International Journal of
eISSN: 2381-1803


Research Article Volume 13 Issue 1
1Integrated Center of Traditional Chinese Medicine, Sorbonne Université, France
2Avenue de la Division Lecler, France
Correspondence: Alain Baumelou, Integrated Center of Traditional Chinese Medicine, GHU Pitié-Salpêtrière and Sorbonne Université, 47-83 boulevard de l'Hôpital, 75651, Paris Cedex 13, France
Received: February 04, 2020 | Published: February 17, 2020
Citation: Y-Nhi D, Carole S, Bingkai L, et al. Self-administered phyto-acupressure for tension-type headache. Int J Complement Alt Med. 2020;13(1):42-46. DOI: 10.15406/ijcam.2020.13.00491
Objectives: The effect of phyto-acupressure (PAP) on chronic tension-type headache was investigated in this prospective pragmatic study. PAP is traditionally used in Asian medicine.
Methods: This open intra-individual study was conducted during three periods of four weeks each: first as baseline with usual treatment, second PAP treatment on top usual treatment and third free choice of the patient. 31 voluntary patients (20 women and 11 men) with frequent episodic and chronic tension-type headache (6 to 15 per month) self-administered massage therapy on acupuncture points with the local application of a concentrated plant formula. Headache frequency, intensity, duration, and analgesic use were recorded and compared with baseline values.
Results: Compared with baseline values, the average number of headache episodes was significantly reduced during the PAP period from 13.06+-6.7 to 10.9+-5.5. The reduction of headache episodes continued for the remainder of the study (p= 0.01). At the end of the trial, when patients had a free choice of treatment, average headache number was 7.17+-4.86 and for 87% of headaches the patients opt for PAP alone. Concerning intensity and duration, the effect of PAP was on the same magnitude as paracetamol on-demand. The intake of paracetamol was sharply reduced by phyto-acupressure.
Conclusions: The phyto-acupressure therapy used in this study seems to go beyond the treatment of pain. In addition to have an analgesic effect measured by reduction in analgesic use, PAP also has a prophylactic action in reducing headache frequency. A randomized controlled trial is needed as a next step.
Keywords: tension-type headache, acupressure, phyto-acupressure, patient satisfaction, traditional Chinese medicine, oriental medicine, complementary medicine, integrative medicine, herbal medicine
PAP, phyto-acupressure; TTH, treatment of tension-type headache; CHQQ, comprehensive headache-related quality of life questionnaire
The Eurolight project found a 91.3% lifetime prevalence of headache in its general European population samples and an estimated 78.6% prevalence for any type of headache each year.1 In parallel, alternative and complementary therapy use for the treatment of tension-type headache (TTH) has been developing. This can be explained as being due to both the lack of appropriate conventional medical treatments and the presence of various contraindications and side-effects indicated in repeated analgesic use. Traditional Asian Medicine represents a therapeutic option in this domain that is increasingly being studied.2 Following these studies, we have developed a phyto-acupressure device, Ylo PAP, which is both a specific and a natural topical treatment for tension headache. Phyto-acupressure (PAP) is the synergy of phytotherapy and acupressure. The empirical basis of acupressure is shared with that of acupuncture. Acupressure involves the activation of specific acupuncture points. Acupressure however, is non-invasive and does not require the use of needles. It can also be self-administered by patients since the treatment areas are larger than those used in acupuncture. Ylo PAP is in the form of a pen containing a concentrated plant formula (Angelica dahurica, Cnidium officinalis, Chrysanthemum indicum) that is administered with a roll-on applicator (Figure 1). The added value of the Ylo PAP device is its rounded stainless-steel tip which is used to activate the acupoints through localized self-massage.
The purpose of this study was to evaluate the analgesic efficacy, the impact on the frequency of tension headache, the reduction in analgesic medication use generated, and the cutaneous tolerance following the use of the Ylo device for the treatment of tension-type headache.
Participants
This open intra-individual pilot study was conducted with 31 voluntary patients (20 women and 11 men), with a mean age of 31+/- 1 year (Table 1). The primary selection criterion for inclusion in the trial was a frequency of tension headache ranging from 6 to 15 episodes per month with the potential of necessitating analgesic use (paracetamol or ibuprofen). There was no comorbidity present among the volunteers and participants were asked to carefully follow the initial instructions given by a clinician trainer. Patients suffering from migraines were excluded from the sample population.
Number of patients |
31 |
Mean age (y) |
31+/- 1 |
Number of headaches per patient |
13,06+/- 6,7 |
Maximum headache intensity |
5,25+/-1,5 |
Average headache duration (min) |
452,9+/- 280 |
Total amount of paracetamol consumed in period 1(g) |
18,9 |
Table 1 Demographic data in first 28days of observation (period 1)
|
Period 1 |
Period 2 |
Period 3 |
Total number of headaches |
223 |
279 |
215 |
Maximum headache intensity |
5,25 |
5,29(NS) |
5,32(NS) |
% of headaches relieved |
80% |
83% |
87% |
Mean relief score per participant |
6,52 |
6,43(NS) |
6,19(NS) |
Average duration of headache (min) |
566.97+/- 30 |
669min(NS) |
532min(NS) |
Table 2 Analgesic efficacy by treatment ° in the group of patients with free choice
|
Period 1 |
Period 2 |
Number of headaches |
405 |
338 |
Number of headaches treated by phyto-acupressure alone |
0(0%) |
279(82,5%) |
Number of headaches treated by both phyto-acupressure and paracetamol |
0(0%) |
45(13,3%) |
Number of headaches treated by paracetamol alone |
223(55%) |
4(1,2%)* |
Total amount of paracetamol per period (g) |
18,9 |
4,2 |
Average dose of paracetamol taken per headache (mg) |
895 |
920 |
Table 3 Paracetamol consumption parameters *Protocol deviations.
Interventions
This study involved three 28-day periods. Period 1 was an observation phase (Table 1) during which the participants provided information on each of their headache episodes and used their routine treatments as needed. In Period 2, subjects used the Ylo PAP device to relieve their headache, beginning from the first appearance of symptoms and continuing as often as necessary. During Period 3, the participants were given the choice of continuing their use of Ylo PAP or of returning to their routine treatment to relieve their headaches. During all three periods, participants self-reported by responding to a questionnaire and keeping a journal on a daily basis.
Ylo PAP device (Figure 2) is in the form of a pen with two rounded ends made of stainless steel. The patient inserts a recharge cartridge with a roll-on applicator containing the concentrated plant formula into the pen. The use of the Ylo PAP device involves three steps. The identification of the specific acupressure treatment areas that correspond both to the location of the headache (top of the head, back of the head, forehead, temples, entire head etc..,) (Annex 1) and to the presence or absence of nausea. The plant extract formula is then applied to the treatment areas using the roll-on applicator. Plants used in the formula are traditionally used in Asian medicine: Angelica dahurica root extract, Cnidium officinalis root extract, and Chrysantemum indicum extract. Acupressure then activates the treatment areas by applying pressure with the rounded surgical stainless steel ends of the phyto-acupression pen. Treatment areas are identified with the aid of an application for smartphones or with diagrams in a paper information booklet. The acupuncture points used are described in Annex 1.
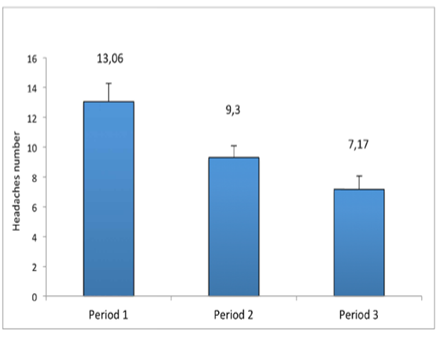
Figure 2 In the patients related with YIo device, there is significant decrease of headaches number in phase 2 versus phase 3 versus (P-value <0.0001).
Outcome measures
Participants kept a daily record of their headache occurrences including details on headache intensity; the medications taken; their self-evaluation of the relief gained through treatment (positive or negative response). Their sensation of relief was expressed on a numerical scale from 1 to 10 (1 for no relief, 10 for total relief); the time, in minutes, needed to feel relief; and the total duration of the headache episode in minutes. The intensity of a headache episode was defined as the maximum value of pain experienced and self-evaluated on a numerical scale from 1 to 10 (1 for small intensity, 10 for maximal).
All headache episodes were recorded in the participant’s journal notebook. The mean number of headaches experienced by each participant was calculated for each of the three study periods. During the baseline period 55% of headaches were treated by paracetamol. In the first two periods, medication use and dosage were also included in the journal notebook. The total amount per period and the average dosages taken were calculated for the total number of headache episodes.
During the study a dermatologist examined the application areas at D0; D28; D56 and D84. The following criteria were evaluated using a scale with 5 degrees ranging from none to severe: erythema; edema; dryness; flaking; and roughness. Study participants also used a 0 to 5 scale in order to report on the presence and severity or absence of: skin tightness; tingling; itchiness; and burning sensations on or around the application zone. Cutaneous tolerance was evaluated on the basis of the participants’ self-reporting data in conjunction with the results of their dermatological examinations. Adverse signs were considered as pertinent when they could be directly, plausibly, or potentially ascribed to the use of the phytotherapy product and/or when such signs persisted. Adverse signs were also considered as pertinent when they occurred during the third period of the study when participants could freely use the Ylo device without oversight.
At the end of the study, participants provided feedback on their degree of satisfaction with the phyto-acupressure device including information on its practicality.
Statistical analysis
Statistical analysis of the results was conducted using the Student’s t-test or the Wilcoxon test in the case of non-normal distribution. Results were considered to be statistically significant if p<0.05.
Headaches frequency
The total number of headaches is drastically decreased during the trial: 405 in the first period, 338 in the second where all the patients use exclusively PAP device and 271 in the third where the choice is free. The sole use without analgesic consumption of the Ylo PAP device decrease the frequency per patient from 13.06+-6.7 in period 1 to 9.30+-4.3 in period 2 (p<0.01) and 7.17+-4.9 in period 3 (p<0.01) (i.e. -28% in study period 2 and -44% in period 3) (Figure 3).
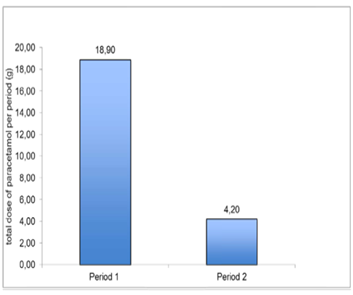
Figure 3 There is significant decrease of paracetamol consumption in phase 2 versus 1(P-value <0.0001).
Headaches severity
The mean maximum headache intensity was comparable for each of the three periods. There was no significant difference in the participants’ average relief scores or in the average duration of the headache episodes for the three periods.
Analgesic consumption
The total dosage of paracetamol consumption was collected during the first two periods of the study. As indicated in figure 3, a strong reduction (-78%) in the use of paracetamol for headache treatment occurred during study periods 1 and 2 (from 18,9g per patient in period1 to 4,2g in period 2 p<0.0001) (Figure 3). The average dose taken per headache remained relatively stable during both periods (Period 1=895mg; Period 2=920mg). According to patient self-reporting, this was because they experienced sufficient-enough relief through their use of the Ylo PAP device and they did not feel the need to take paracetamol as a complement. Only 45 headaches (13.3%) of the participants’ headaches in Period 2 were treated with the use of paracetamol in complement to phyto-acupressure, whereas 83% of their headaches were relieved by the phyto-acupressure device alone.
Treatment adherence
When given free-choice of a treatment option in Period 3, all of the participants choose to continue their use of the phyto-acupressure device. The results of this study indicate that the use of the Ylo PAP device provides a level of headache relief that is similar to that of paracetamol and that this effect is regularly increasing during a 3 months period.
Evaluation of tolerance
No participant displayed adverse clinical symptom during the study. One participant reported benign local signs that were determined to be irrelevant. Under the conditions of this study, the Ylo phyto-acupressure device has a good skin tolerance.
In the adults, headache is the most common form of pain. Over the course of one year 90% of adults experience headache and almost all of them occasionally take analgesics. Tension-type headache is the most common type of headache.3
A recent review suggests that acupuncture, massage, yoga, biofeedback and meditation have positive effects on tension-type headache.4 However, evidence on the efficacy of acupressure and phyto-acupressure remain limited because of few studies published.5 This study explores the effects of phyto-acupressure on 31 patients with chronic tension-type headache. All of the participants included had experienced tension-type headaches for six-months or longer with the occurrence of 6 to 15 episodes per month.
Studies on self-administered acupressure used by healthy subjects indicate that it shows promise for reducing stress among students and for addressing fatigue and sleep disturbance among nurses.5 Self-administered acupressure has also been shown to reduce patient-fatigue associated with breast-cancer treatments.6 Our previous studies have also shown that self-administered phyto-acupressure can reduce sleep disturbances.7 Phyto-acupressure (PAP) is a technique from traditional Asian medicine that combines acupressure with the cutaneous administration of plants. It is closely related to the acupoint herbal patching technique, although PAP involves the topical administration of medicinal plant preparations in conjunction with local point stimulation rather than the use of an herbal medicine patch. The clinical effect of acupressure is believed to be the result of stimulating both meridian and acupuncture points. Plants could be applied on acupuncture points to regulate the body’s functional activity and to strengthen its resistance for the prevention and treatment of illnesses.
This pilot study indicates that the use of the Ylo Headache phyto-acupressure device reduced the frequency of acute TTH attacks. As such, we conclude that PAP can be safely considered as an integrative treatment option for TTH. A similar observation on the efficacy of manual therapy for TTH was made in a meta-analysis including five randomized controlled trials.8 This study found that manual therapy reduced the frequency, intensity, and duration of headache episodes in the short term for individuals with TTH; however, no differences with pharmacological medical care were found on headache intensity in the 24weeks follow-up period.8 In our study, the positive effects of PAP on headache frequency were observed beginning in the first 4 weeks of the study and increasing until the 12th week. Furthermore, the results of this study indicate that PAP had a similar effect to paracetamol on the intensity and the duration of headaches. Our study design, which allowed us to calculate the reduction in paracetamol taken on-demand in the second phase of the study, showed close to a 15g reduction in 4weeks. This is similar to the results given in the 2015 meta-analysis cited here.8 We did not observe any effects on the patients’ quality of life. This can be attributed to this study’s use of the SF-12 (a shortened version of the SF-36), which does not appear to be sensitive-enough to the burden of headache. As such, a quality of life questionnaire that is specific to tension-type headaches, such as the Comprehensive Headache-related Quality of life Questionnaire (CHQQ) should have been used.
The efficacy and patient satisfaction demonstrated in this study can be explained by several factors. The acupressure points used in this study (Annex 1) are all classically defined in traditional Asian medicine. In this sense, the information given to the participants in this study conforms with the Asiatic tradition of selecting both the points to massage and the massage technique used. Furthermore, the plants used in this study are also based on the traditional plants used for headache. These elements make the Ylo PAP device a component of integrative medicine. From the perspective of conventional medicine, this observational pragmatic study shows that the proposed procedure ensures patient satisfaction. While it is difficult to provide a physiopathological explanation for this therapy’s effectiveness on TTH, this difficulty can be attributed, in part, to the diversity of factors that have been linked to the occurrence of TTH episodes. In addition to the intrinsic efficacy of self-massage and/or the administration of plants, diverse elements can also contribute to the patient’s satisfaction with PAP such as: the positive effects of information;10 the importance of individualized care;11 the importance of patient training.12 This reflection highlights the interest of an integrative medicine approach for the care of benign pathologies such as tension-type headache.
The lack of an adequate comparison group constitutes a clear limitation in this study. The methodology used reduced the ability to determine the causality of the procedure. Nevertheless, this pilot study clearly affirms patient satisfaction with the therapy used. Further studies should be conducted in order to investigate the role of each component in the overall effectiveness of this therapy: the administration of plants; acupressure; and the multiple components of the placebo effects involved. Self-administered phytoacupressure is easy and safe; as such it represents important potential as a therapeutic option for patients at pharmacological risk: pregnancy, cancer, patients with hepatic and renal failure, children, and elderly patients.
The phyto-acupressure therapy used in this study seems to go beyond the treatment of pain. In addition to have an analgesic effect measured by reduction in analgesic use, PAP also has a prophylactic action in reducing headache frequency. A randomized controlled trial is needed as a next step.
The authors would especially like to thank Mrs Laurel Mac Ewen for the revision of the manuscript.
Author declares that there are no conflicts on interest.
The research project was partially sponsored by Lutech Society for the Acceleration of Technology Transfer (SATT Lutech) for GHU Pitié Salpêtrière – Sorbonne Université.

©2020 Y-Nhi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.