International Journal of
eISSN: 2577-8269


Case Report Volume 2 Issue 5
1Medical Ultrasonographer, Medical Tower CIMA Hermosillo, Sonora, Mexico
2Obstetrician-Gynecologist, San Benito Clinic, Hermosillo, Sonora, Mexico
3Resident Medical Imaging, General Hospital of the State of Sonora Dr. Ernesto Ramos Bours, Hermosillo, Sonora, Mexico
Correspondence: Antill¢n-Valenzuela J, Medical Ultrasonographer, Medical Tower CIMA Hermosillo, Sonora, Mexico
Received: September 08, 2018 | Published: September 20, 2018
Citation: Antillón-Valenzuela J, Barajas-Valenzuela M, Castañeda-Palafox CD. Ovarian ectópico pregnancy case report. Int J Fam Commun Med. 2018;2(5):297-299. DOI: 10.15406/ijfcm.2018.02.00097
It is defined as the anomalous implantation of the fertilized ovule at the level of the ovarian parenchyma, which occurs in 0.5-3% of cases of ectopic pregnancy. This pathology is observed each more frequently, given its association with a history of PID, endometriosis, use of IUDs or other assisted reproduction techniques; It also has a mortality of up to 10%. Its clinical picture is usually variable and similar to other locations of ectopic pregnancy, which is why imaging studies play a fundamental role for its accurate diagnosis. Although multiple diagnostic criteria have been proposed, there is still little experience in this regard and very often it is usually confused with a tubal location pregnancy in previous imaging studies and confirmed its ovarian location at the time of surgery. We present the case of a 30-year-old woman, with a primitive diagnosis of ectopic pregnancy, and her sonographic follow-up is described until the precise diagnosis of right ectopic ovarian pregnancy, proposing the use of the sign of "block mobility" to sonographic compression as a guideline fundamental.
Keywords: ectopic ovarian pregnancy, ectopic gestation, sign of ‘block mobility’, surgery, old woman, metrorrhagia, uterine cavity, abdominal, family planning, ovarian pregnancy, hemodynamic instability, age, married, sonographic, leucorrhoea, ectopic ovarian
Ectopic pregnancy refers to the implantation of the fertilized ovum outside the uterine cavity, that is, in an abnormal site and occurs in 1-2% of all pregnancies. Within the sites of ectopic implantation, the tubal region is the most frequent site (95%), followed by abdominal (1.3%), ovarian (0.5-3%) and cervical (0.1%) implantation.1–5 Ovarian gestation is a rare form of ectopic implantation with a high mortality rate, reaching up to 10% and whose diagnosis is becoming more frequent given the technological advance in imaging tests. This type of ectopic pregnancy is more frequent in young and multiparous patients, especially in those with risk factors, among which the use of IUD as a method of family planning, use of assisted reproduction techniques, antecedents of endometriosis, pelvic inflammatory diseases stand out. (EPI) or previous pelvic surgeries.1–3 A study conducted at the University Hospital of La Paz, Spain in 2012 by Cristina Gonzalez et al. it mentions the presence of only 6 cases throughout 2001-2011, of which 85% were diagnosed during the first trimester and where it is difficult to diagnose given the little experience in the subject of that time;1 also mentions that the majority of cases were carried out during the surgical procedure.1–3 On the other hand, Huang et al. They carried out a study in Changsha, China in 2011 in which they mention that they only had one case of ectopic pregnancy with ovarian location.6 Another similar study also conducted in Madrid, Spain in 2013 and carried out by Pato et al.5 mentions that the diagnosis of ectopic ovarian pregnancy was made in up to 75% of the cases during the first trimester but does not refer to the total number of cases or how the diagnostic check of its location was made.5 The clinical picture of an ovarian pregnancy is very broad and variable, ranging from an asymptomatic pregnancy of uncertain location, to abdominal pain, amenorrhea with or without metrorrhagia or hemoperitoneum with or without associated hemodynamic instability.1–7 Surgery is currently considered a gold standard in terms of treatment, however, other therapeutic alternatives have been proposed, such as local use or systemic from methotrexate.1–7 further from this, in case from instability or Necrosis requires the completion of oophorectomy, which occurs in approximately 21% of cases. For diagnostic confirmation of ovarian gestation, it is necessary to carry out histopathological study which should show trophoblastic and placental tissue in the ovarian tissue; as well as normal uterine salpinges.1–10
Female patient of 30 years of age, married, menarche at 10 years of age, 30x4 rhythm, with a history of dysmenorrhea, G1, P0, A0, C0. She went to a gynecologist-obstetrician for pregnancy control (7.5 SDG), referring to occasional colic and brown transvaginal waste without other aggregates. Within the analyzes of laboratory is found with Hb 12.5g / dl, leukocytes 8,000 uI, glucose 96mg / dL, β-HCG 2551mUI / mL, as well as general urinalysis (EGO) without alterations. On examination, transvaginal touch was performed, finding whitish leucorrhoea not fetid, so pelvic ultrasound (transabdominal) was requested, and qualitative control of β-HCG, and it was mentioned two days later. In this ultrasound uterus is reported without evidence of gestational sac (Figure 1) and second quantification of β-HCG of 2688mUI/mL. It is mentioned for the third time two days after showing ascending β-HCG quantification (2708mIU/mL), so it was decided to perform a new sonographic study by transvaginal route, confirming the presence of an empty uterine cavity (Figure 2); In addition, right ovary is observed with two nodules adjacent and inseparable from it; one of them with a hypoechoic aspect of 3 cm in diameter and the other of ecogenic appearance of 2.8 cm in diameter (Figure 3); later they are explored with Doppler mode, observing peripheral vascularity in the first (ring of fire sign) and scarce internal vascularity in the second considering itself what may correspond with body lute Y coat gestational disorganized respectively. Finally, indirect compression maneuvers are performed through the transducer, drawing attention to the "block" mobility of the right ovary with these nodules, which is why the probability of ectopic ovarian pregnancy is highly considered (Figure 4). It is sent with a treating doctor who decides to perform surgery (Figure 5); tissue samples are sent to study pathological he which reports "Findings compatible with pregnancy ectopic ovarian " (Figure 6).
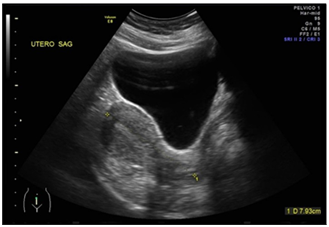
Figure 1 Study desonografia with suprapubic abodaje in which uterus is observed in retroflexion of usual shape and size as well as empty uterine cavity.
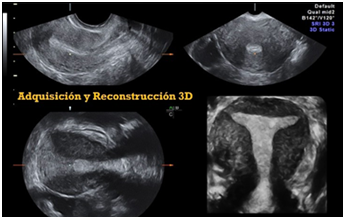
Figure 2 Endo vaginal sonographic study with 3d reconstruction corroborates the finding of empty uterine cavity.
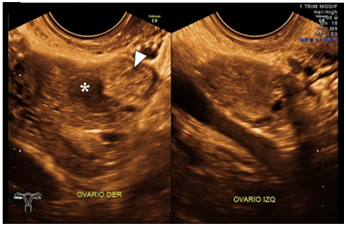
Figure 3 Study of and ovarian sonography in which the right ovary is observed; as well as suggestive image of the luteous body (fleche tip) and adjacent echogenic nodule (*) from origin to determinal. Left ovum without apparent alterations.
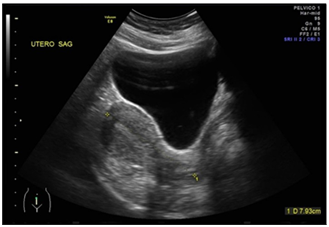
Figure 4 Right ovary visualized via endovaginal where ovarian parenchyma with conserved vascularity is observed; ovidea and hypo echoic image suggestive of the luteum with peripheral vascularity (in ring). Finally, an adjacent echogenic nodule with internal vascularity is observed, with a low resistance resisence (not visualized in the image).
The diagnosis of ectopic ovarian pregnancy is not simple, that is why currently no specific sonographic criteria are established for its diagnosis. Among the main proposed criteria are the empty uterine cavity, present in 100% of the cases, as well as an inseparable echogenic image of the ovary (more echogenic than the corpus luteum and with a continuous vascular pattern) present in 15%.1–7 Other criteria still under study are the presence of vascualrity with resistance index (UR) <0.39 inside the pseudomasa, this finding has high specificity and positive predictive value (PPV) but is only observed in 15% of cases,3–8 besides that this characteristic is also observed in masses corresponding to the corpus luteum.9 Other findings have been described, such as the double hyperechogenic halo and the presence of a gestational sac with an embryo and heartbeat present only in 4% and 7% of cases, respectively.1 All these findings were observed in the case presented; in addition to them, the codependence that exists between the ovarian parenchyma and the adjacent pseudomasa is striking when performing compression maneuvers with the intracavitary transducer, this finding corresponds to "movement in block" of the same, which leads to its origin is ovarian. On the other hand, this finding is not observed when the ectopic pregnancy has tubal or abdominal origin in which there is movement independent of them. That is why we propose the sign of "block movement" as a useful sonographic finding to make the diagnosis of ectopic pregnancy ovarian The maneuver described above coincides with the findings reported by Chukus et al. in 2015 where he mentions this "block movement" and where he also highlights the importance of accurately identifying the corpus luteum, which must be differentiated from the pseudomasa corresponding to the ectopic pregnancy that in most cases has a thick ring and of greater echogenicity than the same body lute.9
The approach of a pregnancy of uncertain location always results in a diagnostic challenge; the sonographic findings observed in this case applied in another context could correspond to the presence of a corpus luteum; However, due to the clinical data and history of our patient (β-HCG levels, absence of visible intrauterine gestational sac and transvaginal bleeding), the possibility of ectopic pregnancy had to be considered in the first instance, and by simple sonographic maneuvers such as the presence / absence of "Blocking of the ovary and pseudomasa" could be demonstrated in spite of its low prevalence (less than 1% of ectopic pregnancies).
None.
The author declares there is no conflict of interest.

©2018 Antillón-Valenzuela, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.