International Journal of
eISSN: 2577-8269


Research Article Volume 2 Issue 2
Council of Cardiovascular Epidemiology and Prevention of the Argentine Society of Cardiology
Correspondence: Walter Masson, Council of Cardiovascular Epidemiology and Prevention of the Argentine Society of Cardiology, Argentina, Tel 1136083629
Received: February 16, 2018 | Published: March 2, 2018
Citation: Masson W, Huerín M, Lobo M, et al. The new guidelines of high blood pressure substantially increase prevalence of hypertension in Argentina. Int J Fam Commun Med. 2018;2(2):76-79. DOI: 10.15406/ijfcm.2018.02.00040
Introduction: The 2017 ACC/AHA guideline recommends the use of lower pressure values to define hypertension.
Aim and methods: A multicenter, descriptive, cross-sectional study was performed. The objectives were: 1) to determine what proportion of non-hypertensive patients according to the previous recommendations in primary prevention were diagnosed as hypertensive by the 2017 ACC/AHA guideline; 2) to establish how many patients should receive pharmacological treatment; 3) To determine reasons to justify the indication of antihypertensive therapy.
Results: A total of 600 patients (mean age 50.3±11.3 years, 43.0% men) were included. According to the new guideline, 47.5% of the patients were classified as hypertensive (men 56.6% vs. women 40.6%). Within this group, 29.5% were candidates to receive antihypertensive drugs (men 40.4% vs. women 19.4%).
Conclusion: Applying the new guide in a non-hypertensive population according to the previous recommendations, led to diagnose approximately 50% more hypertensive patients and indicate antihypertensive therapy in a third of them.
Keywords: Hypertension, guidelines, antihypertensive therapy.
ACC, american college of cardiology; AHA, american heart association; DBP, diastolic blood pressure; SBP, systolic blood pressure; HDL-C, high-density lipoproteins; LDL-C, to low-density lipoproteins.
Hypertension occupies the first place for global disease burden and all-cause mortality.1 Moreover, the evidence favoring antihypertensive drug therapy to reduce cardiovascular events and mortality is conclusive.2 In Argentina, the Third National Risk Factor Survey determined that 34.1% of the population received the diagnosis of high blood pressure.3 By the end of 2017, the American College of Cardiology (ACC) and the American Heart Association (AHA) published the new guideline for the detection, prevention, management and treatment of high blood pressure.4 This guideline is an update of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC7). Compared with the JNC7 guideline, the 2017 ACC/AHA guideline recommends the use of lower systolic blood pressure (SBP) and diastolic blood pressure (DBP) values to define hypertension. On the other hand, these new recommendations suggest taking into account the cardiovascular risk estimated with the new score for cardiovascular disease used by the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to determine which patients with stage 1 hypertension should receive antihypertensive drugs.5 As a consequence, the number of patients diagnosed with hypertension would increase considerably and many patients should be treated with antihypertensive drugs. The objectives of this study were: 1) to determine what proportion of non-hypertensive patients according to the previous recommendations in primary prevention were diagnosed as hypertensive by the 2017 ACC/AHA guideline; 2) to establish how many patients should receive pharmacological treatment after applying the new recommendations; 3) To determine reasons to justify the indication of antihypertensive therapy.
A multicenter, descriptive, cross-sectional study was performed on consecutive patients aged 20 to 79 years attending cardiovascular prevention outpatient clinics in Buenos Aires, Argentina. Subjects attend these centers for a cardiovascular risk screening or for the management of risk factors. Exclusion criteria were: 1) previous cardiovascular disease; 2) history of hypertension according to previous high blood pressure recommendations (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg; 3) prior antihypertensive therapy. In this study, all subjects underwent a clinical examination. Blood pressure was recorded using a homologated automatic oscillometric blood pressure recorder after at least 5 min of rest on a chair and arm supported at heart level. Weight and height were registered and expressed as body mass index (weight in kilograms divided by the square of the height in meters). The blood levels of glucose, total cholesterol, cholesterol bound to high-density lipoproteins (HDL-C), cholesterol bound to low-density lipoproteins (LDL-C), triglycerides, HbA1c and creatinine were measured according to standardized biochemical tests. According to the new guideline of hypertension, blood pressure should be categorized as normal (<120/<80 mm Hg), elevated (120-129/<80 mm Hg), stage 1 hypertension (130-139 or 80-89 mm Hg) or stage 2 hypertension (≥140 or ≥90 mm Hg). Patients with stage 2 hypertension are not show because systolic blood pressure more than 140 mmHg and diastolic blood pressure more than 90 mmHg were exclusion criteria. The new score for cardiovascular disease used by the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol was calculated. Subjects with SBP between 130 and 139 mmHg or DBP between 80 and 89 mmHg plus a score ≥10%, ≥65 years of age or diabetes, were considered candidates for antihypertensive medication according to the 2017 ACC/AHA guideline. Statistical Analysis: Continuous variables were expressed as mean±standard deviation, and categorical variables as percentages. The analysis of categorical data was performed using the chi-square test. A two-tailed p value < 0.05 was considered as statistically significant. STATA 13 and 3.1 EPIDAT software packages were used for statistical analysis. The study was conducted following the recommendations in medical research suggested by the Declaration of Helsinki, Guidelines for Good Clinical Practice and valid ethical regulations. The protocol was reviewed and approved by the Investigation Area of the Argentine Society of Cardiology.
A total of 600 patients (mean age 50.3±11.3 years, 43.0% men) were included in the study. Twenty two percent of patients were active smokers and 9.5% had history of diabetes mellitus. The characteristics of the total population and according to sex are described in Table 1. When applying the new guideline, the patients were classified as “normal blood pressure” or “elevated blood pressure” in the 28.3% and 24.2% of cases respectively. Also, 47.5% of the patients were classified as stage 1 hypertension. This finding was significantly greater in men compared to women (Figure 1). The proportion of subjects diagnosed with hypertension was not different in the age groups analyzed (<40 years: 50.5%, 40-64 years: 46.8%, >65 years: 48.3%, p=0.13). Furthermore, there were no significant differences in the proportion of subjects diagnosed with hypertension when comparing the populations with and without diabetes (52.6% vs. 46.9%, p=0.70). When analyzing patients with stage 1 hypertension, 29.5% were candidates to receive antihypertensive drugs. This proportion was significantly higher in men compared to women (Figure 2). All patients older than 65 years and diabetic subjects with stage 1 hypertension were indicated to receive antihypertensive drugs according to the new guideline. However, the indication of antihypertensive therapy based on the risk score increased with age when evaluating non-diabetic patients between 40 and 65 years old (Figure 3). The main factor that determined the indication of antihypertensive treatment was the cardiovascular risk score ≥10%, both in the total population and in men. However, in women, the main factor was age ≥65 years (Figure 4).
|
Total population |
Men |
Women |
Continuous variables, mean (SD) |
|
|
|
Age, years |
50.3 (11.3) |
45.8 (12.0) |
53.8 (9.5) |
Systolic blood pressure, mmHg |
122.4 (10.6) |
124.5 (9.4) |
120.9 (11.2) |
Diastolic blood pressure, mmHg |
79.0 (6.8) |
79.1 (6.8) |
78.9 (6.8) |
Body mass index, kg/m2 |
27.0 (4.8) |
28.1 (4.1) |
26.3 (4.9) |
Total cholesterol, mg/dL |
220.6 (43.3) |
218.9 (46.2) |
221.9 (41.0) |
HDL-C, mg/dL |
49.5 (14.4) |
41.3 (10.0) |
55.7 (14.1) |
LDL-C, mg/dL |
141.6 (41.3) |
142.5 (45.0) |
140.9 (38.3) |
Triglycerides, mg/dL |
148.3 (92.8) |
177.2 (111.8) |
126.4 (67.8) |
HbA1c, % (patients with diabetes) |
7.1 (1.3) |
7.1 (1.2) |
6.9 (1.4) |
Categorical variables, % |
|
|
|
Diabetes mellitus |
9.5 |
10.9 |
8.5 |
Smoking |
22.0 |
23.7 |
21.1 |
Overweight |
37.6 |
46.4 |
31.2 |
Obesity |
24.4 |
28.6 |
21.4 |
Table 1 Characteristics of the population
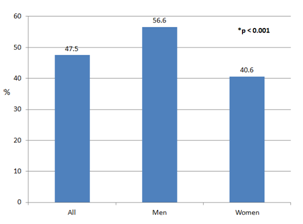
Figure 1 New patients diagnosed with hypertension according to new guideline.
*Difference between men and women.
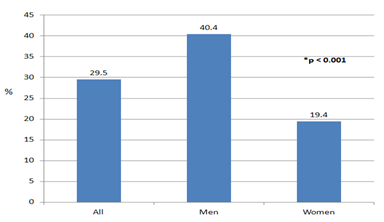
Figure 2 Stage 1 hypertension: Indication of pharmacological therapy.
*Difference between men and women.
In qualitative terms, the current analysis suggests a substantial increase in the prevalence of hypertension using the 2017 ACC/ AHA guideline. However, the percentage of patients recommended for antihypertensive medication increased modestly. A major driver for the changes introduced in the 2017 ACA/AHA guideline was SPRINT (Systolic Blood Pressure Intervention Trial) study.6 This trial randomized patients with SBP greater than 130 mm Hg to intensive blood pressure control of SBP to less than 120mmHg vs. less than 140 mm Hg. The intensive control intervention resulted in a statistically significant reduction in the composite cardiovascular primary endpoint over a median follow-up of 3.26 years as well as a statistically significant reduction in overall mortality, leading to the early trial termination. However, this study presents some considerations that limit the generalization of its results.7 On one hand, the blood-pressure measurement method used in SPRINT (in the office without an observer with automatic device) differs from previous clinical trials and the real clinical practice. On the other hand, some previous observational studies and clinical trials suggest that more intensive blood pressure control doesn’t provide evident cardiovascular and mortality benefits compared with standard control.8,9 In our study, approximately half of the patients received the diagnosis of “new hypertension”. This finding was greater in men compared to women. Similarly, Muntner et al. showed that compared with the JNC7 guideline, the 2017 ACC/ AHA guideline results in a substantial increase in the prevalence of hypertension in US adults, with a higher prevalence in men.10
Another interesting point is that the new guideline defines 4 groups of patients who benefit from pharmacological treatment, even with blood pressure values previously considered as "prehypertension" (stage 1 hypertension): History of cardiovascular disease, diabetes, age ≥65 years and subject with a score ≥10%. In our study, about 20% of women and 40% of men would have an indication for antihypertensive therapy according to the 2017 ACC/ AHA guideline. However, the main reason that determined the indication of antihypertensive drugs differed between men and women. In women, the main reason was age (≥65 years), whereas in men it was the score ≥10%. On the other hand, older age was associated with a greater probability of receiving pharmacological treatment in the group of patients between 40 and 65 years old. The explanation for this finding is the significant role played by age in the calculation of the risk score. The choosing of the ACC/AHA pooled cohort equations to estimate cardiovascular risk creates additional difficulties. The risk estimator has also been criticized for lacking proper calibration and for over estimating risk, particularly in young individuals.11 The radical modifications suggested by the 2017 ACC/AHA guideline of hypertension, recalls the controversy of the latest recommendation for the management of cholesterol. Recent investigations from the United States and Argentina showed that compared to the previous recommendations, the application of the 2013 ACC/AHA guideline for the management of cholesterol increased considerably the number of new statin prescriptions.12,13 Both in the scenario of hypercholesterolemia or hypertension, this may lead to more low-risk patients to receive aggressive drug treatment with questionable benefit-to-harm ratios. When a new guideline that modifies diagnosis and treatment thresholds arises, it’s always essential that this new strategy is not associated with an increase in risk, as could be seen in previous studies of arterial hypertension that found a J curve effect, by which more strictly controlled hypertensive patients, could evolve worse. Regardless of the guideline we choose, the current management of high blood pressure is a major public health problem. Despite the high prevalence and damage caused by hypertension, the most important problem, at least in our country, is the lack of diagnosis, while in treated hypertensive patients, the main problem is the scarce degree of its control.14 In conclusion, when applying the 2017 ACC/ AHA guideline in a non-hypertensive population according to the previous recommendations, the diagnosis of hypertension increased by approximately 50%, while a third of the subjects with this diagnosis would be candidates to receive antihypertensive therapy.
None.
The authors declare that they have not conflict of interest.

©2018 Masson, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.