International Journal of
eISSN: 2577-8269


Research Article Volume 6 Issue 2
1University Anhanguera – Osasco, São Paulo, Brazil
2State University of Campinas – Campinas, São Paulo, Brazil
Correspondence: Carolina Loureço Reis Quedas, University Anhanguera – Osasco, São Paulo, Brazil
Received: April 12, 2022 | Published: April 29, 2022
Citation: Quedas CLR, Honda RTQ, Costa CCS, et al. Prevalence of motor tests in autism spectrum disorder people. Int J Fam Commun Med. 2022;6(2):87-92. DOI: 10.15406/ijfcm.2022.06.00270
In autism spectrum disorder, studies have in social communication, in their interest, education and social/educational inclusion with children and adolescents with aspects studied for this even larger audience is very scarce, observing a gap in the literature regarding this population. This work aims through a bibliographic survey to describe the tests that are being used in autism, as their advantages and objectives, are shown as evidence of study among them. The research was carried out in the Bireme and Pubmed databases with the descriptors “assessing motor autism”, “assessing motor skill performance and autism” and “assessing the development of physical fitness and autism”. the search resulted in 846 studies, after excluding duplicates, 823 articles remained. After reading the titles and abstracts, 703 studies were excluded and after applying the inclusion and exclusion criteria, 16 articles were included in this review. have similarities with each other, such as some ages and some tests such as: delineating the trail, basting a cord that is manual dexterity, grabbing and dribbling a ball and very similar tests such as walking under a line, jumping on one foot only in displacement, among others. We conclude that the tests available in the market are expensive for professionals and that each one evaluates more a specific skill for gaps in the estimates.
Keywords: autism, motors skills, deficient, motor assessments
Autism Spectrum Disorder (ASD) is defined as a disturbance in the development of the central nervous system, characterized by persistent deficits in social communication and the presence of restricted and repetitive patterns of behavior and interests. The typical characteristics of the disorder are observed in the different life contexts of the child with ASD, which may translate into different support needs and functional levels.1
The prevalence of autism today in the United States, according to the CDC (Centers for Disease Control and Prevention) is 1 in every 54 children aged 8 years. The increase is 10% compared to the previous number in 2014, which was 1 in 59 children. The statistic, released every two years by the CDC, continues to show the ratio of four boys to every girl and refers to 8-year-olds in the United States, in 11 states. These prevalence estimates are based on educational and health records collected by the CDC's Autism and Developmental Disabilities Monitoring Network.2
Studies are interested in social communication, in its neurological processing, and the social/educational inclusion of children and adolescents with ASD.3–7 However, the study of motor aspects for this population is still scarce, observing a gap in the literature regarding this population, alluding to the characterization of these aspects and the most appropriate forms of skill assessment, such as global coordination, manual functions ( including functional handedness), hand preference, and balance.
In this sense, it is already known that impaired motor capacity is a possible sign for the early diagnosis of ASD and could be included as a diagnostic criterion alongside difficulty with social communication and restrictive and repetitive behaviors.8 The child develops awareness of the world around him and of himself through motor exploration from the first days of his birth. Through motor control, the child experience activities that will serve as a basis for the construction of basic notions for their intellectual development.9
The research by Licari et al.10 states that motor delays are present in the phenotype of individuals with ASD. In their research, they found 2,084 children with autism aged ≤6 years, in which, more than a third met the criteria for motor difficulties, a rate almost as common as intellectual disability. This study demonstrates that motor difficulties are a prominent feature of the autism phenotype, requiring further consideration.10
In another study, the authors applied the DCDQ questionnaire to 16,705 parents of children with ASD and compared the DCDQ total scores and subscales from the SPARK dataset with published norms for each age between 5 and 15 years. The proportion of children with ASD at risk of motor impairment was very high, 86.9%. Children with ASD did not overcome their motor impairments and continued to be at risk for DCD even into adolescence. Still, only 31.6% of the children were receiving physical therapy services in both the diagnostic criteria and the autism assessment.11
In this way, understanding that there is still something to be explored in the motor assessment of children with ASD, the objective of this study is to present the tests that are being used in people with autism, their advantages, and disadvantages, and what are the tests of skills that are being used. resemble each other.
To meet the proposed objective, a systematic literature review was carried out in the Birem and Pubmed databases, based on the guidelines of the statement of preferred report items for systematic reviews and meta-analysis.12 For the searches, the descriptors "assessing motor development and autism", "assessing motor skill performance and autism" and "assessing physical fitness and autism" were used. words present in specific categories. This systematic search was carried out from February 20 to March 19, 2021.
The inclusion criteria established were: I) only texts that presented an application of quantitative motor assessment with individuals with ASD; II) studies from 2015 onwards; III) articles that were available online. The exclusion criteria used were: I) works that did not present any assessment instrument referring to motor function.
After performing the searches for the descriptors, the collected articles were organized and the duplicates were excluded. After excluding duplicates, studies were selected based on reading titles and abstracts. Those selected were read in full and the inclusion and exclusion criteria were applied. Finally, a qualitative analysis was carried out to achieve the main objective.
In total, the search resulted in 846 studies, after excluding duplicates, 823 articles remained. After reading the titles and abstracts, 703 studies were excluded and after applying the inclusion and exclusion criteria, 16 articles were included in this review. The search flowchart is illustrated in Figure 1. The objectives, methods, and conclusions of the articles included in this review are presented in Table 1.
Author |
Title |
Purpose |
Method |
Test/Instrument |
Skills |
Lourenço17 |
The Efficacy of a Training Program on Trampolines in Motor Proficiency of Children with Autism Spectrum Disorder |
Evaluate the effect of a trampoline training program on the motor proficiency and body mass index (BMI) of children with ASD. |
17 children with ASD aged between 4 and 10 years old .6 children on trampolines training - experimental group (EG), and the remaining 11 in the control group (CG). |
Bruininks – Oseretsky Test for motor proficiency |
fine manual control, manual coordination, body coordination, strength, and agility |
Alsaedi22 |
An Assessment of the Motor Performance Skills of Children with Autism Spectrum Disorder in the Gulf Region |
Aims to determine the prevalence, severity, and nature of the motor abnormalities seen in children with autism spectrum disorder (ASD) as well as to elucidate the associated developmental profiles. |
Assess various aspects of the motor performance of 119 children with ASD and 30 typically developing children (age range: 6–12 years) from three Gulf states. |
Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2) |
fine manual control, manual coordination, body coordination, strength and agility |
Choi et al.23 |
The development of fine motor skills is associated with expressive language outcomes in infants at high and low risk for autism spectrum disorder |
Investigate developmental trajectories of fine motor skills between 6 and 24 months in relation to expressive language outcomes at 36 months in infants at high and low familial risk for autism spectrum disorder (ASD). |
Participants included 71 high-risk infants without ASD diagnoses, 30 high-risk infants later diagnosed with ASD, and 69 low-risk infants without ASD diagnoses. |
At first the Mullen Scales of Early Learning (MSEL). |
Fine Motor |
Bricout et al.16 |
Motor Capacities in Boys with High Functioning Autism: Which Evaluations to Choose? |
Provide an overall profile of motor capacities in children with ASD compared to neurotypically developed children through specific tests, and to identify which motor tests best discriminate children with or without ASD. |
Twenty-two male children with ASD and twenty completed an evaluation with 42 motor tests |
Movement Assessment Battery for Children (M-ABC). |
MABC - manual dexterity, play and catch, balance |
Chu et al.19 |
The role of physical activity and body-related perceptions in motor skill competence of adolescents with autism spectrum disorder |
Assess the associations of motor skill competence with physical activity and physical self-perception of adolescents with autism spectrum disorder (ASD). |
Cross-sectional study. 63 male adolescents, aged 12–18 years, |
Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2) |
fine manual control, manual coordination, body coordination, strength, and agility |
Kaur et al.20 |
Creative Yoga Intervention Improves Motor and Imitation Skills of Children with Autism Spectrum Disorder |
Compare the effectiveness of an 8-week physical therapist- delivered yoga intervention or academic intervention in children with ASD |
Twenty-four children with ASD between 5 and 13 years of age participated in the study, with 12 children each in the yoga and academic groups |
Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2) |
fine manual control, manual coordination, body coordination, strength and agility |
Bremer et al.24 |
The Interrelationship Between Motor Coordination and Adaptive Behavior in Children with Autism Spectrum Disorder |
Explore the relationships between motor coordination and adaptive behavior in 7–12-year-old children with ASD. |
A sample of n = 26, from Ontario, Canada, |
(MABC-2) (VABS-2) |
MABC - manual dexterity, play and catch, balance |
Dadgar et al.21 |
The Relationship between Motor Imitation, and Early Social Communication Skills in Children with Autism |
Investigate the association of motor skills and imitation ability with early social communication skills in children with ASD |
In this study, 20 children with ASD aged 3 to 5 years |
TGMD-2 |
locomotion and ball skills |
Jeoung25 |
Motor proficiency differences among students with intellectual disabilities, autism, and developmental disability |
Determine whether students with such disabilities have differences in their motor proficiency. |
Was compared the motor proficiency of 82 students (age, 11 to 20 years) with different severities of intellectual disability developmental disability, or autism |
Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2) |
fine manual control, manual coordination, body coordination, strength and agility |
Manicolo et al.15 |
Gait in children with infantile/atypical autism: Age-dependent decrease in gait variability and associations with motor skills |
Investigate Gait and its associations with pre walking motor milestones, motor skills, and age. |
A study group pf 32 children aged between 4.1 and 16.9 year. |
MABC-2 |
MABC - manual dexterity, play and catch, balance |
Kaur et al.18 |
Comparing motor performance, praxis, coordination, and interpersonal synchrony between children with and without Autism Spectrum Disorder |
Compare gross and fine motor, praxis/imitation, motor coordination, and interpersonal synchrony skills |
across three groups of |
Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2) |
fine manual control, manual coordination, body coordination, strength and agility |
Le Menn-Tripi et al.26 |
Sensory-psychomotor evaluation in Autism: A new tool for functional diagnosis |
the construction and validation of a new scale, designed to evaluate sensory-psychomotor signs in Autism: ‘the Sensory-psychomotor Particularities Scale in Autism’ (SPSA). |
The population of this study includes 111 children aged 25 to 155 months. The diagnosis was made according to the clinical criteria of the ICD-10 |
MABC -2 |
MABC - manual dexterity, play and catch, balance |
Ament et al.27 |
Evidence for Specificity of Motor Impairments in Catching and Balance in Children with Autism |
Compare motor functioning among three groups: children with ASD, children with ADHD, and TD children in order to better define motor deficits in these clinical groups and understand whether motor deficits assist in distinguishing between clinical groups. |
A total of 200 children, ages 8–13 years, participated: 56 children with ASD. |
MABC-2 |
MABC - manual dexterity, play and catch, balance |
Holloway et al.28 |
Relationships between gross motor skills and social function in young boys with autism spectrum disorder |
Examine the relationship between gross motor skills and social function in young boys with autism spectrum disorder |
Twenty-one children with ASD participated in the study. |
Peabody Developmental Motor Scales Second Edition (PDMS-2) |
PDMS-2 : reflexes, locomotion, body control, object manipulation, grasping, visual-motor perception |
Liu et al.13 |
Nutrition, BMI and Motor Competence in Children with Autism Spectrum Disorder |
Examine the relationship between motor competence, body mass index (BMI), and nutrition knowledge in children with autism spectrum disorder (ASD). |
Fifty-one children with ASD (five females and 46 males) aged 7–12 participated in the study. |
MABC-2 |
MABC - manual dexterity, play and catch, balance |
Sarabzadeh et al.14 |
The effect of six weeks of Tai Chi Chuan training on the motor skills of children with Autism Spectrum Disorder |
Aims to investigate the effectiveness of basic Tai Chi Chuan forms to improve motor function problems in children with ASD. |
18 children with ASD in the age range between 6e12 years old were divided randomly into experimental and control groups. |
M-ABC |
MABC - manual dexterity, play and catch, balance |
Table 1 Description of articles
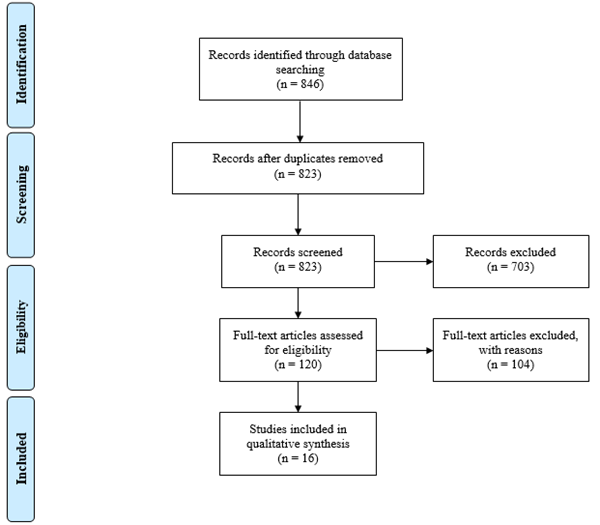
Figure 1 PRISMA flow diagram.
Font: The authors, based on http://www.prisma-statement.org/PRISMAStatement/FlowDiagram
The MABC-2 is a test consisting of eight tasks that involve manual dexterity skills, throwing/receiving skills, and skills related to static and dynamic balance. The test is divided into 3 (three) sections per age group with 8 tasks between sections: Section 1: 3 to 6 years; Section 2: 7 to 10 years; Section 3: 11 to 16 years.
The tests of this test stand out in 8 tasks divided into manual dexterity that are 3 tasks of fine motor coordination, precision, and agility, skills with the ball with 2 tasks that involve skills such as manual eye coordination, reaction time, sense of space, precision, balance, and global motor coordination and balance with 3 tasks that include static and dynamic balance.
The articles by Amente et.al (2015), Liu et al.13 Sarabzadeh et al.14 Le Menntripi et. al (2019), Manicolo et al.15 and Bricout et al.16 use Mabc2 to assess possible delays in the motor development of children and adolescents with ASD.
The Bruininks-Oseretsky Test of Motor Proficiency–2nd Edition (BOT-2) was used in 6 studies by the authors Lourenço et al.17 Kaur et al.18 Chu et al.19 Bogjia et. Al (2019), Kaur et al.20 and Asaedi (2020).
This test has two versions, the short and the extended. The short form has 12 specific groups: fine motor coordination: fine motor precision (painting a star and outlining the trail), fine motor integration (copying the circles and copying a diamond), and manual dexterity (basting a string in blocks).
Global Motor Coordination: bilateral coordination (touching the nose with the tip of the index finger, keeping the eyes closed, and rotating the thumbs and index fingers). Balance (walking with one foot in front of the other under a line). Agility and Speed (jump with one foot for 15 sec). Coordination of the upper limbs (catching and throwing the ball with one hand and dribbling the ball alternating hands) and strength (push-ups with the knees extended or supported on the floor). It assesses children aged 4 to adults aged up to 21 years and 11 months.
The TGMD 2 test was used in the article by Dadgar et al.21 is a test that covers the age of children from 3 years to 10 years and 11 months, it assesses the individual's global motor coordination through two subcategories: Locomotion (6 skills) and Object control (6 skills).
Skills are running, galloping, one-footed jumping, long jump, standing jump, and moving laterally over a line. Object control skills consist of hitting a stationary ball (baseball, dribbling the ball stationary, receiving a ball with the hands, kicking a ball, throwing a ball at the wall over the shoulders, and throwing a ball from below. The result of this the test is very specific as it shows the child's motor age in its subcategories as well as the differences between them.
PDMS-2 includes five subtests distributed over two motor components/scales: global and fine motor skills. Its results are expressed in three domains of motor behavior: the fine motor quotient (QMF), the global motor quotient (QMG), and the total motor quotient (QMT), the latter resulting from the first two.
The QMF is found by the sum of two sets of subtests, namely, fine grip and visuomotor integration, while for the QMG three are used: postural control, locomotion, and manipulation of objects (the latter is replaced by the reflex subtest for children up to eleven months old). Each of these subtests consists of items (motor tasks) adjusted for age and placed in an increasing sequence of difficulties. The child starts the test on a given item, according to his age, and continues in the sequence until he fails to perform three consecutive ones.
After analyzing all the skills and evidence of the tests, we can conclude that the global skills involving objects are present in all tests, for example: throwing a ball, bouncing the ball, catching the ball with the hands. Skills that involve locomotion are also present, such as: walking under a line (which also involves balance) and running. The balance skills are present in the tests in the one-foot displacement, jumping with one foot in displacement, and standing on a beam.
Regarding fine motor coordination, the TGMD-3 test does not present any test aimed at this ability, the others (MABC-2. BOT-2 and PDMS-2) present different tests, but two tests stand out for their similarity, such as: delineating a trail, copying a circle and snap the string to a ruler or blocks.
None.
The Authors declares that there is no conflict of interest.

©2022 Quedas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.