International Journal of
eISSN: 2577-8269


Case Report Volume 6 Issue 2
Department of Surgical Gastroenterology, Saptagiri Institute of Medical Sciences, India
Correspondence: Aswini K Pujahari, Prof and head, Department of Surgical Gastroenterology, Saptagiri Institute of Medical Sciences, Bangalore 560090, India, Tel 09632469433
Received: February 25, 2022 | Published: March 22, 2022
Citation: Pujahari AK. Chronic unilateral leg warty lesion: clinical image and literature review. Int J Fam Commun Med. 2022;6(2):59-60. DOI: 10.15406/ijfcm.2022.06.00265
54 years old diabetic male presented with history of with painless multiple progressive warty lesions on the right lower two third of the left leg remain undiagnosed for twelve years. It was spreading and growing relentlessly, not responding to medication prescribed by multiple doctors and patient thought of a uncurable disease. The biopsy came confirmatory. Antifungal therapy along with surgical excision hasten up the healing. An adequate biopsy is a must in undiagnosed skin lesion. Specific medical therapy and adjuvant surgery give early relief.
Keywords: leg lesion, painless warty lesion, long-duration lesion, chromoblastomycosis
A 54-year-old male, a paddy field worker getting often gets minor injuries on the legs, had presented with progressive cutaneous warty lesions on his lower right leg of 12 years duration. The lesion was exophytic, painless, progressive and spreading in nature. On pressure during examination, thick white discharge was noted, however there was no evidence of blood or pus discharge. He was diagnosed to be diabetic seven years back and was on oral hypo-glycaemic agents. It started as an elevated reddish nodular lesion on the lateral margin of the right foot. There was no pain or itching, he felt that it was oozing watery fluid. The swelling kept on increasing in number and size on the leg with time. He consulted multiple doctors, who prescribed oral medicines but it had no effect and it kept on increasing in numbers as well as size of the warty lesion. There were no constitutional symptoms during whole period.
On examination, the limb was hyper pigmented and swollen compared to the other limb. There were multiple warty lesions, many of them had conglomerated to form a large cauliflower like masses at places. It was involving only the lower two third of the leg without involving the weight bearing part of the sole. The lesions towards the knee were healing at places (Three views of the leg-Figure 1). There was no local rise of temperature, firm to feel, non-tender and on pressure thick, white sticky fluid was oozing out (Arrow in the Figure 1). There was no significant inguinal lymph node enlargement. He had superficial hypo-pigmented lesion on his back that of Taenia furfur (Figure 2). On investigation, the haematological and biochemical parameters including renal, and liver functions were normal except for hyper-glycemia with HbA1C of 7.9gm%. He was negative for retroviral serology. The micro photograph of the same (Figure 3) showing area with fungi (white arrow) surrounded by inflammatory tissue in the form of a granuloma and was reported as Chromoblastomycosis.
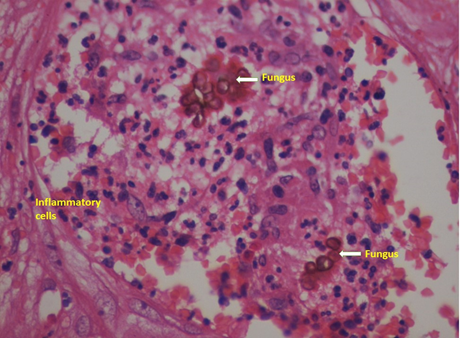
Figure 3 The micro photograph of the same (Figure 3) showing area with fungi (white arrow) surrounded by inflammatory tissue in the form of a granuloma and was reported as Chromoblastomycosis.
Chromoblastomycosis is a chronic fungal skin and subcutaneous tissue infection. It is seen worldwide but more common in the tropics. These are group of melanized fungi and cause pigmentation on the skin.1 Present case had black pigmentation on the affected right leg clearly visible in comparison to the left (Figure 1). The main pathogens are Fonsecaea pedrosoi, Phialophora verrucosa, Cladosporium carrionii, or Fonsecaea compacta.2 It is relatively rare clinical condition and hence clinical diagnosis is difficult. It is mostly nonfatal and continues for long duration up to 36 years before starting the therapy.3 Besides the typical presentation like the present patient, they might have, painless papules or nodules appear in the affected area progressing to scaly and verrucous plaques. Once the fungal agents enter the body part, small lesions comes up and it grows slowly for long time. The response to a single antifungal agent is not adequate and hence combination therapy is preferred.7 As the present case came after twelve years of the disease, we considered him as a severe case and advised surgical excision and electrocautery application to the subcutaneous tissue and started on two antifungal therapies. The drugs are itraconazole 200 mg twice daily and terbinafine 500mg per day initially. After a month the itraconazole was reduced to 200 mg daily once he responded to the treatment and advised to continue after 3 months of disappearance of all lesion. Besides the antifungal agents he has under gone two sessions of surgical excision and electro cauterization. On follow up, 3 months after the combined therapy showed good results, with reduction in the number of lesions (Figure 4). The follow up haematological and biochemical parameters has not shown any drug induced toxicities. In a small group of six patients pulse therapy of 400mg of itraconazole once a day and terbinafine alternate week were found to be effective and with less side effect and found no haematological and biochemical changes.7,8 The optimum duration of antifungal therapy is not fixed. It is given as per the response of the patients. But as per the literature antifungal therapy is recommended to continue till the tissue culture/ histology shows no fungi.8 The most common complications of chromoblastomycosis are ulceration, secondary bacterial infection, lymphedema that leads to elephantiasis and myiasis.9 Rare cases of malignant transformation to squamous cell carcinoma have been documented.10
Biopsy is diagnostic in long standing undiagnosed skin lesion. Chromoblastomycosis showing the fungal agent confirm the diagnosis. Two oral fungal agents give good response. Surgical excision restores the leg earlier.
None.
The author declares there is no conflict of interest.

©2022 Pujahari. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.