International Journal of
eISSN: 2577-8269


Case Report Volume 5 Issue 1
1Scientific Association of Medicine Students of the University Andina of Cusco, Cusco, Perú
2Thoracic and Cardiovascular Surgery Service, Hospital Nacional Adolfo Guevara Velazco. Cusco, Peru
Correspondence: Junior Julio Zapata Choque, Scientific Association of Medicine Students of the University Andina of Cusco, Cusco, Perú
Received: December 31, 2020 | Published: January 13, 2021
Citation: Choque JJZ, Latorre JCE, Sandoval CNN. Bilateral pulmonary hydathidic cyst with fatal outlet: a case report. Int J Fam Commun Med. 2021;5(1):11-13. DOI: 10.15406/ijfcm.2021.05.00213
Hydatidosis is a parasitic zoonosis caused by Echinococcus Granulosus, its life cycle includes dogs, sheep and others; liver involvement is the most frequent (65%-75%), followed by the lung (10%-25%), in Peru the pulmonary location is 60%. Its signs and symptoms are produced by the mass effect, its superinfection or anaphylactic reactions secondary to its rupture. We present the case of a 24-year-old insulin-dependent patient with type I diabetes mellitus, hypertension and diabetic retinopathy with bilateral pulmonary hydatidosis. A cystectomy was performed without complications and a lobectomy that was complicated with admission to the ICU until the death of the patient. Diabetes mellitus causes a state of immunosuppression which caused the advanced state of the patient's parasitosis, as well as being related to multiple intra- and postoperative complications and even leading to the death of the patient.
Keywords: echinococcosis, echinococcus granulosus infection, diabetes mellitus, insulin dependent (Source: MeSH NLM)
Hydatidosis is a zoonosis produced by the larval forms of the cestodes of Echinococcus Granulosus;1 which has the dog as its definitive host, which after eliminating the eggs through their feces are disseminated to the environment and these will be ingested by intermediate hosts such as sheep and accidentally by man through contaminated food,2 they can have various locations, 60% are pulmonary and of this in 82% unilateral lesions are appreciated.6 In Peru, between 2001-2006 hydatidosis affected seven to eleven people per 100,000 inhabitants, occurring more frequently in the regions of Junín, Cerro de Pasco and Huancavelica, with prevalences of 14 to 34 cases per 100,000 inhabitants3–7 in the city of Cusco no epidemiological reports are mentioned. In treatment, 97% of cysts need surgical treatment either by conservative or radical surgery according to the behavior of the cyst; radical surgeries lead to more postoperative complications.8 Type I diabetes mellitus (DM1) is a chronic disease characterized by the partial or total destruction of the beta cells of the islets of Langerhans, producing an inability to produce insulin; in addition to having acute and chronic complications such as arthropathy, nephropathy, neuropathy, retinopathy and increased cardiovascular risk.9 Hyperglycemia, hypoglycemia, and high glycemic variability aggravate the pathological states of patients and increase the incidence of adverse events related to surgery in the pre- and postoperative period.10 We present the case of a 24-year-old patient from Puerto Maldonado, Peru with a history of insulin-dependent DM1 and bilateral pulmonary hydatidosis, who underwent 2 surgical interventions: an uncomplicated cystectomy and a lobectomy that, presenting many postoperative complications, led to death of the patient due to acute respiratory failure.
A 24-year-old male from Puerto Maldonado with a history of insulin-dependent Diabetes Mellitus I (DM1) for 19 years, diabetic retinopathy, arterial hypertension and bilateral pulmonary hydatidosis for 2 years; He arrived at the emergency service due to a 3-month illness period characterized by moderate chest pain and dyspnea on medium efforts, which increased in the last 15 days; A physical examination was carried out, where the abolition of the vesicular murmur was observed in the middle 1/3 of the right hemithorax and, based on the left hemithorax, his hospitalization was subsequently indicated for further auxiliary tests. A Computed Tomography of the Thorax was indicated (Figure 1) where images suggestive of pulmonary hydatid cysts were observed and then an evaluation of the specialty of Thorax and Cardiovascular Surgery was requested for the management of the patient. It was decided that the patient should enter surgery at two different times to undergo surgical treatment; days later, the patient underwent the respective preoperative examinations of pneumology (Pneumological Risk III/IV), cardiology (Cardiological Risk III/IV) and anesthesiology (ASA III) and the technique of the first operation between a Cystectomy vs Lobectomy was evaluated; While waiting for the date of the first surgical intervention of the left pulmonary cyst, since it could become complicated, the patient was managed with Captopril (25mg PRN at BP ≥140 / 90), insulin NPH 20U SC in the morning and Crystalline Insulin 5U later of meals, despite treatment, the patient had poor glycemic control (180-340 mg/dl), which is why the dose of NPH insulin is increased to 15U in the morning and 10U at night, after evaluation by endocrinology.
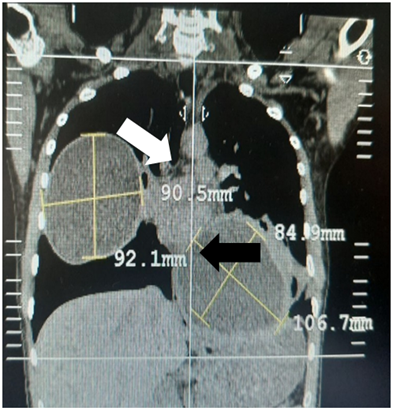
Figure 1 Multislice Spiral Tomography shows 02 cystic images, one in the right hemithorax with liquid content (white arrow) and another in the left hemithorax with liquid content (black arrow) of 9.05 cm x 9.21 cm and 8.49 cm x 10.67 cm respectively, thus as a pneumoperichst suggestive of a cystic lesion in the process of rupture.
The first surgical intervention is carried out 12 days after the patient's admission where the airway is managed with a double lumen endotracheal tube (ETT) to minimize complications in surgery; A thoracotomy + left cystectomy is performed and a pericystic bag measuring 10cm x 8.4 cm in diameter was removed (Figure 2), 2 thoracic drains were left and he left the operating room 3 hours later without complications, hemodynamically stable and with spontaneous ventilation. The postoperative period was managed with some complications typical of the patient's diabetes because he presented episodes of hypoglycemia which were managed with 33% dextrose and hyperglycemia that were managed with Insulin Lispro 5U before meals and Insulin Gliargine 20U morning and 10U night; 12 days after the surgical intervention, the patient was discharged without complications after control with chest X-ray and removal of the 2 thoracic drains in addition to having treatment with Albendazole 250mg/12hrs until the next surgery. Two months later, the patient returned for his second surgical intervention on the right side, in the preoperative period he returned with alterations in glucose values which caused the surgical intervention to be canceled 2 times, these alterations were controlled together with endocrinology and 7 days Later, he entered the operating room where the airway was managed again with a double lumen ETT and a thoracotomy + right upper lobectomy was performed and two thoracic drains were placed.

Figure 2 Pericystic membrane removed in the first intervention: Left Thoracotomy plus cystectomy in the left lower lobe (10.67 cm x 8.4 cm).
During the operation, the patient presented an inability to spontaneously ventilate with glucose of 220mg/dl, so he remained in sedation and later entered the Intensive Care Unit with a BP: 93/63, HR: 103 and RR: 12 (with mechanical ventilation) with rhonchi and rough breathing for postoperative management. With this evaluation, the diagnosis of Acute Respiratory Failure, decompensated type I diabetes mellitus and septic shock to pulmonary focus is reached. The necessary management was carried out and the patient presented a favorable recovery with respiratory physiotherapy and pulmocare 1 can every 12hrs that contributed to the extubation of the patient, but 2 days later he began to present compromise of the sensorium state with a BP: 80/50, HR : 130 and glucose values of 350 to 450mg / dl plus a metabolic acidosis, a control chest X-ray is requested (Figure 3) and the diagnoses previously raised are handled again this time without patient improvement apart from vasopressor support, 3 days later he presented a BP: 170/90, HR: 150 with Ventricular Tachycardia evolving to Ventricular Fibrillation and despite the efforts to stabilize it, he died in the ICU.
Echinococcosis is a neglected disease because it manifests itself mainly in rural areas and poor populations of Peru and is considered an endemic country of hydatid cyst mainly in the Andean region; since, between 93-95% of cases of this anthropozoonosis come from this region,4 what is striking in this case is that it corresponds to a jungle area where the disease is not endemic. It can affect any part of the body, the most common being the liver and, secondly, the lungs3 being the location of the patient's cysts; most cysts are unilateral Gonzales et al. In his study carried out in Peru, he mentions that approximately 82% show unilateral injuries,6 therefore the importance of the case presented resides in the bilaterality of the injury. The diameter of both cysts was greater than 8 cm and when it is greater than 8 cm according to the study by Aldahmashi et al. They are more related to complications that can manifest with vomica, empyema or pneumothorax,11 which we did not observe in our patient, which course with cough, chest pain, and mild respiratory distress and that symptomatic patients, who are the majority, go to hospital when are presented.5 The surgical technique used in our patient was cystectomy + capitonage in the 1st surgery and a lobectomy in the 2nd, it should be noted that the surgical techniques are conservative (cystectomy, parasitectomy) and radical (segmentotomy, lobectomy or pneumonectomy) that according to Rafael et al. In his study in Peru, he showed that 14.6% and 21.7% respectively are associated with complications such as atelectasis in 66%, bronchopleural fistula in 12% and respiratory failure as presented by our patient after the 2nd surgery in only 6%.4
Type 1 diabetes mellitus (DM1) is a complex genetic trait. Once the clinical diagnosis of DM1 is reached, the process of immune damage is already so advanced that it is considered a state of immunosuppression and in the particular case of septic patients it is associated with suffer events of an advanced infectious and parasitic nature.14,15 Our patient has a history of DM1, and in both surgeries he presented episodes of hyperglycemia that were controlled with the treatment described in the preoperative period and which followed the schedules that the patient received, which is consistent with the study carried out by Nazar et al.12 where it mentions that glucose alterations in an insulin-dependent patient in the preoperative period are managed with NaCl, Insulin R and Dextrose + EV potassium.12 The decompensation in glucose values leads the patient to develop infections in 6% due to the state of immunosuppression that is more severe in a patient with DM1 like ours;13 In the 2nd postoperative period, our patient was admitted to the ICU with respiratory failure, decompensated Diabetes Mellitus and, after intensive management, it was complicated by in-hospital pneumonia that led to death despite having improved and being on respiratory physiotherapy.
None.
The author declares there is no conflict of interest.

©2021 Choque, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.