral arterial infarction in the occipital cortex with a small cortical hemorrhagic softening (Figure 3). MRI performed on the third day (Figure 4) confirmed the CT data, without revealing any abnormality on angiographic sequences or diffusion sequences. Laboratory tests, as well as cardiovascular explorations (transthoracic echocardiography and supra-aortic arteries Doppler) showed no abnormality. The patient received aspirin, dipyridamole and amlodipine at a daily dose of 5 mg. Control MRI 15 days later was normal (Figure 5). The evolution was marked by a complete regression of visual disturbances, with a current decline of 16 months.
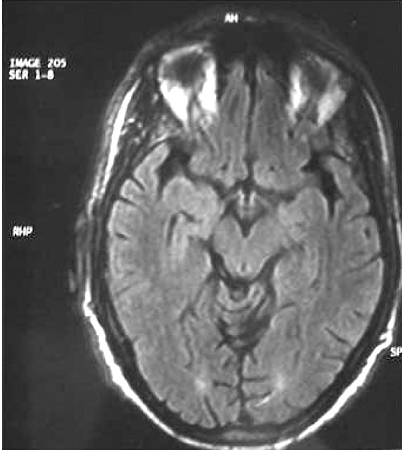
Figure 4 Brain MRI, axial slice, T2 FLAIR sequence and diffusion: poorly systematized bilateral posterior hypersignals.
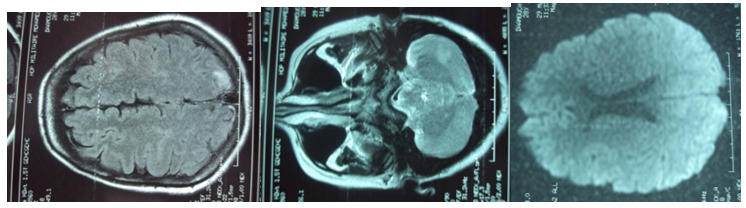
Figure 5 Brain MRI, axial slice, T2 FLAIR sequence and diffusion: occipital and cerebellar hypersignals poorly systematized.
Cases 3, 4, 5: 3 primiparous patients with pregnancy carefully monitored, and no medical history, presenting generalized tonic-clonic seizures in postpartum after cesarean delivery, preceded by or associated with an hypertensive peak, without headache edematous syndrome or fever.
Seizures stopped with 10mg of diazepam, and hypertension disappeared rapidly after a milligram of nicardipine intravenously injection.
The review after crisis resolution didn’t find sensorimotor deficit or lower limb edema. The fundus was normal and proteinuria was negative.
The CT angiography or angio MRI has objectified signs for posterior leukoencephalopathy.
The electroencephalogram (EEG) showed epileptic abnormalities.
An etiologic balance including a complete blood count, blood electrolytes, a calcium and phosphate, a magnesium, transaminases, a study of cerebrospinal fluid, an Immunological and inflammatory markers, thyroid hormones, viral and syphilitic serology was negative.
The patient was placed under sodium valproate at a dose of 20mg/kg and antiplatelet agent with almost complete disappearance of clinical and radiological signs evolution after a decline of 20 months.
Reversible posterior encephalopathy (EPR) or Posterior reversible encephalopathy syndrome (PRES), replaced various names, hypertensive encephalopathy, regressive posterior leukoencephalopathy or the occipito- parietal encephalopathy. It means a clinical and radiological syndrome, combining four cardinal symptoms to varying degrees: «headache, impaired consciousness, seizures and visual disturbances ranging from the alteration of the visual field to cortical blindness», with mainly parieto-occipital white matter abnormalities.2
Its occurrence is secondary to rupture of the blood-brain barrier (BBB) by sudden and paroxysmal blood pressure increase, or by toxic endothelial damage, leading to vasogenic edema.3 In the particular case of peri-partum, other mechanisms are superadded, including capillary hyperpermeability of pregnancy, high blood pressure, and the role of vascular tone modulating substances such as: hypersensitivity to endogenous vasopressors, lower vasodilator prostaglandins, and the cytotoxic factor of placental origin responsible for endothelial cell dysfunction.1
The majority of reported cases in obstetrics is linked to preeclampsia or eclampsia1,4-6 or with HELLP syndrome7 the absence of limb edema and proteinuria, and the normal liver function singles out our second observation.
Topographically, posterior achievement predominance is explained by the smaller development at this level of the sympathetic system which is the neurogenic response intended to compensate the myogenic response altered by endothelial injury. The result is a hyper perfusion which is combined with the alteration of the BBB and blood hypertension, leading to vasogenic edema.8,9
The EPR occurrence context of is generally specific and can suggest the diagnosis: hypertension, eclampsia or pre-eclampsia, renal failure, acute intermittent porphyria, treatment with immunosuppressive or anti-mitotic, such as cyclosporine or tacrolimus,... Brain imaging, including MRI is the key to the diagnosis. Indeed, it shows signal abnormalities in cortico- parietal-occipital cortex, hypo intense on T1, hyper intense on T2 and on FLAIR sequences, however, with normal diffusion sequences. The increase in the apparent diffusion coefficient (ADC), and the rapid regression of the lesions reflect the vasogenic edematous character of lesions and confirm the diagnosis.10,11
The prognosis of this disease is generally favorable with antihypertensive treatment or after toxic treatment discontinuation.2 However, cases of residual epilepsy have been described and correlated with delayed treatment.5 In peri-partum, the tendency of most authors is to extract the fetus early in view of the likely pathophysiological relationship of eclampsia and EPR.6
Posterior reversible encephalopathy is an unknown affection. Its pathophysiology is not yet fully elucidated. The magnetic resonance imaging is the cornerstone for the diagnosis, to differentiate this syndrome from other arterial and especially venous vascular affections, avoiding the patient an often heavy treatment.
None.
Author declares there are no conflicts of interest.

©2021 Oumerzouk. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.