International Journal of
eISSN: 2577-8269


Case Report Volume 4 Issue 3
1Department of Epidemiología, Universidad del Cauca, Colombia
2Department of Radiología, Universidad del Valle, Colombia
Correspondence: Fabricio Andrés Lasso Andrade, MD Universidad del Cauca Esp Epidemiología- Universidad Autónoma de Bucarmanga, Cra 2 #12-18 Valle del Guamuez-Putumayo, Colombia, Tel 3142638921
Received: March 27, 2020 | Published: May 11, 2020
Citation: Andrade FAL, Arteaga AC. Conservative management of unusual bullet embolism in the internal iliac vein. Int J Fam Commun Med. 2020;4(3):70-72. DOI: 10.15406/ijfcm.2020.04.00187
The embolism by projectile of firearm in the peripheral venous system, is a rare event, in which its diagnosis is often incidental. The embolisms in the venous system are much rarer than in the arterial system, representing only 4% of reported cases. We present the case of a 31-year-old patient with multiple gunshot wounds, one of them in the thorax with initial location of the bullet in the cervical region adjacent to the right internal jugular vein, with subsequent migration to the ipsilateral internal iliac vein. In this case, the patient remained asymptomatic with conservative management.
Keywords: bullet embolism, penetrating vascular injury, gunshot wound, ballistic trauma
The embolism by projectile of firearm in the vascular system, is an exceptional event. The embolism can be arterial or venous, being more frequent the incidence of arterial embolism, representing 80% of the cases. Its incidence is uncertain, but it is estimated that it oscillates around 0.3%.1,2 The places of the vascular system involved are usually the right ventricle, pulmonary arterial tree, aorta and the femoral system.3 The diagnosis is based on clinical suspicion in patients with gunshot wounds with the help of diagnostic imaging, which often means that the diagnosis is made incidentally. We present a case of bullet embolism of the right internal iliac vein due to a gunshot wound to the chest.
A 31-year-old man with no previous medical history was taken to the emergency department after suffering multiple injuries from a firearm, a chest wound and two in the right upper extremity, at a distance of approximately 8 meters, the gun caliber is unknown. The patient was alert, oriented with Glasgow 15/15 coma scale, normal vital signs, central and peripheral pulses, strong and symmetric, hemodynamically stable and negative shock index. The physical examination showed wounds with an entrance and exit hole in the proximal third of the right upper limb, another entrance and exit hole at the level of the hand of the same extremity. An entrance orifice was identified in the right deltoid region, without exit orifice. No wound had hard or soft signs of vascular injury. The initial chest radiograph shows a projectile in the right cervicothoracic region, without other findings (Figure 1). At six o'clock a new chest X-ray is performed, in which the projectile is not observed in the initial position (Figure 2). Radiography of the neck is performed, where the absence of the projectile is verified in the cervicothoracic space (Figure 3), but the abdomen radiograph shows the projectile in the right iliac fossa Figure 4(A,B). The follow-up with computed tomography without and with contrast of abdomen and pelvis showed the projectile lodged in right internal iliac vein (Figure 5). A grayscale and Doppler ultrasound study of the neck showed a small hematoma in place where the projectile was initially lodged without clearly demonstrating the path of communication with the right jugular vein by ultrasound. Because the patient was asymptomatic, the decision was made to treat the patient conservatively. After 2 years of follow-up, the patient remains asymptomatic.

Figure 1 Chest radiography of admission to the emergency room, it is verified that there is no intrathoracic lesion secondary to wound by firearm. In the right cervical region, a foreign body with a metal density compatible with a firearm projectile is identified. The position of the projectile was correlated with lateral chest X-ray.
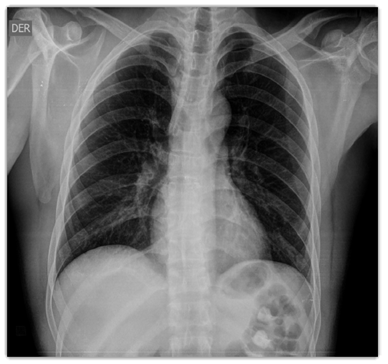
Figure 2 Chest x-ray taken 6 hours after admission as a protocol of the Trauma Unit, in which the projectile is not visualized in the right cervical region.

Figure 4(A) Radiography of abdomen in frontal (A) and lateral (B) projection in which projectile is visualized, housed in topography of the right internal iliac fossa.

Figure 4(B) CT of the abdomen in the bony window, coronal (A) and sagittal (B). A projectile (P) lodged in the right internal iliac fossa is observed at the level of the Sacral 1 vertebra. In the CT of the abdomen in the venous phase (not shown), the projectile was identified in the right internal Iliac vein.

Figure 5 Ultrasound of neck vessels. In transversal and climbing, the right internal jugular vein (IRYV) is identified and lateral to this is visualized a hypoechoic, oval zone of 1.5 cm compatible with small hematoma (H) where the projectile was lodged. In color and spectral Doppler mode arterial and venous flows of neck of normal characteristics were observed. The fistulous course between the hematoma (H) and the right internal jugular vein (IRYV) were not visualized in the US.
Davis in 1834 described the first case of embolism by projectile, in a 10-year-old boy with a gunshot wound, with a projectile located in the right ventricle of the heart, with subsequent embolism to the venous system. The majority of cases involve the arterial system, with anterograde migration; patients are usually very symptomatic due to distal ischemia. Venous embolism involves about 20% of cases. The majority of venous embolisms due to projectile migrate to the right chambers of the heart or pulmonary artery (83%), only 4% are located in the peripheral venous system.1,2 Large studies of vascular trauma show that the incidence of projectile embolization ranges between 0.3% and 1.1%, studies carried out during the Vietnam War, Afghanistan and Iraq.5,6 The diagnosis of intravascular projectile embolism should be based on the history of trauma from penetrating bullet wounds, which is incongruent the finding of entrance and exit wounds, as well as the unexpected trajectory of the missiles and the absence of direct injury of the tissue adjacent to the persistent location of the bullet, all this together with the help of diagnostic images.7 This case report demonstrates how a gunshot wound enters the right jugular vein and then migrates to the right internal iliac vein. The majority of projectile embolisms follow the blood flow. In this case, migration was retrograde to the peripheral venous system, which could be explained by the effects of gravity, which has been reported in 15% of cases.8
There is controversy in the management of embolism by projectiles, although in the case of arterial embolism, endovascular management is recommended, due to major complications arising from ischemia. The conservative management of embolism by projectiles in the venous system has been widely reported, mostly in asymptomatic patients.9 This patient remained asymptomatic, which is why conservative management was chosen. Complications of venous embolism due to retained projectile are numerous and include the destruction of heart valves, endocarditis, sepsis, venous thrombosis and thrombophlebitis. The majority of these complications occur years later.10 Our patient remained without complications after 2 years of observation.
None.
The author declares there is no conflict of interest.
None.

©2020 Andrade, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.