International Journal of
eISSN: 2577-8269


Case Report Volume 6 Issue 1
1Retina and vitreous Asociación para Evitar la Ceguera en México IAP, Mexico
2Ophthalmology Asociación para Evitar la Ceguera en México IAP, Mexico
Correspondence: Alejandro Sánchez-Hoil, Asociación para Evitar la Ceguera en México IAP, Postal Adress: Vicente García Torres 46, San Lucas, Coyoacán, Mexico City. Mexico, CP: 04030, Tel (+52) 999 163 08 30
Received: January 17, 2022 | Published: January 31, 2022
Citation: Sánchez-Hoil A, García-Uribe PA, Lara M, et al. Repair of penetrating ocular trauma with anterior and posterior pole involvement. Int J Fam Commun Med. 2022;6(1):26-28. DOI: 10.15406/ijfcm.2022.06.00258
Context: Ocular trauma is the leading cause of monocular visual impairment around the world, especially in developing countries like Mexico. Great part of this cases occurs in pediatric and young adult groups. Epidemiology can vary depending on the population studied, but different factors such as socioeconomic status, occupation, sport and other activities have a great influence. Approximately 30% to 40% of ocular blindness cases in the world is due to ocular trauma, and of these, between 80 and 90% of events are preventable.1,2
Objective: The aim of this paper is to expose the importance of an individualized and damage-oriented repair plan in the scenario of a penetrating ocular trauma and serve as a treatment guideline in similar cases.
Method: A case report of a 15 year-old male with right eye open globe injury with metal cable tip causing a penetrating corneal injury, posterior capsule rupture, lens opacity and vitreous hemorrhage
Conclusion: The present case report illustrates the diverse ways of presentation that can be found when managing a penetrating ocular trauma. Our patient history is a good example of extended ocular involvement including cornea, lens, vitreous and retina. Individualized and damaged oriented surgical treatment is key in ocular trauma scenarios.
Keywords: ocular trauma, open globe injury
Open globe injuries are generally considered to be serious events due to potential permanent loss of vision of one or both eyes, and even partial or complete loss of the eye globe. These events are a very frequent reason for urgency both in primary care centers as well as specialized ones. In most cases, they are trivial traumas that only affect the superficial structures of the eye; on other occasions, they can cause extremely serious sequelae, being an important cause of unilateral blindness in the world.3 Ocular trauma is the leading cause of monocular visual impairment around the world, especially in developing countries like Mexico. Great part of this cases occurs in pediatric and young adult groups. Epidemiology can vary depending on the population studied, but different factors such as socioeconomic status, occupation, sport and other activities have a great influence. Approximately 30% to 40% of ocular blindness cases in the world is due to ocular trauma, and of these, between 80 and 90% of events are preventable.1,2 A penetrating trauma is considered a unique complete thickness wound, that in most of the cases is caused by a sharp object, without a way of exit. This lesion may or may not be associated with involvement of posterior structures such as the retina or even have the intraocular retention of a foreign body.4
Considering all the variations and diverse ways of presentation its important that all ways penetrating ocular trauma or adjacent structures are submitted to a complete ophthalmologic examination to rule out a serious eye injury.5 These traumas are much more frequent in men than in women, and usually present in early and middle adulthood, although children are not without risk. The anterior segment is injured in an isolated manner in more than half of the cases, with isolated lesions of the posterior pole being rare.6
Surgical management by an ophthalmologist should begin as soon as the patient can safely undergo surgery. Initial surgical treatment includes microsurgical repair of corneal and/or scleral wounds with interrupted sutures. With adequate sealing of the anterior and posterior chamber. If there is a perforating injury involving posterior pole, additional surgery may be necessary. In case of crystalline compromise, its extraction is indicated with placement of an intraocular lens in a bag, or if not possible, in a groove or sutured. Indications for a vitrectomy include signs of developing retinal detachment, the presence of moderate to severe vitreous hemorrhage, phacoanaphylactic uveitis, intraocular foreign body and damage to other tissues requiring repair.7,8
Corneal repair intervention with or without cataract extraction and vitrectomy may preserve anatomic function of traumatized eyes and prevent loss of vision. However, there is currently no infallible or ideal management guideline for all causes and most of them must be individualized for the scenario of each patient.9,10 Here we present the case of a young man who suffered penetrating ocular trauma and was managed by means of corneal wound closure, lensectomy and vitrectomy via pars plana with an adequate postoperative anatomic and visual result.
We present a case of a 15-year-old Mexican male admitted to the retina department of “Asciación para Evitar la Ceguera en México” hospital at Mexico City with the chief complaint of decreased vision and trauma to his right eye on July 16, 2021. Patient had no important family health background and medical history was unremarkable. While working, he suffered a direct hit with a metal cable tip causing a penetrating corneal injury. The patient removed the foreign body second after and seek for medical attention.
Initial ophthalmic examination revealed diminished visual acuity to hand movement (LogMar 1.00), an intraocular pressure of 12mmHg, ciliary injection, corneal haze and edema with a full thickness periferic traumatic injury at 9 o´clock which was sealed with fibrinoid tissue, a retroqueratic blood cloth at 3 o´clock associated to a Descemet´s membrane rupture, a formed anterior chamber with profuse cellularity (4+), an irregular pupillary border and posterior synechiae at 9 o´clock with underlying involvement of the anterior capsule and lens opacity. Posterior structures were not visible due to media opacity and vitreous hemorrhage Figure 1 (A). He was classified with an ocular trauma score group 2 (56 points). Left eye examination had no pathologic findings.
A diagnostic B-scan ultrasound was performed on the right eye and intraocular lens calculation was obtained through left eye measurements. The aforementioned study reported a right eye axial length of 23.9mm, posterior lens capsule rupture, vitreous hemorrhage and a retinal tear at 9 o´clock Figure 1 (B). An anterior segment optical coherence tomography (OCT) was also performed in order to show the Descemet´s membrane rupture Figure 1 (C).
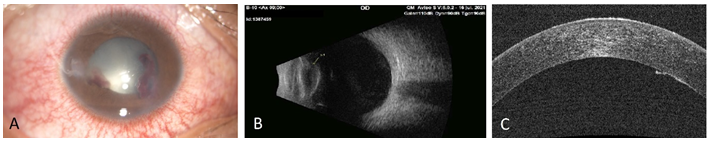
Figure 1 A - Anterior segment, clinical findings. B - B-scan ultrasound showing posterior lens capsule rupture (arrow). C - Anterior segment OCT showing Descemet´s membrane rupture.
Patient was admitted to the operating room. Next, we will mention the maneuvers carried out. Corneal defect was closed with 10-0 nylon simple interrupted sutures and blood clots were removed with anterior chamber washout. Trypan blue was placed for anterior capsule staining followed by continuous anterior capsulorhexis starting at the temporal tear. Afterwards, three 23 Ga vitrectomy trocar were placed at 3.5 mm from the limbus continued by infusion set and pars plana lensectomy with preservation of the anterior capsule remanent. Vitrectomy was performed with a complete posterior vitreous detachment, as well as photocoagulation surrounding retinal tear at 9 o´clock and a 3-piece IOL insertion in sulcus using the anterior capsule remanent previously mentioned. Finally, air-fluid exchange, sclerotomy closure and air bubble tamponade for Descemet´s membrane rupture was performed. Patient's evolution and recovery was favorable.
Six-month follow-up examination of the right eye showed a visual acuity of 20/20 (LogMar 0.00), a nearly intact transparent cornea with just a peripheral opacity at 9 o´clock and diffuse pigment retroqueratic deposits, a formed anterior chamber with no cells, and a 3-piece IOL in sulcus with a retrolental fibrotic ring Figure 2 (A). Fundus examination with a 9 o´clock extreme periphery retinal tear fully surrounded by laser Figure 2 (B). No additional findings were found. Left eye examination continued to be reported as normal. Control anterior segment OCT showed complete resolution of the Descemet´s membrane rupture Figure 2 (C).
The present case report is intended to illustrate the diverse ways of presentation that can be found when managing a penetrating ocular trauma. Our patient history is a good example of extended ocular involvement including cornea, lens, vitreous and retina.1
This case also shows the importance of a complete and exhaustive ophthalmologic examination, completed with the proper auxiliary tests, to identify all of the compromised structures and therefore design an optimal and individualized surgical plan.2 In this case specifically the use of a 3 piece IOL was decided for a final adequate dioptric power, as well as microincision scissors, forceps, and vitrectomy consumables, which were key for the optimal for the optimal realization of the repair.
Previous literature reports on certain affections such as preoperative posterior lens capsule rupture allows the surgeon to have a good starting point for including technique variations as showed in this report with the use of a continuous anterior capsulorhexis followed by a pars plana lensectomy, instead of an anterior phacoemulsification, to avoid the lens luxation to the vitreous cavity and therefore maintaining an adequate support for an IOL placement.
Regarding prognosis, this case is a good example of final outcome impact of a willful and complete presurgical plan based on previously available information and ophthalmologic examination completed with extension tests
According to the Ocular Trauma Score (OTS), the end visual result expected for this patient according to group 2 classification was: 28% of no light perception, 17% of light perception to hand movement, 18% of 1/200-19/200, 13% of 20/200-20/50 and 15% of 20/40 or better. Our case showed a final visual acuity of 20/20, which could be considered a surgical success considering initial probability.3
None.
The author declares there is no conflict of interest.

©2022 Sánchez-Hoil, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.