International Journal of
eISSN: 2577-8269


The Giant Ovarian Cyst is not frequently seen, usually benign tumor, which eventually become malignant. It grows up slowly, free symptoms despite of some constipation, breath difficulties, and lose weight. At the beginning sonogram could miss the diagnosis, it usually be docne by Axial Tomography, and needs surgical procedure by laparoscopy if they are less than 10 centimeters in diameter or laparotomy whenever longer to spread avoided.1,2
The Giant Ovarian Cyst is no frequently, as mama and uterus tumors are. The most common ovarian cyst is less than 7 centimeter and uses to be bilateral. 75-80% are benign tumors but at the time, they could became malignant because of the ovarian function is always present to generate tumors. About 10% of the women could have some cysts in their lifetime and eventually surgical resection will needed. The Giant Ovarian Cyst may occupied all abdominal cavity, and the symptoms use to be as an abdominal mass, with some intestinal constipation, lose weight, renal failure, diaphragmatic elevation with some breath, circulation and walk difficulties.3,4
Single 38 Female (Figure1), who went to check it out for breath difficulties, weakness, abdominal mass growing and lose weight in about 35 kilos last year5
No Personal Pathologic History
Personal no pathologic History: Just smocking.
Gynecological History: P=0 M13 R=irregular. Sexual Life Beginning: 18 years old, no contraception methods carry on.6
Physical exploration
Female, thin, good oral mucosa hydration, limited moves to breathe, no cardiac problems. Abdominal wall prominent, peristaltic sound only heard in upper left side, diffuse mate noise in all abdominal cavity at the percussion exploration. Laboratories: Hb 10g/dl, Hto 30 WBC 10,300. N 56% Plaq 230,000 Glucose 89 mg/dL Na 135 mEq K 4mEq Cl105mEq. Axial Tomography (Figure 2 and Figure 3): shows a very big intraabdominal homogeneous mass, from de left ovarian pulling all organs to superior left abdominal quadrant
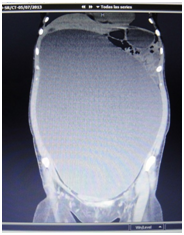
Figure 2 Axial Tomography shows Giant Ovarian Cyst, with intrabdominal organs in uper left quadrant.
In the operating room (Figure 4), a laparotomy made from the xiphoid to the pubic bone (Figure 5), under general anesthesia, the findings were a very big left ovarian cyst, taking out with left adnexalectomy. It was 14 kilos weight (Figure 6). Right ovarian normal aspect size 2.5 x 3 centimeters, biopsy had taken, the others organs looks normal. Postoperative course was uneventful and the patient discharged home. Pathological report: Serous left Ovarian Cystadenoma, no malignancy. The pictures had aggregated.7
The Giant Ovarian Cyst are no common, and in obesity, frequently are misdiagnoses as ascites and should always considered in differential diagnosis or abdominal cavity enlargement at reproductive age Initial sonographic evaluation can fail to diagnose correctly. Axial Tomography confirms diagnosis. They are named Giants Cyst whenever they are more than 12 kilos weight and almost 85% are benign, but 30% could become to malignant, that is the reason to take complete them out to spread avoided. Just watching them is not enough to say is benign or malignant; they must have to see for the Pathologist. Whenever the size is 10 centimeters in diameter or less, they can be removing by laparoscopy surgery.8,9
The Giant Ovarian Cyst, not frequently and usually benign tumor must suspect at reproductive age asymtomatic female enlarge abdominal wall. Diagnosis done by axial tomography. Laparatomy considered to spread avoid and handle with care. It should take a very big surgical incision.
None.
The auhtor declares there is no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.