International Journal of
eISSN: 2577-8269


Case Report Volume 2 Issue 3
1Department of Otolaryngology, High Specialty Medicine Unit of the Northwest, Mexico
2Department of Pediatric Oncology, Regional General Hospital, Mexico
Correspondence: Juan Antonio Lugo Machado, Department of Otolaryngology, Medical resident of 2nd year of ENT, High Specialty Medicine Unit of the Northwest, Mexico, Tel 6441559891
Received: May 12, 2018 | Published: May 23, 2018
Citation: Espinoza INR, Machado JAL, Félix IO, et al. Maxillofacial tumor as manifestation extramedullary acute myeloid leukemia in children presentation of a clinical case. Int J Fam Commun Med. 2018;2(3):150-151. DOI: 10.15406/ijfcm.2018.02.00058
Acute myeloid leukemia (AML) can present as an extramedullary variety (AML-MS) with or without bone marrow disease.1–4 Myeloid sarcoma (SM) is defined as an extramedullary tumor composed of myeloid blasts in an anatomical location other than the bone marrow with the potential to infiltrate the liver, spleen, lymph nodes and brain. The participation of other sites is rare. The most common places include soft tissues, bones and periosteum. The clinical manifestations are diverse given the different sites of occurrence, with signs and symptoms determined by their location and size.2–5 Here we describe the case of a child of one year and 5 months of age, whose initial presentation was volume increase in right and painless maxillofacial region accompanied by nasal symptoms
Keywords: maxillary tumor, extramedullary, myeloid leukemia acute infantile, maxillofacial region
The aim of this article is to describe an unusual case of AML-MS, which appeared as a maxillofacial tumor. Allen Burns was the first to describe this type of injury in 1811 as a green colored tumor that affected the orbit.6 Due to its characteristic green color; King in 1853 named it chloroma (meaning green in Greek "chloros") chloromas. Exposure to ultraviolet light of the myeloperoxidase enzyme present in this type of tumor cells is responsible for the coloration, SM develops in 1-8% of patients with AML and in 16% of cases in the head and the neck.The main classification of tumors of haematopoietic and lymphoid tissues according to WHO is based on a combination of clinical, morphological, immunophenotypic, genetic and biological characteristics, should have: a logical approach similar to that followed by a doctor and pathologist, since works together to arrive at a diagnosis in a patient suspected of having a hematopoietic neoplasm. Hematopoietic neoplasms are widely stratified according to the lineage of the neoplastic cells, that is, myeloid, lymphoid, histiocytic/dendritic or ambiguous lineage. The latter category is composed of neoplasms of precursor cells (acute leukemia) that are formed by cells that lack a specific lineage associated markers and therefore are "undifferentiated", or that express antigens of more than one lineage, and thus appear to have a mixed lineage phenotype. Neoplasms composed of precursor cells (acute myeloid leukemia, leukemia/lymphoblastic lymphoma, neoplasm of blast plasmacytic dendritic cells and acute leukemia of ambiguous lineage) are considered separately from the more mature cell compounds (myeloproliferative neoplasms, myelodysplastic/myeloproliferative neoplasms, myelodysplastic syndromes, lymphocytes of B lymphocytes and mature T/NK lymphocytes, Hodgkin lymphoma and histiocytic/dendritic cell neoplasms). For mature lymphoid neoplasms, further sub classification and listing is based to some extent on the stage of differentiation compared to a normal homologous postulate (eg, mantle cell lymphoma, follicular lymphoma), on morphology (eg, diffuse lymphoma) of large B cells), in clinical presentations or the clinical setting (eg, large diffuse B cells), lymphoma associated with chronic inflammation), or more commonly, in the combination of morphological, immunophenotypic and / or genetic parameters that together allow a disease specific entity to be defined (eg, anaplastic large cell lymphoma, ALK positive.) For the myeloid neoplasm, an additional sub-classification is based mainly on its maturation pattern and general biological characteristics.1–7
Pediatric patient of 1 year 5 months of age, Hospitalized in the oncology pediatric service for clinical picture of 5 months of evolution characterized by volume increase in right maxillofacial region, hyaline rhinorrhea in sometimes greenish of right nostril, ipsilateral epiphora and febrile pictures . Pathological antecedent: a previous year was diagnosed with acute T-cell lymphoblastic leukemia (ALL) and received multiple chemotherapy schemes, the last report of bone marrow aspirate with morphological and molecular remission of ALL. During the treatment he presented infectious fungal diseases. They request interconsultation to otorhinolaryngology with diagnosis of right maxillary sinusitis, probably fungal. Physical examination showed an increase in volume in the right maxillofacial region with a hard, non-painful consistency, no changes in coloration, mild proptosis of the right eyeball. (Figure 1A) Anterior rhinoscopy: abundant hyaline rhinorrhea of right nostril and erythematous mucosa, no occupational tumor is observed.
Contrast MRI: increased volume of soft structures in the right half of the face, involves soft and muscular tissues surrounding the alveolar process of the right maxilla, displaces upward orbital floor structures and moderate soft tissue reinforcement. (Figure 1B) Simple CT: soft tissue volume increase in the medial wall of the right maxillary sinus that partially obstructs the nasal cavity, remodeling and bone infiltration of the anterior wall of the maxillary sinus and occupied by density to liquid (Figure 2A) (Figure 2B).
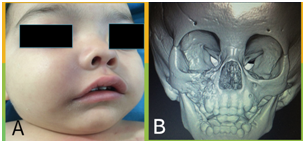
Figure 1 (A) Right hemicra volume increase, (B) Volumetric reconstruction: anterior wall and alveolar apofifis of the right maxilla with bone erosion as well as orbital floor.
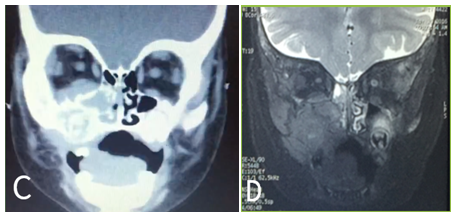
Figure 2 (A) Single CT scan of the coronal section: observe a tumor with soft tissue density located on the anterior side of the right maxillary sinus with apparent involvement of the nasal cavity, and extension to orbit as well as bone destruction. (B) MRI increased focal volume of soft structures in the middle of the right side involving soft tissue and muscle that surrounds the maxillary sinus, lower edge of the orbit and elevates the lower rectus muscle causing mild proptosis, intermediate intensity is observed with moderate restriction to the diffusion of water, which suggests high cellularity content.
A tumor biopsy was taken, using the right sub-labial approach (Figure 3A), finding the following findings: infiltrating lesion of the maxillary bone and soft tissues, softening of the cortex, presence of sallow and hemorrhagic fluid. Histopathological and immunohistochemical report: adipose and fibro-connective tissue with infiltration of diffuse neoplasia of medium and large cells, (Figure 3B) CD-20 negative, CD-3 negative, Myeloperoxidase positive 3+. Diagnosis: Acute extramedullary myeloid leukemia in right maxillofacial region. Start chemotherapy (Cytarabine, Cardioxane, Daunorubicin, Etopocide and Onicit).
The patient at the start of chemotherapy treatment shows a decrease in the size of the tumor and improvement of nasal symptoms; however it has complications secondary to chemotherapy (AraC syndrome and neutropenic colitis) and dies. The diagnosis of AML-MS in patients with established leukemia should always be included in the differential diagnosis if a soft tissue mass presents. Liron et al, 2005 reported that MS could occur in any of the following three clinical situations: 1) In patients who have a history of AML, during active disease or a recurrence; 2) In patients with chronic myeloproliferative disorders, or 3) In patients with no history of haematological disease, commonly prior to the onset of leukemia.6 To confirm the diagnosis the biopsy is necessary. Immunohistochemistry has historically been useful in establishing the definitive diagnosis in the absence of leukemic involvement in the bone marrow. Data on the prognostic significance of AML-MS are limited. Although the presence of AML-MS may be associated with a poor prognosis and a 5-year short survival rate from 20% to 30%. AML-MS is not a common presentation, but it is important that it is diagnosed early.3–5 SM are sensitive to local radiotherapy and in combination with chemotherapy a good result is obtained. Within the differential diagnoses, invasive sinusiti funica and neoplasias must be included.6
None.
None.
The authors declares there is no conflict of interest.

©2018 Espinoza, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.