International Journal of
eISSN: 2381-1803


Research Article Volume 16 Issue 5
1Principal Academic Adviser, School of Education, University of Southern Queensland, Professor of Vedic Science, Education and the Environment at Maharishi Vedic Research Institute, Australia
2Professor of Mathematics (formerly Mark Friedman), Department of Mathematics, Maharishi International University, Fairfield, Iowa, USA
3Clinical Professor of Physiology and Health at Maharishi International University, Fairfield, Iowa, USA
Correspondence: Dr Lee Fergusson, Principal Academic Adviser, School of Education, University of Southern Queensland, Education and the Environment at Maharishi Vedic Research Institute, Australia
Received: September 01, 2023 | Published: September 20, 2023
Citation: Fergusson L, Pekker M, Palakurthi M. Vikriti, Agni and health: a preliminary mathematical model of Ayurvedic treatment. Int J Complement Alt Med. 2023;16(5):259-270. DOI: 10.15406/ijcam.2023.16.00661
Ayurveda is a well-established form of alternative medicine. The terms Prakriti, Vikriti, Agni, and Koshta are well-known and their associations have been articulated in both the traditional literature of Ayurveda and by practicing Ayurvedic clinicians. These associations, while well understood and applied clinically, have not until recently been explored empirically. Correlational analysis has shown that these principles and processes of Ayurveda can be statistically observed in a large sample of patients. For example, Prakriti (the constitution of the body) and Vikriti (the current state of the body) are correlated to Agni (digestion) and Koshta (gut responsiveness), and results uniformly indicate that Vikriti is also associated to weight, body mass index, and diet, each an established cardiovascular disease risk factor.
The present proof-of-concept case study takes these topics to the next stage of empirical investigation aimed at formulating an approach to bring Ayurvedic research into mainstream Life Sciences and complementary medicine. The principal challenge here is in a gap between the paradigms of modern Life Sciences and Ayurveda. We propose bridging this gap by formulating a minimal phenomenological nonlinear dynamics model to account for the critical role Agni plays in the health of Vikriti and for a threshold-type improvement in both Agni and Vikriti during the process of a six-month Ayurvedic treatment.
Keywords: ayurveda, Vikriti, Agni, Koshta, mathematical modelling
The paradigm of modern medicine can be described as ‘bottom up’ healthcare as its practice is based on the conceptual framework of molecular biology, quantitative testing, and randomised statistical methods. Allopathic medicine builds its interpretive power and curative-palliative treatments upon these foundations.
The paradigm of Ayurvedic medicine, on the other hand, can be described as ‘top-down’ as its key theoretical concepts are of whole-system type. These concepts were developed as conceptualizations of operational definitions by highly sensitive Ayurvedic doctors (such as Charaka and Sushruta) and have been successfully used for treating patients and for training doctors over millennia. Here, an assessment of a patient’s health condition is based on the doctor’s evaluation of the patient himself or herself without using any devices and statistically applied normative standards.
Nonlinear dynamics is a relatively new area of mathematics. Its more recent developments include catastrophe theory, bifurcation theory, chaos theory, and numerical bifurcation analysis. Nonlinear dynamics models are widespread in science and technology, as they are suitable to account for both quantitative and qualitative phenomena.1 In particular, application of these models in biological and medical research has led to the emergence of new fields of research, such as systems biology and systems medicine.2Alon, 2019 At present, examples such as nonlinear dynamics in COVID-19 pandemic modelling3 and its application to climate research and sustainability science have become increasingly common.4,5
Our aim and approach:
The present proof-of-concept paper aims to make a preliminary case for the use of nonlinear dynamics modelling in Ayurveda. The authors hypothesize that such an approach has a potential to facilitate the integration of modern and Ayurvedic paradigms.
Mathematical models in modern medicine account for interactions between particular systems in the human organism. For example, in endocrinology, a typical model6 would account for interactions of certain endocrine glands via the hormones they produce; in autonomic medicine, one can consider neuronal reactants, such as amino acids, interacting via various neurotransmitters.7
The conceptual framework of Ayurveda, typically, does not include formal definitions of the concepts and relationship between their different elements, but uses qualitative and metaphoric descriptions. For example, in our case, we use phrases such as: “Vikriti refers to an individual’s current state of psychophysiological functioning”; “current condition of the body”; “current state of patient’s psychophysiology”; “Agni refers to the digestive system and its ‘digestive fire’”; and “Agni maintains equilibrium in Vikriti”.
The above brief discussion points to a gap between the paradigms of modern medical science and Ayurveda medicine, and that the mechanisms underlying Ayurvedic successes are largely unknown. These facts constitute the principal challenge to our project. Therefore, our first working hypothesis relates to constructing a minimal formal phenomenological conceptual framework to make our mathematical modelling possible.
Using a real-world patient case report as our starting point, we have formulated a minimal phenomenological nonlinear dynamics model to account for the relationship between Vikriti and Agni during the process of treatment, which is based on the traditional Ayurvedic theory of Charaka and Sushruta. Our model accounts for the crucial role Agni plays in the health of Vikriti wherein a small delayed, and then sharply increased, salutary psychophysiological effect can be observed as a response during six-months of Ayurvedic treatment.
The present study, which builds on earlier research by authors 1 and 3,8 concerns the Ayurvedic concepts of Prakriti (constitution of the body), Vikriti (current condition of the body), Agni (digestion), and Koshta (gut responsiveness), as influenced by the Doshas (or life energies), and considers their collective relation to cardiovascular disease (CVD) risk factors and health.
The published literature on Prakriti, Vikriti, Agni, and Koshta, and the fundamental contribution of Doshas to them, is extensive.9–11 These aspects of mind and body are detailed and explained in the essential texts of Ayurveda: Charaka Saṁhitā; Sushruta Saṁhitā; Vāgbhatt Saṁhitā; Mādhav Nidān Saṁhitā; Shārngadhar Saṁhitā; and Bhāva-Prakāsh Saṁhitā. The following operational definitions used in this study have been derived from these ancient texts.
Doshas: Charaka Saṁhitā explains the qualities of the three Doshas (Sūtrasthāna, I.59‒61). According to Verma et al.,12 the Doshas are the life energies which animate and give direction to human psychophysiology, and it is “only when the three life energies or doshas, that make up every individual’s constitution, are perfectly balanced can a person enjoy good health”. Charaka refers to the Doshas as the “life breathe of all living beings” and disease as their “obstruction” (Sūtrasthāna, XVII.115-118); elsewhere they are described as the “vital power” (Sūtrasthāna, XI.4). Therefore, it is the Doshas which influence the health of the mind and body. Ayurveda has identified three distinct types of metabolic and psychophysiological qualities: Vāta, which is associated with properties such as coldness, roughness, dryness, instability, and movement; Pitta, which is associated with properties such as heat, metabolism, sharpness, oiliness, and liquidity; and Kapha, which is associated with properties such as steadiness, stability, heaviness, reliability, and slowness.
According to Charaka, “Vāta, Pitta, and Kapha pervade the entire body and thus produce good or bad consequences when [respectively] non-aggravated or aggravated. In the normal [non-aggravated] state, they produce good consequences, such as development, strength, complexion, cheerfulness, and so on; but when in an abnormal [aggravated] state, they cause bad consequences, known as disorders or disease” (Sūtrasthāna, XX.9).
Vitiation: Sometimes referred to as Vṛiddhi or ‘increase’ in Ayurveda, is a measure of disorder in the Doshas. Vitiation is variously described as attenuation, elevation, aggravation, disruption, dissemination, corruption, or impairment (i.e., a disturbance of some property in the mind and/or body). Each of these possible conditions mean something specific in Ayurveda (for example, vitiation can relate to “accumulation, imbalance, or diminution”, Sūtrasthāna, XVIII.114), but for the purposes of this research, vitiation is taken to mean elevation (i.e., increase or accumulation) or it’s opposite, diminution. Charaka points out that in their “balanced or orderly state, the Doshas maintain the body; when vitiated they afflict the body with disease” (Vimānasthānam, I.5).
Prakriti: Refers to an individual’s permanent state of psychophysiological functioning and refers to the fundamental characteristics or traits of an individual’s mind and body; Charaka refers to Prakriti as Swabhāva or one’s “nature” (Vimānasthānam, I.21). Prakriti is fixed at birth and does not change throughout life and thus represents one’s innate constitution. There are ten possible Dosha combinations which can form Prakriti: Vāta; Vāta-Pitta; Vāta-Kapha; Pitta; Pitta-Vāta; Pitta-Kapha; Kapha; Kapha-Vāta; Kapha-Pitta; and Tridosha, when all three Doshas are present in equal proportion, which occurs at the time of birth. Chintala & Bhagavathi13 maintain that accurate diagnosis of Prakriti and its vitiated states (i.e., the vitiation of Vikriti, Agni, and Koshta) is important because it helps a physician “forecast illness susceptibility, severity of signs and symptoms, disease activity scores, and bio-markers, such as hematological, pathological, and biochemical indicators”.
Vikriti: Refers to an individual’s current state of psychophysiological functioning. Vikriti changes constantly, even during the same day, with different variations and levels of Doshas in the mind and body depending on diet, environmental factors and conditions, psychological states, etc. Prakriti and Vikriti are thus parallel, but different, states or conditions of the mind and body. Accordingly, “Prakriti…has no variation, whereas Vikriti has many [variations]” (Vimānasthānam, I.10).
Agni: Refers to the digestive system and its “digestive fire” (Vimānasthānam, VI.12). Charaka attributes the root cause of all disease to an imbalance or “derangement” of Agni, and ascribes one’s lifespan, complexion, strength, health, and “long life free from disorders” to it; “one dies if this fire is extinguished” (Chikitsāsthānam, XV.1). According to various other Saṁhitās (e.g., Vāgbhatt Saṁhitā, Nidansthan, 12.3), a diminished capacity of Agni (i.e., the hypo function of Agni called Agnimandya) is described as the “basic cause for the pathogenesis of diseases”.
Charaka states Agni is influenced by the Doshas and results in either Vishamāgni (irregular digestive capacity) when vitiated by Vāta, Tikshnāgni (intense digestive capacity) when vitiated by Pitta, or Mandāgni (low digestive capacity) when vitiated by Kapha. When all three Doshas are in balance, the result is Sāmāgni (balanced digestive capacity) (Vimānasthānam, VI.12). Sushruta similarly states that balanced Doshas in Vikriti are related to a balanced Agni (Sūtrasthāna, XV.41). The four Agnis will be explained in more detail in the following section of this paper. Of interest to the present study, Charaka also maintains that an equilibrium of Doshas in Vikriti can be maintained through Agni; in other words, a balanced Agni can affect the equilibrium of Vikriti.14,15 In these ways, Vikriti provides energy to Agni (i.e., can alter the normal functioning of Agni) and a balanced Agni provides equilibrium to Vikriti in a continuous feedforward and feedback loop, another core concept explored in this research. Thus, Agni is considered central to Ayurveda and to this study because it is the body’s “vital energy” (Chikitsāsthānam, XV.1).
Koshta: Refers to the alimentary canal and the responsiveness of the gut in relation to Agni; Koshta includes the current condition of the gut biome and the elimination system. Charaka refers to Koshta as “the great channel in the middle of the body” (Sūtrasthāna, XI.48), and identifies four main types. When the gut is vitiated by Vāta, the result is Krūra Koshta (infrequent bowel clearance); when vitiated by Pitta, the result is Mṛidu Koshta (quick bowel clearance); and when vitiated by Kapha, the result is Madhyāma Koshta (moderate bowel clearance). However, when all three Koshtas are in balance, the result is Sāmā Koshta (balanced gut responsiveness). Vāgbhatt also mentions these four types of Koshta (Sūtrasthāna and Ayushyakamiya-Adhya, I.8). Research suggests that a change in Koshta may affect the condition of Agni16 and the heart.17 The four Koshtas will be explained in more detail in the following section of this paper.
Cardiovascular disease: While not the main focus of this research, CVD risk factors and their management are an important part of modern life.18 In Ayurveda, a great deal of importance is been placed on the heart (Hridaya) and its health. For example, heart palpitations are associated with the vitiation of Vāta and obstruction in the heart is associated with the vitiation of Kapha (Chikitsāsthānam, XXVI.70-73).
For the purposes of simplicity, in this study we have only isolated three CVD risk factors—weight, body mass index (BMI), and blood pressure (BP)—as examples of variables affected by Vikriti, Agni and Koshta, but others are possible. Of relevance also are recent findings which link digestion and gut responsiveness to CVD risk factors, such as those of Ryan et al.19 and Aggarwal.16 For a more complete description of the relationship of Ayurveda to CVD, including hypertension and hypercholesterolemia.20
Irrespective of the type of imbalance, Charaka states that all three forms of disease—innate, exogenous, and psychological (Sūtrasthāna, XI.45)—are caused by ‘intellectual error’ (Sūtrasthāna, I.52) or ‘mistake of the intellect’ (Pragyāparādha, Shārīrasthāna, I.109). To rectify disease, three therapy types have been identified by Charaka: spiritual; rational; and psychological (Sūtrasthāna, I.54).
Ayurvedic theory declares: a change in one part of the body causes a change in a corresponding part of the body, a theory which is fundamental to our conception of ‘association’ in this research. The notion of ‘change’ in this context refers to both a) an influence of balance, harmony, and the body’s restorative nature, which leads to good health, and b) the vitiation (i.e., elevation or diminution) of one aspect of the body, which correspondingly causes imbalance somewhere else in the body, resulting in ill-health.
Thus, according to foundational Ayurvedic theory: Prakriti does not change; changes in Vikriti affect changes in Agni, Koshta, and CVD risk factors; changes in Agni create equilibrium in Vikriti and affect changes in Koshta and CVD risk factors; changes in Koshta affect changes in CVD risk factors; and changes in all of them affect changes in a person’s overall short- and long-term health. These collective changes are caused by internal and/or external stimuli, such as those caused by changes in diet (internal) or changes in the weather or season (external), which impact the current state of one’s mind and body (Vikriti). This phenomenon is schematically represented in the conceptual model shown in Figure 1.

Figure 1 Conceptual model of the relationships between Prakriti, Vikriti, Agni, Koshta, CVD risk factors, and health.
To test the proposition of reciprocal change of the types described above where the vitiation of a Dosha in Vikriti can cause a vitiation in Agni, for example, preliminary research conducted by these authors suggests there are significant associations between Vikriti, Agni, Koshta, and CVD risk factors8 and that changes in one parameter predict, albeit weakly in some cases, changes in another according to Ayurvedic theory.
In our study of 160 Ayurvedic patients, the vitiation of Vāta was correlated to Vishamāgni (φ = .31, p = .00007) and to Krūra Koshta (φ = .80, p < .00001). Results uniformly indicated that the vitiation of Vāta was also inversely associated with weight (rpb = ‒.40, p = .00001), BMI (rpb = ‒.40, p = .00001), and diet (φ = ‒.25, p = .001), but not BP (rpb = ‒.12, p = NS); Vishamāgni was associated with lower weight (rpb = ‒.32, p = .00004), lower BMI (rpb = ‒.33, p = .00001), and diet (φ = ‒.16, p = .03), but not BP (rpb = 0.0, p = NS); and Krūra Koshta was also associated with lower weight (rpb = ‒.36, p = .00001), lower BMI (rpb = ‒.40, p = .00001), and diet (φ = ‒.29, p = .0001), but again not with BP (rpb = 0.0, p = NS). Similar results were observed for patient’s diagnosed with vitiated Pitta and Kapha and their respective Agnis and Koshtas. Earlier descriptive findings on the same topic have suggested similar associations.14
Findings from the Fergusson, Palakurthi and Dornala study thereby support Ayurvedic theory and clinical practice passed down from Charaka Saṁhitā and Sushruta Saṁhitā to contemporary doctors (or Vaidyas), i.e., that a patient’s vitiated Vikriti is related to the quality of their digestion and gut responsiveness, and that the Doshas, as expressed in the current state of a patient’s Agni and Koshta, relate to some CVD risk factors.
The overall structure of the conceptual model can thereby be represented as four possible parallel phenomena in the body as shown in Figure 2. These four phenomena are: vitiated Vāta in Vikriti leading to Vishamāgni and then Krūra Koshta; vitiated Pitta in Vikriti leading to Tīkshnāgni and then Mrīdu Koshta; vitiated Kapha in Vikriti leading to Mandāgni and then Madhyama Koshta; and non-vitiated Vikriti, Agni, and Koshta. For the purposes of brevity, in this study only the first of these four phenomena—i.e., the one associated with the vitiation of Vāta in Vikriti, Agni, and Koshta (first column in Figure 2)—will be examined.
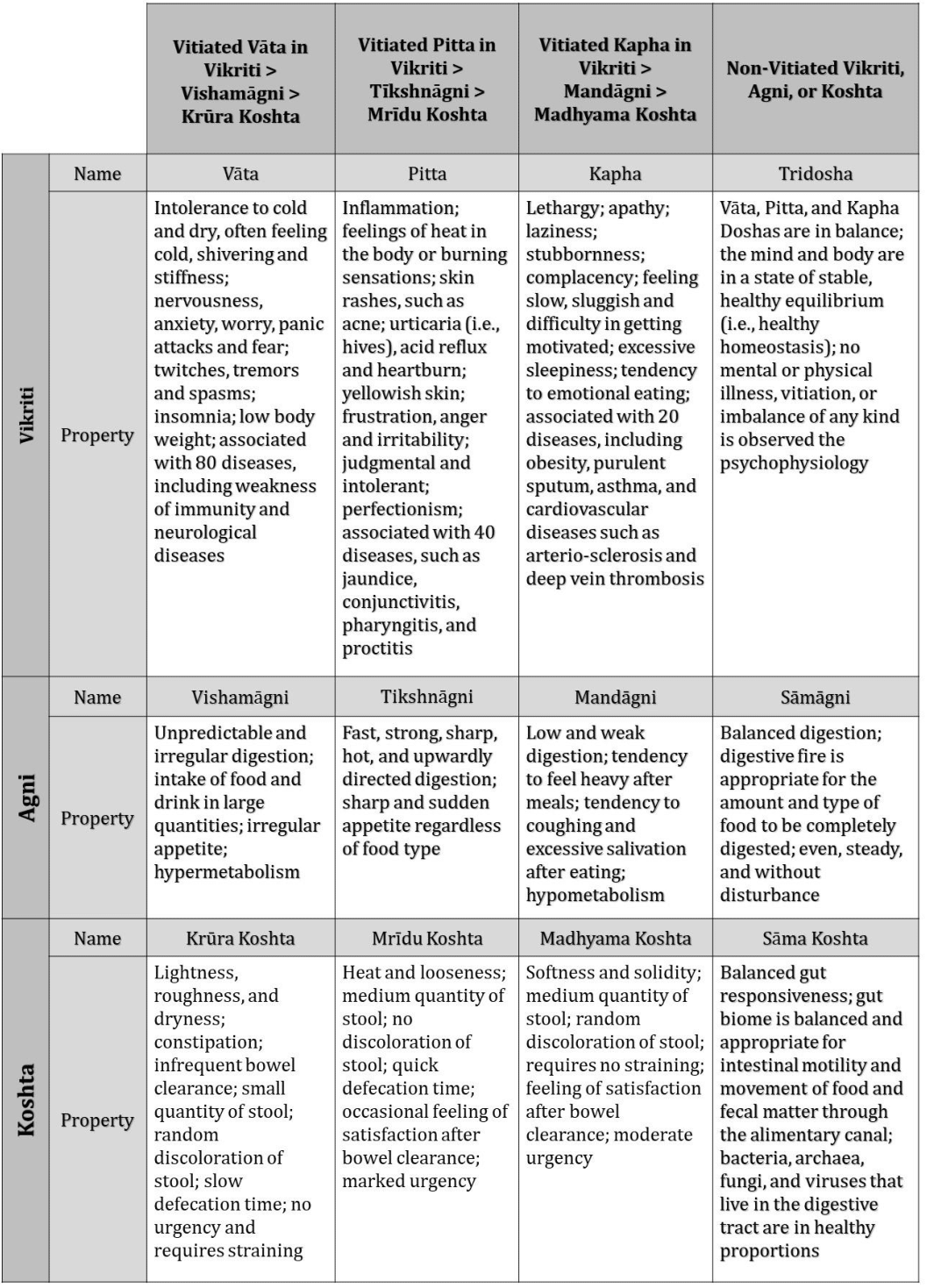
Figure 2 Associations between vitiated and non-vitiated Vāta, Pitta, or Kapha in Vikriti, Agni, and Koshta and examples of their psychophysiological properties.
Vitiated Vāta in Vikriti
According to Ashtānga Hṙidayam, symptoms of vitiated Vāta in Vikriti include emaciation (Kārshya), black or dark coloration (Kārshṇya), desire for heat (Ushṇakāmatv), shaking or tremors (Kamp), constipation (Anāh), abdominal distension (Shakribrahān), loss of strength and immunity (Bal-bhraṁsh), loss of sleep (Nidrā-bhraṁsh), loss of sensory perception (Indriya-bhraṁsh), irrelevant speech (Pralāp), and timidity (Dīna) (Sūtrasthāna, XI.6). Clinically, these symptoms translate into an intolerance for cold and windy and dry weather, cold hands and feet, impulsiveness, a tendency to overcommit to activity, a tendency to insomnia, quick to forget things, restlessness, a tendency to worry and anxiousness, and stiff muscles and joints.
Vitiated Vāta in Agni
According to Mādhav Nidān Saṁhitā (VI.5, 10–12, 24), “feeling weak or tired (without physical exertion), heaviness of the body, feeling of obstruction in the abdomen, giddiness, improper movement of Vāta, constipation or diarrhea are the general symptoms of Ajīrṇ (i.e., indigestion). Āma, Vidagdh, and Vistabdh are the three kinds of Ajīrṇ caused by Kapha, Pitta, and Vāta, respectively…. The symptoms of Vistabdh Ajīrṇ are abdominal pain, tympanites (swelling of the abdomen due to gas), Vāta type of pain, retention of stool and flatus, ignorance and pain of the limbs and various parts of the body”. In Ayurveda, four main digestion types are possible: Vishamāgni; Tīkshnāgni; Mandāgni; and Sāmāgni.
Vishamāgni represents unpredictable and irregular digestion. In this condition, a person can alternately feel satiated after eating a meal, with a feeling of being well nourished and satisfied, but at other times, can feel bloated, heavy, lethargic, and uncomfortable. Vishamāgni is associated with vitiated Vāta because, like the wind, it can be erratic and causes symptoms such as bloat and gas, rumbling in the abdomen, often accompanied by constipation or alternate periods of constipation and loose stool. Symptoms of digestion related to vitiated Vāta in Agni include unpredictable appetite, irregular and unpredictable digestion, after a meal sometimes feeling satiated but at other times feels bloated, gaseous, heavy, lethargic, and uncomfortable, with rumblings in the abdomen, and a sensitivity to many food types.
Vitiated Vāta in Koshta
The status of each patient’s gut responsiveness is determined by various diagnostic techniques. According to Divyashree et al.,21 “Koshta refers to the state of the abdomen or alimentary tract and is usually determined by the behaviour of the bowel habits”; according to Ragad & Gokhale et al.,22 it is “the space or hollowness of the body for accommodation of organs including stomach, liver, spleen, pancreas, intestine, etc. and pelvic cavity for accommodation of uterus, urinary bladder, and lower part of bowel”.
Ayurveda identifies four main types of gut responsiveness: Krūra Koshta; Mṛidu Koshta; Madhyama Koshta; and Sāma Koshta. When the qualities of Krūra, Mṛidu, and Madhyama Koshta are in equal proportion and when no one Dosha is vitiated in the gut, one is said to experience Sāma Koshta. Divyashree et al.21 maintain that one’s Koshta varies according to one’s Prakriti and Vikriti: Krūra Koshta relates to Vāta-vitiated Vikriti, Mṛidu Koshta relates to Pitta-vitiated Vikriti, and Madhyama Koshta relates to Kapha-vitiated Vikriti.
Krūra Koshta thus occurs when Vāta is dominant in the alimentary canal, which decreases the liquid content of the stool and results in elimination of hard stools; Krūra Koshta therefore causes difficulty in elimination. The Laghu (lightness) and Ruksha (dryness) qualities of Vāta reduce softness, stickiness, and oiliness of the stool, however these qualities are required in harmony with others for proper elimination, thereby preventing loose stools; in Krūra Koshta the qualities of lightness and dryness are elevated.
The purpose of this pilot study is to reevaluate the associations between Vikriti and Agni using a mathematical model to uncover underlying mechanisms. It is important to point out that the authors appreciate Ayurveda is not merely about the body, but is an alternative, but complete, medical science concerned with every aspect of human life—consciousness, mind, body, behaviour, society, and the environment. However, for the purposes of this research we have chosen to limit our investigation to a few core aspects of the body and their relations, and even then only in one stream of associations related to Vāta can be modelled in any detail. In doing so we do not mean to trivialize or understate the importance of modelling Pitta and Kapha or indeed other aspects of life.
Diagnosis of Prakriti, Vikriti, Agni, and Koshta
In Ayurveda, three main forms of diagnosis are recognised: Darshana (observing); Sparshana (touching); and Prashna (inquiring). Darshana relates to the observation of a patient’s gait, stance, and posture, colour of hair and eyes, colour and features of the tongue, facial expressions and voice, enlarged or shrunken parts of the body, among other observations.
Sparshana, sometimes referred to as the ‘palpation method’ typically preceded by Darshana, means the tactile sense of touch, and can include assessing body temperature, but most commonly involves feeling the skin for roughness, dryness, heat or cold, moisture, and so on. Sparshana can include any of the following diagnostic techniques: touching the eyeballs to assess intraocular pressure; testing reflexes; examination of swelling and rigidity of organs; palpation of glands and tumors (in Ayurveda called Gulmalgranthi); and palpation and percussion of fluid retention (ascitis qalodara).
Sparshana includes Nādi-Vigyān.23 According to Shārngadhar Saṁhitā, “the artery pulsating at the base of the thumb indicates life. Happiness and misery, including balanced and imbalanced states of the physiology, should be known from its [i.e., the pulse’s] movements” (Pūrva Khaṇda, 3.1). Khajuria et al.24 point out that “each cell in our body possesses its own intelligence. It is the communication of this intelligence in the form of vibrations that is studied in Nādi-Vigyān. Nādi-Vigyān understands the vibratory frequency of the pulse at various levels on the radial artery”. These vibrations of Vāta, Pitta, and Kapha are felt by the practitioner on the left wrist of a sitting female and right wrist of a sitting male.25
Prashna means inquiry or questioning, such as asking how the patient feels, what symptoms they are experiencing, how have their diseases progressed, whether they are sleeping well at night, what they eat, how they feel after eating, how much they exercise, their outlook on life, their mental condition, and so on. In the following patient case report, all three diagnostic techniques were applied by Vaidya Dr Manohar Palakurthi, a co-author of this paper.
This patient case report draws from the real-world clinical data of Prakriti, Vikriti, Agni, Koshta, CVD risk factors, and the health status of a patient and will serve as the data source for mathematical modelling. The report includes initial patient diagnosis, prognosis, recommendations, and follow-up diagnosis at six-months. Data were collected from a patient attending an Ayurvedic clinic in the U.S. Midwest during an initial consultation in early 2022 and then repeated after six months during a follow-up consultation. Data collection involved the following two-step process.
In Step 1, two measures of the patient were taken by a qualified nurse: a) height and weight were recorded; and b) BP using a manual sphygmomanometer. Based on a), the patient’s BMI was calculated using the following standard formula: kg/m2, where kg is the patient’s weight in kilograms and m2 is their height in metres squared. BMI was recorded according to the following classification: <18.5kg/m2 (underweight); 18.5‒25kg/m2 (normal weight); 25‒30kg/m2 (overweight); and >30kg/m2 (obese). Based on b), BP was rated as: 130/80mmg= normal; 130‒139/80‒89 mmg=elevated; 140‒159/90‒99mmg=Grade 1 hypertension; and 160‒179/100‒109 mmg= Grade 2 hypertension. These hypertension criteria were determined using guidelines provided by Unger et al.26
In Step 2 Vaidya Manohar diagnosed the patient’s Prakriti, Vikriti, Agni, and Koshta, employing each of the three main types of Ayurvedic diagnostic technique listed above.
Initial consultation
‘PD’ (not her real initials) was a 44-year-old female, non-vegetarian patient. At her initial consultation, PD’s height was 1.60 m (5’3”), weight was 45.2kg (99.6lbs), and BMI was 17.6 kg/m2. PD’s BP was an elevated 135/81 mmg. PD reported infrequent pain in the abdomen after eating (even when consuming small amounts of food), periodic feelings of dullness and sluggishness after eating, a problem which has come and gone throughout her adult life, and generally comfortable bowel movements, but with a tendency toward dryness. PD reported her diet was rich in meat (mostly chicken and fish) and most vegetables; she also liked regularly eating raw foods, such as salads and nuts. PD reported what were likely symptoms associated with rheumatoid arthritis (mild pain in the mid-back and right hand) and irregular menstrual flow and pain, the two main purposes of her visit to the clinic.
Prakriti: The following were noted by Dr Manohar: PD was thin and had a light physique (she confirmed that while her adult weight fluctuated, it had always been “around 100 lbs”); she was quick moving; had narrow shoulders and hips, and chiselled facial features; her veins could be easily seen under the skin; she had rough, dry skin, and was cold to the touch; her hair was fine, dry, and brittle, all indications of Vāta constitution.
Vikriti: The following were also noted: PD had a tendency to worry and anxiousness; she reported that her sleep was somewhat fitful and light, and she would sometimes awaken feeling as if she had not slept well (although this sensation was random and not persistent); she was less inclined to tolerate cold rather than heat, and also less tolerant of windy and dry weather; she had cold hands and feet at presentation; she reported “I have a feeling of stiff muscles and joints” but did little exercise; she appeared somewhat restless, with some tapping of hands and feet during consultation; as a result of Prashna, PD reported a slightly impulsive nature, a tendency to overcommit to activity, and a tendency to insomnia; she reported a general tendency to quickly forgetting things, and said she sometimes felt “flighty” and “ungrounded”.
Agni: The following were also noted: PD reported an unpredictable appetite; irregular and unpredictable digestion; after eating, she sometimes felt satiated but at other times felt bloated, gaseous, heavy, lethargic, and uncomfortable, with frequent “rumblings in the abdomen”; she reported a sensitivity to many food types.
Koshta: The following were also noted: PD reported mild, but somewhat increasingly frequent, constipation (i.e., a tendency to dry and firm stool); constipation alternating with periods of loose stool; minor and infrequent feelings of hemorrhoids during evacuation (for a complete description of hemorrhoids—in Ayurveda called, Arśa—and their cause by vitiated Vāta, see Charaka Saṁhitā, Chikitsāsthānam, XIV); and infrequent pain in the abdomen, but not always associated with eating and irrespective of volume and type of food consumed; PD described her bowel movements as “erratic” and sometimes “painful”.
The following represents a summary of PD’s consultation. Due to unfavorable behavior (e.g., suppression of natural urges), inconsistent daily routine (e.g., lack of regular light exercise) and seasonal routine (e.g., prolonged exposure to cold weather), and a diet of Vāta-inducing food, qualities of Vāta were elevated in the body, with increased coldness, dryness, roughness, instability, and movement throughout the body resulting in feelings of cold and stiffness, along with a tendency to nervousness, worry, and sleeplessness. PD was underweight, had low BMI and elevated hypertension, and was suffering from back and hand pain.
PD was thus diagnosed as: Prakriti= Vāta-Pitta; Vikriti=vitiated (i.e., elevated) Vāta; Agni=Vishamāgni; Koshta=Krūra Koshta; imbalance of Vāta Dosha is the likely cause of back, and particularly, hand pain, and this pain may indicate the early onset of rheumatoid arthritis. (For a more detailed description and explanation of Vāta Dosha, its vitiation and adverse influence on Agni, Koshta, rheumatoid arthritis or Āmavāta, and health, see Charaka Saṁhitā, Sūtrasthāna, XII, and Chintala & Bhagavathi et al.13 Figure 3 applies these patient data to the conceptual model of Figure 1.
Prognosis
Unless elevated levels of Vāta are reduced, PD will suffer further from back, hand, and menstrual pain, feelings of bloatedness after eating, and constipation, and may develop rheumatoid arthritis. Vitiated Vāta is associated with various diseases and affects strength, skin, stamina, and shortened lifespan; it aggravates the mind and can cause fear, anxiety, bewilderment, and delirium.
Recommendations
The immediate focus of PD’s treatment was on the reduction of Vāta through a combination of: A) Vāta-pacifying diet; B) Vāta-pacifying daily routine (Dinacharya); C) Vāta-pacifying seasonal routine (Ritucharya); D) various Vāta-pacifying herbal supplements (Rasāyanas); and E) daily massage with Vāta-mitigating herbalised oil (Abhyanga). The importance of A) alone is highlighted by Charaka Saṁhitā, which states: “There are six Rasas (or tastes of food): sweet, sour, salty, pungent, bitter, and astringent. When used properly, the body is maintained in a healthy state; their incorrect use results in vitiation of the Doshas” (Vimānasthān, 1.4). Specific recommendations to reduce the influence of vitiated Vāta were:
Follow-up consultation
PD returned to the clinic for a follow-up consultation after six-months of Ayurvedic treatment and reported she had followed the recommendations closely during that time. Furthermore, PD reported that her initial feelings of improvement were slow for several months but improved rapidly after three or four months. At follow-up, PD was diagnosed as: Vikriti=reduced vitiation of Vāta; Agni=improved digestion, with regular appetite and no feelings of bloatedness, i.e., a return to Sāmāgni; Koshta=improved gut responsiveness and little or no constipation, i.e., a return to Sāmā Koshta; weight= 48.9kg, i.e., increased to within the ‘normal’ weight range; BMI= 18.9km/m2, i.e., increased to within the ‘normal’ range; and hypertension= 125/74mmg, i.e., reduced to within the ‘normal’ range.
We first summarize the doctor’s assessment of the patient during the treatment period. We next formulate our theoretical framework and working hypothesis. We then use them to construct our mathematical model (Figure 4).
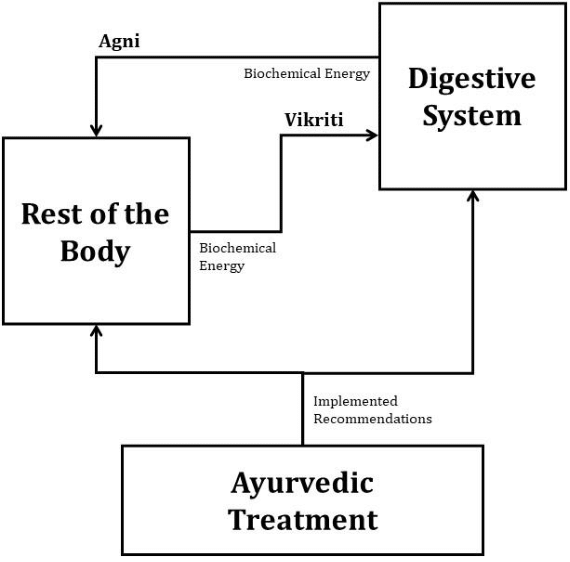
Figure 4 Conceptual model of the relationships between digestive system, the rest of the body, and the Ayurvedic treatment.
Doctor’s assessment of the patient during the six-months process of the Ayurvedic treatment.
2.1. Diagnosis and its interpretation
2.1.1. Agni: significantly vitiated by Vāta (Vishamāgni)=1 (i.e., low level of biochemical energy); and
2.1.2. Vikriti: significantly vitiated by Vāta=1 (i.e., low level of biochemical energy).
2.2. Recommendations to reduce the levels of Vāta in the body:
2.2.1. Follow a special diet, daily routine, balanced seasonal routine; and
2.2.2. Take special herbal supplements.
3.1. Diagnosis and its interpretation
3.1.1. Agni: improved digestion, with no vitiation of Vāta= 3 (i.e., high level of biochemical energy); and
3.1.2. Vikriti: reduced vitiated Vāta= 3 (i.e., high level of biochemical energy).
Theoretical framework
Remark
Advantages of the framework:
Limitations of the framework:
Mathematical model
Our working hypothesis allows the formulation of a mathematical model of two elements of the Ayurveda treatment process (see Figure 4):
A threshold phenomenon is an example of a biological switch. These are, typically, associated with bistability and, often with a hysteresis mechanism, are well understood and ubiquitous in biological and science problems. The examples include: in system biology,2 modelling nonlinear effects in mitochondrial respiratoration and in phenotypic changes,27 dementia,28 and depression.29
We model the threshold via the hysteresis singularity.30 This is the situation where a sharp change in the output occurs when an accumulation of a continuous change in an input reaches a critical point. We use a standard modelling approach in mathematical biology.31,32 The interaction between the digestive system and the rest of the body is modelled mathematically by a system of two coupled, first order, parametrised, nonlinear ordinary differential equations (ODEs):
The equilibrium equations are:
Here:
are constants;
x is Agni, the biochemical energy produced by the digestive system;
y is Vikriti, the biochemical energy in the rest of the body;
u is a parameter that accounts for the combined external influences on the body, listed above in Recommendations for the patient case report;
-a1x is the rate of loss or expenditure of Agni;
-a2y is the rate of loss or expenditure of Vikriti;
is the positive feedback of Agni from the digestive system to the rest of the body, which accounts for the threshold phenomenon described in Charaka Saṁhitā and by the personal experiences of the patient;
cu and (1-c)u are fractions of the combined external influences u on Agni and on Vikriti, correspondingly; and
00 is the first point on the curve; 99 is the last point on the curve.
We assume that during the Ayurvedic treatment process, the patient’s organism was in a homeostatic state (i.e., a stable solution of the equilibrium equations above) interrupted only by a single jump, as shown in the bifurcation diagrams in Figures 5–7.
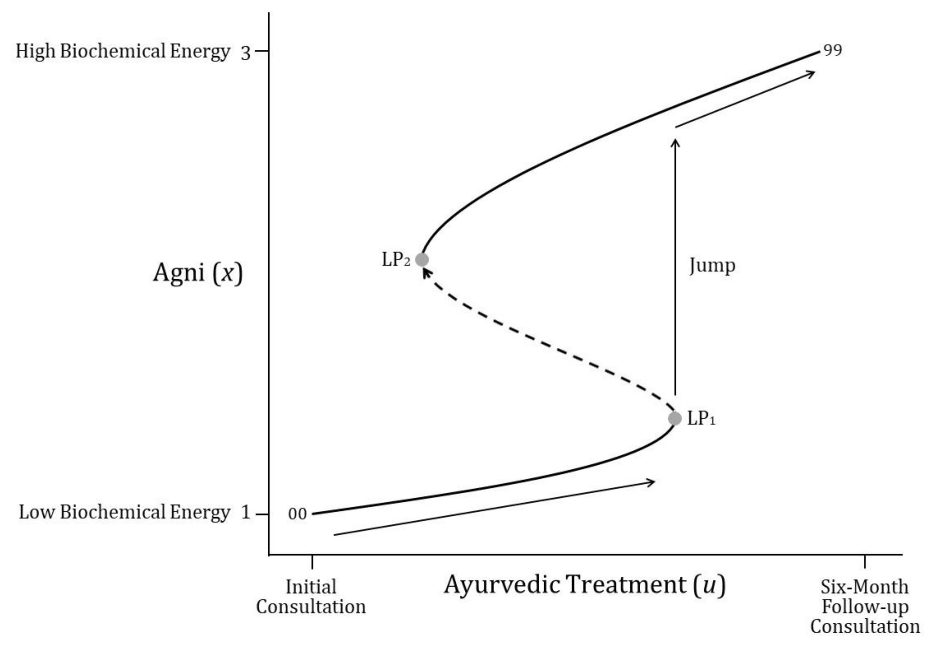
Figure 5 Increase of Agni (x) (improvement of health of the digestive system) with Ayurvedic treatment (u).
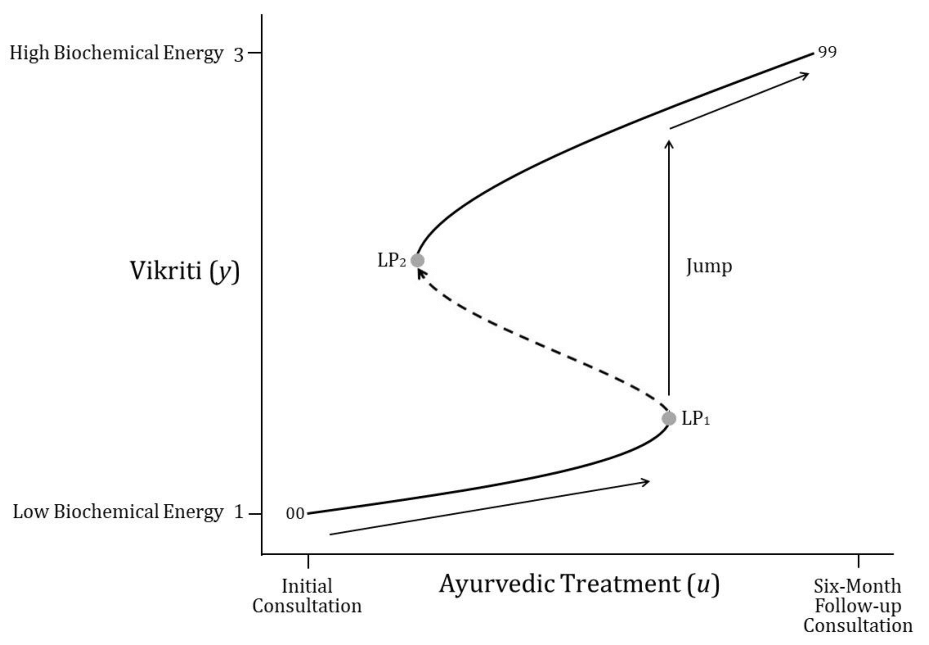
Figure 6 Increase of Vikriti (y) (improvement of health of the rest of the body) with Ayurvedic treatment (u). with Ayurvedic treatment (u).
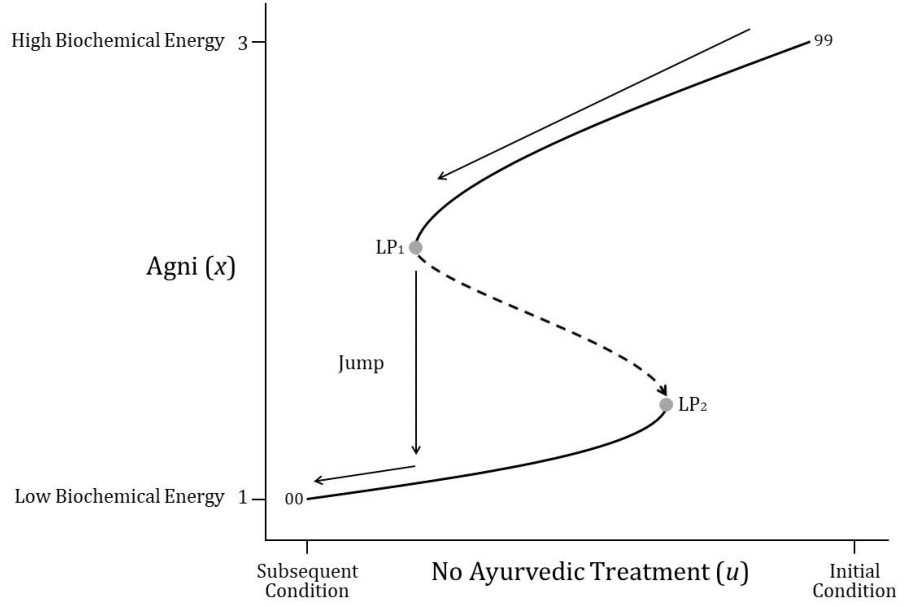
Figure 7 Decline of initial, healthy condition of Agni (x), assuming an unhealthy (u) lifestyle, to a less healthy condition of digestion.
We perform numerical continuation of solutions to the equilibrium equations by the numerical continuation and bifurcation software Cl matcontL (developed by the second author and his collaborators Bindel et al.,33). This includes location of bifurcation limit points LP1 and LP2, which produce the bifurcation diagrams in Figures 5–7. In particular, in Figures 5 & 6, for Agni and Vikriti, correspondingly, low biochemical energy is associated with reduced health and increased vitiation (1), whereas high biochemical energy is associated with improved health and reduced vitiation (3).
Note, in mathematical terminology, this curve is a bifurcation diagram, where LP1 and LP2 are limit points, the upper and lower segments of the curve are stable, and the middle one is unstable.
When, at some stage in the treatment process, Agni crosses the threshold point LP1, a sharp transition or a ‘jump’ in the health status of the patient occurs: his digestive system switches from a persistent irregular unhealthy digestion (Vishamāgni) to a persistent, balanced and healthy one. And thereafter, beyond LP1, Agni continues to increase and the digestive system continues to improve on the new path until the time of the follow-up consultation.
This notion of a ‘jump’ in health status, as a result of Ayurvedic treatment, is particularly relevant in the case of vitiated Agni due to excessive levels of Vāta Dosha, as was the case with the patient, because the properties of Vāta are said by Charaka to “quickly arise and quickly subside” (Sūtrasthāna, XVIII.7); elsewhere, Charaka speaks about treatment impacts related more generally to “saturation” as “instant” or “prolonged” phenomena (Sūtrasthāna, XXIV, 26-30). The cause of this jump may be one or a combination of accumulated treatment effects reaching their critical contribution to balancing the digestive system.
The pattern of improvement of Vikriti (y), see Figure 6, is analogous to that of Agni. Interestingly, according to our model, a reverse hysteresis pehomenon is also true, namely, dependence of Agni and Vikriti on their history applies in this case too. If a patient is healthy but adopts an unhealthy lifestyle for some reason, starting at the point 99, then ill-health would occur with the vitiation of Doshas, with a delay, according to the following pathway shown in Figure 7. Thus, the patient’s health would slowly deteriorate until it reaches a limit point (LP2), where it jumps, or rapidly declines, and then continues to slowly decline to point 00 on the lower curve.
We have constructed a minimal phenomenological nonlinear dynamics model to account for some elements of interaction between Agni and Vikriti in a six-month Ayurvedic treatment case.
Background of our model
Our starting point was the conceptual model presented in Figure 1. This model was informed by traditional Ayurvedic theory of Prakriti, Vikriti, Agni, and Koshta as animated by the three Doshas. The theory is predicated on two fundamental concepts of health: a) when the aggravated presence of a Dosha vitiates the psychophysiology of an individual, as expressed and observed in Vikriti, such vitiation of properties then also adversely affects Agni and Koshta, potentially leading to increased CVD risk factors and ultimately ill-health; and b) both adverse, as well as salutary, changes in one aspect of the physiology cause a parallel and commensurate change in another related aspect of the physiology. Our earlier research8 found suggestive evidence of this effect. Here, our predictive mathematical model provides a hypothetical mechanism by which this effect may actually be causative.
The challenges
Our principal challenge: no formal definitions of Agni and Vikriti and no information about the nature of the interaction between them, required for our mathematical model, are available.
Addressing challenges
As a working hypothesis, we have constructed a minimal phenomenological conceptual framework using the raw data from the patient case report, including the doctor’s evaluation of these data and certain qualitative descriptions of Agni and Vikriti.
Results
Our predictive mathematical model accounts for two important empirical and theoretical results:
There is not yet a scientific explanation of the fundamental mechanisms underlying many successes of Ayurvedic treatments. The results of our modelling also lead to a conjecture that, in the human organism, there exist high-level regulating/control mechanisms, and the Ayurveda protocols take advantage of them.
To the best of our knowledge, the present paper formulates the first, though minimal but rigorous, mathematical model of mechanisms behind the protocols used by an Ayurvedic doctor, including the diagnostic (no devices) methods and non-invasive (no drugs) treatment protocols. Our rigorous modelling may stimulate the formulation of testable hypotheses. Further developing and extending research in this direction has a potential to bring significant benefits to a larger group of cardiovascular patients.
From the clinical perspective, a deep understanding of the mechanism of vitiation of the Doshas is of paramount importance, hence the proposed next step is to investigate this mechanism, specifically, to account for the positive results produced by the Ayurvedic treatment protocol described in our paper using suitable physiological concepts and markers to first develop a theoretical model and then a predictive mathematical one.
An attempt at modelling the relevant Ayurvedic elements, properties, and processes would be a natural extension of the approach in this research. It might become a longer-term research endeavour in which mathematical modelling could be used as a useful research tool to uncover and articulate underlying psychophysiological mechanisms.
None.
The authors declare that they have no conflicts of interest.
None.

©2023 Fergusson, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.