International Journal of
eISSN: 2577-8269


Case Report Volume 7 Issue 5
Department of pediatric surgery, National University Center, Hubert Koutoukou Maga, Cotonou Benin
Correspondence: Gogan Mahunakpon Vihotogbé Léon Samuel Boris, Pediatric Surgery Department, National University Hospital, Hubert Koutoukou Maga, Cotonou, Benin
Received: September 11, 2023 | Published: October 4, 2023
Citation: Gogan MVLSB, Lafia KT, Metchihoungbé CS, et al. Management of right posterolateral congenital diaphragmatic hernia in a resource-limited country. case report and review. Int J Fam Commun Med. 2023;7(5):172-174. DOI: 10.15406/ijfcm.2023.07.00334
Congenital right diaphragmatic hernia is rare and often has a guarded prognosis when the liver is intrathoracic. The clinical case presented is that of a right posterolateral diaphragmatic hernia with the liver up, which highlights the importance of a chest X-ray in the face of neonatal respiratory distress and early management as soon as clinical stabilization is achieved.
Keywords: right diaphragmatic hernia, congenital, intrathoracic liver, neonate
Congenital diaphragmatic hernia (CDH) is a congenital anomaly in which abdominal viscera protrude into the thoracic cavity through a congenital diaphragmatic gap.1,2 It results from incomplete closure of the pleuroperitoneal membrane during fetal development.3 The protrusion of the abdominal viscera into the thoracic cavity affects the normal development of the lungs and is responsible for pulmonary hypoplasia and pulmonary hypertension. These pulmonary lesions, together with associated malformations, make this a serious condition with a high morbidity and mortality rate, despite the progress made in its management.4–6 The incidence of this condition ranges from 0.8 to 5/10,000 births, and varies from one population to another.7–10 Depending on anatomical location, HDC can be divided into three categories: posterolateral, anterior and central.11 Posterolateral CDH, also known as Bochdalek's hernia, is the most common (70-75%) and is highly fatal. It is rarely located on the right side (13%), with increased mortality, especially when the liver is intrathoracic.12–17 In line with the updated criteria for Surgical Case Reports (SCARE),18 we present the case of a neonate with a right Bochdalek hernia with intrathoracic liver, managed in our unit with a good outcome.
Patient presentation
Male neonate seen on day 6 of life and referred from a peripheral center for persistent neonatal respiratory distress. The father and mother were 26 years old and had no chronic pathologies. Delivery was by caesarean section at 41 SA + 5 days, with cephalic pole extraction of a newborn crying APGAR 9-10-10 and weighing 3100 g. Amniotic fluid was clear.
Clinical findings
On physical examination, the newborn was in moderate general condition, pink with good spontaneous gesticulation. He had a slightly globular chest on the right, superficial polypnoea at 81 cycles/min, with pulsed oxygen saturation of 91% on 0.5 l/min oxygen. The Silverman score was 3/10. Hydroaerobic sounds were heard in the right hemithorax on auscultation, and there was no rales. He was hemodynamically stable and the abdomen was discreetly retracted to the right. The rest of the examination was unremarkable, and there were no other clinically detectable malformations.
Diagnosis assessment
A thoracoabdominal X-ray, with the nasogastric tube in place, showed digestive clearing in the right hemithorax associated with right pulmonary hypoplasia. The hepatic shadow was not present in the right flank (Figure 1a & 1b).
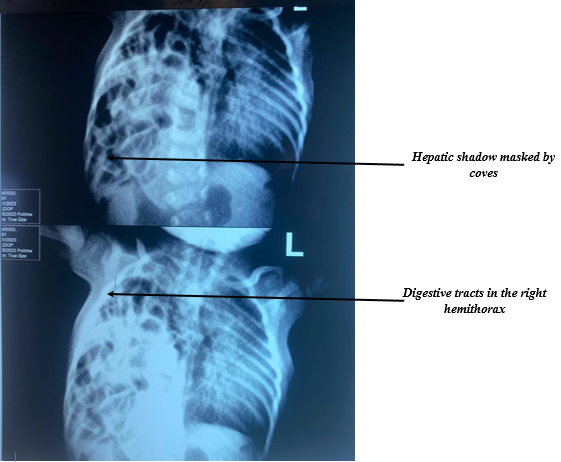
Figure 1 Thoracoabdominal X-ray showing the presence of a loop in the right hemithorax and herniation of the liver.
Therapeutic intervention
After medical resuscitation, he was taken to the operating room. After a right supra-umbilical transverse laparotomy, exploration revealed almost all the small intestines, the cecum, the ascending colon and the left liver in the thorax through a right posterolateral diaphragmatic breach. Intra-abdominal reintegration of the liver, herniated anses and resection of the hernia sac were performed. The defect measured approximately 6 cm x 4 cm (Figure 2). On the right, two lobes of the lung had a good macroscopic appearance, and the loops were intact. The diaphragmatic defect was sutured with tension-free non-absorbable suture after placement of a chest tube.
Follow-up and outcome
The immediate post-operative course was straightforward, with removal of the chest tube on day 4. Respiratory autonomy was achieved on day 15, and the newborn was discharged on postoperative day 21. The outcome was favorable, with a follow-up of 6 months.
Congenital diaphragmatic hernia is an embryofetopathy characterized by the presence of a diaphragmatic embryonic defect(s). Studies of European and Anglo-Saxon malformation registers reveal an incidence of between 0.8 and 5/10000 births.7–10 This incidence varies from one population to another, with a slight male predominance (sex ratio of 2).2,19,20 The malformation accounts for 8% of all congenital anomalies, with an overall infant mortality of 2%.21 Due to the protrusion of the abdominal contents into the thoracic cavity, the normal development of the lungs is affected, resulting in global pulmonary hypoplasia of variable severity and pulmonary hypertension. These lesions account for the severity of the pathology.
Depending on the location of the diaphragmatic defect, CDH at the level of the domes may be left, right or bilateral. Posterolateral CDH, also known as Bochdalek's hernia, is the most common (70-75%), and is highly fatal. It is rarely located on the right side (13%), as in the clinical case, with increased mortality in this case, especially when the liver is intrathoracic.12–17
Our patient, presented with a right Bochdalek hernia with part of the liver intrathoracic. He was seen on the 6th day of life with persistent neonatal respiratory distress. No antenatal ultrasound scan had been performed. This delay in diagnosis and treatment, linked here to the absence of good obstetrical monitoring of the pregnancy and a delay in immediate neonatal paraclinical investigation, is common in our context. Antenatal diagnosis, if carried out, would enable us to determine the degree of severity of the malformation, to search for associated malformations, and to plan follow-up and immediate antenatal and postnatal care. Prenatal management has improved considerably with the development of imaging techniques that enable us to assess the degree of pulmonary hypoplasia by measuring the LHR, and to decide whether or not fetal tracheal obstruction is necessary by fitting a Plug. This management increases the newborn's chances of survival.
Prenatal diagnosis of right HDC remains difficult in antenatal care, according to the current literature, because unlike left HDC, right HDC can present as heterogeneous masses in the thoracic cavity.2,11,22 According to Jani et al., this difficulty is increased prenatally by ultrasound in cases where the liver is the only organ to have herniated, due to its echogenicity similar to that of the lungs.23 However, Hedrick et al. in Philadelphia were able to make the diagnosis prenatally in 81.5% of cases.22
In the absence of prenatal diagnosis, neonatal respiratory distress remains the key symptom of this pathology at birth, as presented by the present patient. This respiratory distress associated with decreased respiratory sounds on the side homolateral to the hernia, a retracted abdomen and a shift in heart sounds to the contralateral side are key diagnostic symptoms.23 The thoracoabdominal X-ray at birth shows digestive clearing in the thorax, as on our patient's X-ray, and a mediastinal shift.24–27 These signs in our patient led to the diagnosis.
As the current consensus is to operate on more stable patients,3 the newborn was stabilized and taken to the OR by laparotomy. Several thoracic and abdominal approaches are now described, including minimally invasive ones. The limited technical resources at our center justified open surgery, which was performed by right subcostal laparotomy. The liver and coves were intrathoracic and were reduced. The right posterolateral defect was of moderate size, allowing repair without a prosthetic patch. When possible, patchless repair remains the choice of several teams, as it would reduce the recurrence rate and negligible complications.2
Despite advances in the medical and surgical management of HDC, mortality and morbidity remain high.20 The mortality rate ranges from 30% to 60% for isolated HDC and up to 89% for forms associated with other structural or chromosomal abnormalities.3,4 This mortality is higher in right HDC than in left HDC, as described in several studies (50% versus 75%).28 The survival of the patient in this case, despite the lack of technical facilities for neonatal resuscitation, could be linked to less severe hypoplasia of the lungs, the moderate size of the diaphragmatic defect and the presence of a hernia sac. According to several authors, these factors contribute to the morbidity and mortality associated with diaphragmatic hernia.
Right-sided diaphragmatic dome hernia remains rare and highly fatal, especially in countries with a poor technical platform and when the liver is intrathoracic. The present case highlights the importance of chest radiography in all cases of neonatal respiratory distress, for early diagnosis and management.
None.
The author declares there is no conflict of interest.

©2023 Gogan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.