International Journal of
eISSN: 2574-8084


Case Report Volume 3 Issue 2
1Department of Surgery, Kumamoto General Hospital, Japan
2Department of Gastroenterological Surgery, Kumamoto University, Japan
Correspondence: Shinya Shimada, Department of Surgery, Kumamoto General Hospital, Community Health Care Organization (JCHO), 10-10 Tohricho, Yatsushiro, Kumamoto 866-8660, Japan, Tel 81-96-532-7111, Fax 81-96-532-2772
Received: June 01, 2017 | Published: June 21, 2017
Citation: Morinaga T, Horino K, Shimada S, et al. A case in which a solitary fibrous tumor developed in the retroperitoneal cavity. Int J Radiol Radiat Ther. 2017;3(2):208-210. DOI: 10.15406/ijrrt.2017.03.00056
Solitary fibrous tumors (SFTs) were initially reported to be pleural tumors, but they can occur at any site. Herein, we report an unusual case in which a large SFTS developed in the retroperitoneal cavity. A 43-year-old female was referred to our hospital because of abdominal distension. Computed tomography (CT) and magnetic resonance imaging revealed a large retroperitoneal tumor occupying the entire abdominal cavity. In addition, CT showed that the right adrenal artery was the tumor’s main feeding artery. At first, we suspected an intra-abdominal tumor, but no conclusive evidence to support this diagnosis was obtained. As there was a possibility of malignancy (and to relieve the patient’s symptoms), we performed the surgical resection. A postoperative pathological examination revealed that the tumor was an SFTs derived from the retroperitoneal mesenchyme. The patient has been tumor-free for 5years since the operation. We present a rare case of SFTs that was difficult to differentiate from an adrenal tumor.
Keywords:intra-abdominal tumor, retroperitoneal mesenchyme, SFTs, solitary fibrous tumors
MRI, magnetic resonance imaging; CT, computed tomography
SFTSs was described in 1931.1 It was a pleural tumor. SFTs was subsequently referred to as solitary mesothelioma, benign fibrous mesothelioma, or localized fibrous tumor of the pleura because of its histological features and the fact that many cases involved the pleura.1‒3 Previously, it was considered that SFTs are derived from mesothelial or mesenchymal tissues, but recent ultrastructural and immunohistochemical studies have strongly indicated that SFTs originate from the mesenchyme.4,5 We now know that SFTs can occur at any site, and reports of extra-thoracic SFTs involving sites such as the mediastinum,6,7 pericardium,8,9 and retroperitoneum10 are becoming increasingly common. However, SFTs are difficult to diagnose due to their rarity. Here, we describe a case in which an SFTs arose in the retroperitoneal cavity and was hard to differentiate from an adrenal tumor.
A 43year-old female noticed a mass in her abdomen about 1 month before she was referred to our hospital. The area just above the mass was tender, and the mass extended from the right upper abdomen to the lateral abdomen and was the size of a child’s head. No other findings were noted during physical examinations. A laboratory analysis produced almost normal results, and computed tomography (CT) and magnetic resonance imaging (MRI) revealed a large retroperitoneal tumor measuring 20×16cm occupying the entire abdominal cavity. The tumor had pushed the surrounding organs, such as the right kidney and liver, outwards (Figure 1). The right adrenal artery was the tumor’s main feeding artery, but many other arteries surrounded and fed the tumor (Figure 2). The tumor’s interior had a non-uniform structure; some areas exhibited early enhancement, whereas other areas were barely enhanced. There were no signs of distant metastasis or infiltration into the surrounding tissues. From the above findings, we initially suspected an adrenal tumor, but no conclusive diagnostic evidence was obtained. A further laboratory analysis produced the following results: adrenaline, 10pg/mL; noradrenaline, 189pg/mL; dopamine, <5pg/mL; cortisol, 17.1µg/d; aldosterone, 398pg/mL; dehydroepiandrosterone sulfate, 56µg/dL; plasma renin activity, 4.7ng/mL/h; urinary vanillylmandelic acid, 4.2mg/day; urinary metanephrine, 0.09mg/day; urinary normetanephrine, 0.24mg/day. These findings suggested that the mass was a non-functioning tumor. In addition, no accumulation was seen in the adrenal region on metaiodobenzylguanidine scintigraphy. Finally, we performed a complete surgical resection of the tumor and the right adrenal gland because of the possibility of malignancy and to relieve the patient’s symptoms. Macroscopically, the surgical specimen was 20.0x20.0x18.0cm in size and weighed 1.8kg. The mass was surrounded by a fibrous capsule and had not infiltrated into the surrounding tissue. A cross-section of the tumor showed a yellowish fibrous lobulated solid mass and some cysts (Figure 3). A pathological examination revealed that the tumor was composed of spindle-shaped cells, which were arranged in the “patternless pattern” and exhibited varying degrees of cellularity and low mitotic activity [1-2 mitoses per 10 high-power field]. Immunohistochemical staining detected positivity for CD34 and vimentin. On the other hand, the tumor was negative for c-kit, desmin, smooth muscle antigen (SMA), and S-100, which confirmed the diagnosis of a retroperitoneal SFTs. Based on the surgical findings, we suspected that the tumor was of mesenchymal origin; i.e., that it was derived from the nearby right adrenal gland. The patient did not suffer any complications and was discharged. No further treatments were performed, and 5years have passed without recurrence since the operation.
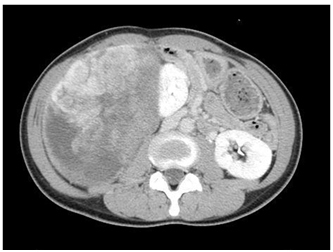
Figure 1 Macroscopic findings: Axial CT image of the abdomen at the mid abdomen level shows a large retroperitoneal tumor measuring 20×16cm was found. It occupied the entire abdominal cavity and had pushed the surrounding organs, such as the right kidney and liver, outwards.
The first SFTs was described in 1931.1 It was a pleural tumor. Incidence of SFTs was reported to be 2.8 cases per 100,000 registrations.2 SFTs most commonly occur in individuals in their 60s to 70s and do not exhibit any predilection for either gender. According to previous studies, approximately 30% of SFTs occur in the extra-thoracic region,1 but we now know that SFTs can occur any site. In agreement with this, the number of reported cases of extra-thoracic SFTs, including SFTs of the mediastinum,6,7 nasal cavity,11 liver,12,13 kidneys,14 pericardium,8,9 and retroperitoneum,10 is increasing. This report describes a case in which an SFTS arose in the retroperitoneum.
Previously, SFTs were considered to originate from the mesothelium,1‒3 and thus, were referred to solitary mesothelioma, benign fibrous mesothelioma, or localized fibrous tumors. However, recent ultrastructural and immunohistochemical studies strongly indicated that SFTs originate from the mesenchyme. The histological characteristics of SFTs include the so-called “patternless pattern”, which involves a haphazard, storiform arrangement of spindle cells, and a “hemangiopericytoma-like appearance” with prominent vascularity. Both patterns were evident in our case. In addition, immunohistochemical staining of SFTs results in positivity for CD34, Bcl2, and vimentin and negativity for c-kit, desmin, SMA, and S-100. In our case, CD34 and vimentin staining were positive. On the other hand, c-kit, desmin, SMA, and S-100 staining were negative. These results confirmed the diagnosis of SFTs.
Some cases of extra-thoracic SFTs are found after the detection of hypoglycemia, which is attributed to insulin-like growth factor produced by the tumor (incidence: about 5%).15 However, many extra-thoracic SFTs are encountered during the course of examinations for other disorders, such as stomach ache or dysuria, or during medical check-ups.16 Some cases of SFTs in retroperitoneum were found by palpable swelling in abdomen, but a certain case was found by dysuria because ureter runs to bladder in retroperitoneal cavity.17 In our case, palpable swelling in abdomen was a trigger to find her SFTs. SFTs have almost no specific symptoms, and thoracic SFTS might have been found first because they are easy to detect on X-ray examinations, whereas extra-thoracic SFTS are difficult to detect until they progress to some extent. It is hard to diagnose SFTs preoperatively because they do not exhibit any specific findings. So, clinicians should be aware that SFTs could occur at any site. The basic treatment for SFTs is resection with sufficient clear margins. Although most SFTs usually have a good prognosis, they have the potential to recur or metastasize after surgery, and so careful follow-up is required after complete resection.
In summary, we experienced a rare case in which SFTs developed in the retroperitoneal cavity, which was hard to differentiate from an adrenal tumor. We performed complete surgical resection, and 5years have passed without recurrence since the operation.
None.
Author declares that there is no conflict of interest.

©2017 Morinaga, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.