International Journal of
eISSN: 2577-8269


Case Report Volume 5 Issue 5
1Assistant Professor, National Institute of Laboratory Medicine & Referral Center (NILMRC), Dhaka, Bangladesh
1Assistant Professor, National Institute of Laboratory Medicine & Referral Center (NILMRC), Dhaka, Bangladesh
Correspondence: Sunzida Arina, Assistant Professor, National Institute of Laboratory Medicine & Referral Center (NILMRC), Dhaka, Bangladesh
Received: July 24, 2021 | Published: October 7, 2021
Citation: Arina S. Pulmonary histoplasmosis: A case report. Int J Fam Commun Med. 2021;5(5):148-150. DOI: 10.15406/ijfcm.2021.05.00237
Histoplasmosis is a systemic fungal infection caused by dimorphic fungus Histoplasma capsulatum. It is widely distributed throughout the world. In present study, the case of a 50-year-old male patient diagnosed as pulmonary histoplasmosis. Initially, the patient was suspected as a case of alcoholic hepatitis but subsequently the diagnosis of pulmonary histoplasmosis was confirmed by lung biopsy. The symptoms were dissuaded following amphotericin B and itraconazole treatment.
Keywords: histoplasma capsulatum, histoplasmosis, pulmonary, antifungal
Primary pulmonary histoplasmosis is a lung disease caused by the dimorphic fungus Histoplasma capsulatum. The disease may be self-limiting or asymptomatic in healthy individuals. The severity of this disease depends upon the number of inhaled fungal particles and the immune status of the host.1 Once this was considered a rare and fatal disease, but now it can be diagnosed. By modern diagnostic techniques this can be readily recognizable. The indiscriminate use of broad-spectrum antibiotics and the increasing use of steroids could possibly have altered the balance of normal host inhabitants and prepared the ground for infection by the mycoses.2 Among immunocompromised individuals the morbidity and mortality rates of this mycosis are greater. Clinical presentations may include fever, cough, chest pain and weight loss. These are non-specific symptoms that may also occur in other diseases. The majority of affected individuals present clinically silent manifestations and display no apparent symptoms. Therefore, misdiagnosis of pulmonary histoplasmosis as other pulmonary diseases, including tuberculosis, is very conceivable. Misdiagnosis may delay the treatment, and the disease is fatal if left untreated.3
The present study is diagnosed as a case of pulmonary histoplasmosis. It is necessary to find out the disease characteristics in order to facilitate the diagnosis and treatment of pulmonary histoplasmosis.
A 50year-old male patient came to a medicine specialist in 15th January 2021 with a persistent chest pain and cough. Then he referred to a respiratory medicine specialist in 23rd January 2021. On physical examination he has been found crepitation in lungs, hepatomegaly, clubbing, loss of testicular sensation. The patient had a history of smoking for 30 years and alcohol intake. Sometimes he had low grade fever. No signs of sweating, hemoptysis or other discomfort were noted. X ray chest reveals consolidation involving right upper and mid zones (Figure 1). Pulmonary CT guided FNAC detected a huge soft tissue lesion in the right upper lung. FNAC smear shows adequate cellular containing mostly necrosis and granular debris. Extracellular small bodies are seen. Morphologically these were suspicious for Histoplasmosis. No malignant cell was found. (Figure 2) On physical examination following were found: Body temperature, 37°C; heart rate, 76 beats/min; blood pressure, 120/80 mmHg. In addition, no superficial lymphadenopathy was noted and bilateral symmetry was observed in thoracic cage. Laboratory examination was also performed and revealed the following results: White blood cell count, 12,160/cumm (normal range, 4000-11000/cumm); red blood cell count, 4.85 m/ul (normal range, 4.5-6.5 m/ul); hemoglobin level, 15.3 gm/dl (normal range, 13-17 gm/dl); blood platelet count, 4,29,000/cumm (normal range, 1,50,000-4,00,000/cumm); an elevated erythrocyte sedimentation rate, 85 mm/1st hr (normal range, 0-10 mm/1st hr). Tuberculin test was negative. Quantiferon TB gold plus test was also negative. No acid-fast bacilli were found in acid-fast staining. In combination with clinical data, the patient was preliminarily diagnosed as bronchogenic carcinoma. This diagnosis was made on the basis that CT of chest showed a large mass with irregular margin in right lung. Sputum for fungus test revealed fungal elements having structural compatibility with Histoplasma capsulatum (Figure 3). So, the diagnosis of Histoplasma capsulatum was advantageous for the patient and open a new era of investigation in diagnosis of disease.
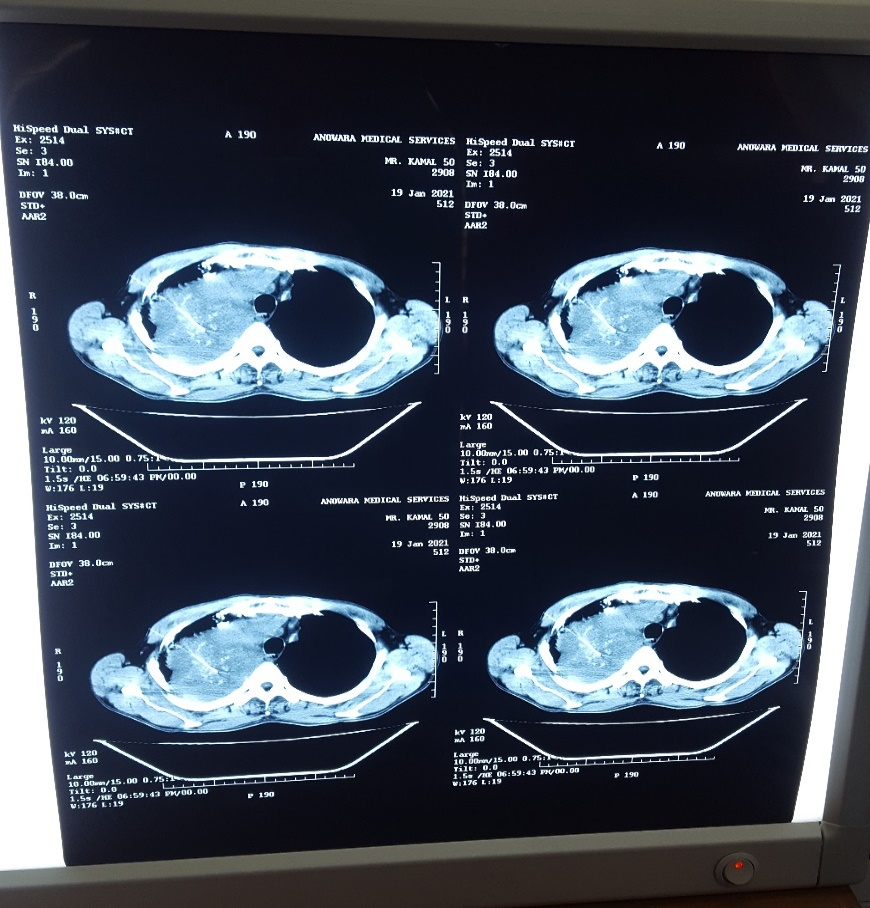
Figure 2 CT guided FNAC: Smear shows adequate cellular material containing mostly necrosis and granular debris. Extracellular small bodies are seen. Morphologically these are suspicious for Histoplasmosis. No malignant cell is seen.

Figure 3 Microscopic examination shows fungal elements having structural compatibility with Histoplasma capsulatum.
As the patient had history of alcohol intake and chronic back pain with above physical findings he was diagnosed as alcoholic hepatitis or chronic liver disease by a medicine specialist. The patient was treated with Moxifloxacin for 7 days, Paracetamol for pain, Esomiprazole and Domperidon for 1 month. As physical condition was not improving, he was referred to respiratory medicine specialist. With previous findings the patient was advised for FNAC, Z-N staining and the patient was prescribed with Montelucust and Doxophyline for continuous intake, Pregabalin for 10 days, Methyl prednisolone for 10 days, Dexlansoprazole for 1 month, Paracetamol with Tramadol hydrochloride for pain. Based on the findings of CT guided FNAC and microscopic findings, the patient was suspected with histoplasmosis. Following diagnosis, the patient was admitted to hospital and was treated with Amphotericin B and Itraconazole. The condition of the patient was improved after treated with antifungal drugs.
Histoplasma capsulatum is a fungal pathogen that can cause diseases in healthy people when taken at infecting doses. It is endemic in Middle America, South America, Africa, Australia, East Asia, India, Malaysia, and particularly in North America.4
Histoplasmosis was first reported by Darling in 1906, but subsequently remained practically un-recognized. Bunnell and Furcolow (1948) and Johnson and Batson (1948) described the chronic pulmonary form of histoplasmosis. Following this the number of cases has been increasing in most countries in the world.5
The first histoplasmosis survey was done in Bangladesh in 1961 (then East Pakistan), which revealed that 12–23% of people had a positive skin reaction to histoplasmin.6 The first case of histoplasmosis was reported1982 in Bangladesh7 and the second case in 2005.8 But nowadays cases are increasing.
Pulmonary histoplasmosis is a primary lung disease caused by infection with Histoplasma capsulatum. Histoplasma capsulatum is a dimorphic fungus, an intracellular organism, which parasitizes the reticuloendothelial system in histoplasmosis involving the spleen, liver, kidney, Central nervous system and other organs.9 The organism exists as a saprophyte in nature and found in soil, caves and abandoned constructions that are enriched in bat or bird excrement. Infection with Histoplasma capsulatum occurs by the inhalation of microconidia or mycelial fragments, which then settle in the host's lungs and convert to yeast forms. The invasion of this fungus is intimately associated with the host immunity. In immunocompetent patients, macrophages, epithelial cells and lymphocytes can eliminate the fungus.10
In developing countries like Bangladesh, tuberculosis is the commonest cause of granuloma formation and resembles clinical presentation which can be confused with the histopathology of granuloma formation of fungal infection.11 As histoplasmosis is an uncommon diagnosis in Bangladesh, diagnosis and management strategies should be work -up by the physician.
In this case as the patient had a history of alcohol intake for 30 years and had hepatomegaly, primarily he was diagnosed as a case of alcoholic hepatitis and treated as per symptoms. But improvement was not satisfactory. He was also suspected as a case of pulmonary tuberculosis and carcinoma also. But finally pulmonary histoplasmosis was diagnosed and patient was treated with antifungal drugs. After accurate discovery of disease, the patient improved.
Although it is thought to be an endemic disease, histoplasmosis is actually worldwide.12 It is essential for the physician to investigate the patient’s health status considering the opportunistic infection. Awareness should be increased to development and expansion of mycological diagnostic facilities. In present study of pulmonary histoplasmosis initially was misdiagnosed and later successfully treated with antifungal therapy. CT-guided lung needle aspiration biopsy should be performed in suspicious cases based on medical history and imaging to facilitate the differential diagnosis of pulmonary infection. Proper therapeutic management and prolonged follow up are essential to avoid recurrence of fungal infection.
None.
The author declares there is no conflict of interest.

©2021 Arina. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.