International Journal of
eISSN: 2381-1803


Case Report Volume 16 Issue 2
Department of Kayachikitsa, R, BAyurvedic Medical College & Hospital, India
Correspondence: Kshama Gupta, Professor, Dept of Kayachikitsa, R B Ayurvedic Medical College & Hospital, Agra, Uttar Pradesh, India
Received: April 04, 2023 | Published: April 13, 2023
Citation: Gupta K, Mamidi P. Ayurvedic management of Immune Thrombocytopenic Purpura - A case report. Int J Complement Alt Med. 2023;16(2):112-117 DOI: 10.15406/ijcam.2023.16.00638
Immune thrombocytopenic purpura (ITP) is a bleeding disorder characterized by isolated thrombocytopenia. The course is more chronic in adults associated with higher mortality in older patients. In extreme cases of ITP, serious complications such as bleeding into the lungs, brain, or other vital organs can occur. Clinical manifestations include purpura, petechiae and ecchymosis. Majority of ITP patients are not getting reliable and durable remissions with modern medicine. The present case report deals with an elderly patient having chronic ITP with multiple comorbidities (obesity, schizophrenia, UTI and T2DM) approached for Ayurvedic treatment. Patient came with ecchymotic patches on both upper extremities with extremely low platelet counts (9700/mcL) was diagnosed as Tiryaggata Raktapitta and Ayurvedic treatment has been provided. Ayurvedic formulations (Putapakwa Vishama Jwarantaka Loha, Raktastambhaka Vati, Samshamani Vati etc) have improved the platelet counts (from the lowest count of 9700/mcL to highest count of 50000/mcL), hematological indices and quality of life in present case. Ecchymotic patches were completely disappeared without any further recurrences. The present case of ITP (Raktapitta) is a good example for Nidaanaarthakara Roga as it has manifested due to the consequences of malarial fever (Vishama Jwara). Ayurvedic treatment seems to be promising in the management of chronic ITP and generates hope for those patients who are having extreme thrombocytopenia, multiple comorbidities, reluctant (or unfit) for corticosteroids and invasive diagnostic procedures like bone marrow biopsy, and not satisfied with the available therapy from other systems of medicine. Further clinical trials with large sample size are required to substantiate the present case study findings.
Keywords: ayurveda, ecchymosis, idiopathic, ITP, purpura, raktapitta
ITP, Immune thrombocytopenic purpura; CAM, Complementary and alternative medicine; IVIg, Intravenous immunoglobulin; ANA, Anti-nuclear antibodies; IV, Intravenous; OHAs, Oral hypoglycemic agents; RUTI, Recurrent urinary tract infections; TRAs, Thrombopoietin receptor agonists
Immune thrombocytopenic purpura (ITP) is a bleeding disorder characterized by thrombocytopenia (platelet count less than 150,000/mcL). The course is more chronic in adults associated with higher mortality in older patients.1 Idiopathic thrombocytopenic purpura is the condition of having a low platelet count of no known cause. As most causes appear to be related to antibodies against platelets, it is also known as ITP. Platelet counts below 50,000/mcL increase the risk of bleeding from trauma and counts below 20,000/mcL may cause spontaneous bleeding. ITP may be either acute or chronic..2 Incidence of ITP is around 3/100,000 person-years, both persistent (more than 3 months duration after diagnosis) and chronic ITP (more than 12months duration after diagnosis) affect 70% of adult patients.3 In acute ITP cases patients usually suffer from bruising; petechiae, bleeding gums and epistaxis (in patients having the platelet count below 20,000/mcL). In extreme cases of ITP (platelet count below 20,000/mcL), serious complications such as bleeding into the lungs, brain, or other vital organs can occur.2 Clinical manifestations include purpura, petechiae and ecchymosis that occur primarily in the lower and upper extremities. Platelet counts less than 10,000/mcL can be associated with spontaneous widespread hematomas.1 The first line therapy for ITP includes corticosteroids, intravenous immunoglobulin (IVIg) and anti-Rh (D) whereas the second line therapy includes Rituximab, splenectomy and thrombopoietin receptor agonists (TRAs). None of them reliably induce durable remission in the majority of ITP patients.4
Elderly patients having chronic ITP with extreme low platelet counts, having multiple medical comorbidities and are reluctant to undergo invasive diagnostic procedures like bone marrow biopsy and also reluctant (or not suitable for) to take corticosteroids may seek the help of Complementary and Alternative Medicine (CAM) therapies for sustained relief. Ayurveda is an ancient Indian system of medicine, in which ITP could be correlated with a condition of Tiryak Raktapitta.5,6 As per the previously published case reports, Ayurvedic treatment seems to be beneficial in the management of ITP.7-10 The present case report deals with an elderly patient having chronic ITP (having extremely low platelet counts of lesser than 10,000/mcL) with multiple comorbidities such as obesity, schizophrenia and T2DM (type 2 diabtetes mellitus) and came to our care for Ayurvedic treatment with the hope for sustained and better relief. Written informed consent has been taken from the patient for the publication of this case report and accompanying images.
A 65 year old female patient came to our care (18.11.2021) with the complaints of ecchymosis (large area of skin discoloration caused by extravasation of blood into the subcutaneous tissue) on both upper extremities (Figures 1 & 2) and fatigue (since 07.11.2021). The patient was diagnosed as having chronic ITP and the investigation reports have revealed low platelet counts/severe thrombocytopenia (9700 to 10000/mcL), elevated erythrocyte sedimentation rate (ESR) levels (38 mm/hr), positive Anti-nuclear antibodies (ANA) and decreased hemoglobin (9.8 g/dL) levels (Table 1) (15.11.2021). All these signs& symptoms have started insidiously and they were gradually progressive. Previous history has revealed that the patient got hospitalized (17.08.2021 to 22.08.2021), received intravenous (IV) fluids, antibiotics, antacids, antipyretics, antimalarial drugs, nebulization, oxygen and other supportive care for the treatment of Plasmodium vivax malaria and urinary tract infection (Table 1). Approximately after three months of hospitalization (07.11.2021), the patient has developed severe thrombocytopenia with ecchymosis on both upper extremities extremities (Figures 1 & 2)without having any other symptoms except fatigue.
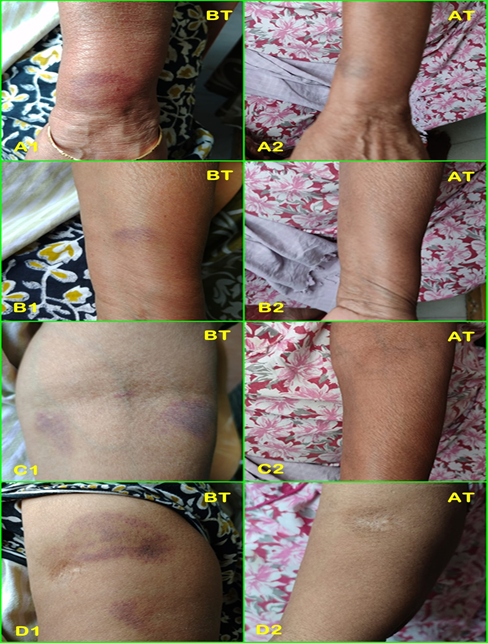
Figure 1 Ecchymotic patches on the left hand.
BT-Before therapy; AT-After therapy (after completion of one year of therapy); A1&A2-Ecchymotic patches on the left dorsal aspect of the wrist before and after therapy respectively; B1&B2- Ecchymotic patches on the left forearm before and after therapy respectively; C1&C2- Ecchymotic patches on the left antecubital fossa before and after therapy respectively; D1&D2- Ecchymotic patches on the left lateral aspect of the arm before and after therapy respectively;
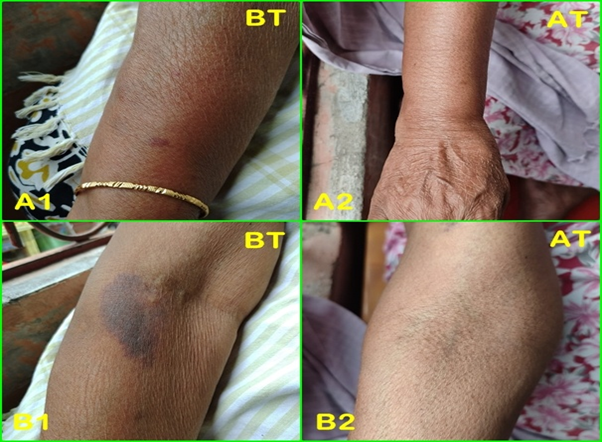
Figure 2 Ecchymotic patches on the right hand.
BT-Before therapy; AT-After therapy (after completion of one year of therapy); A1&A2- Ecchymotic patches on the right dorsal aspect of the forearm before and after therapy respectively; B1&B2- Ecchymotic patches on the right antecubital fossa before and after therapy respectively;
The patient has also been suffering with schizophrenia (since 1989), obesity (since 2001), and T2DM (since 2010) and has been taking antipsychotics (Olanzapine) and oral hypoglycemic agents (OHAs) regularly. The patient has also provided the history of recurrent urinary tract infections (RUTI) caused by Escherichia coli (E. Coli) bacteria and frequent hospitalizations for the same. Patient was non smoker, non alcoholic and doesn’t have positive family history for any autoimmune disease. Patient is not having any drug or food allergy. Initially, patient has approached a hematologist (07.11.2021) for the management of severe thrombocytopenia, and the hematologist has suggested bone marrow biopsy and oral corticosteroids after doing all the necessary investigations (Table 1). The patient was reluctant to undergo invasive diagnostic procedure like bone marrow biopsy and also not willing to take oral corticosteroids with the fear of their side effects. Due to this reasons, the patient has approached us (18.11.2021) for Ayurvedic treatment in the hope of better and sustained relief.
At the time of examination (18.11.2021), ill defined, dusky red to violaceous, multiple ecchymotic patches/macules of different sizes over left wrist, forearm, antecubital fossa and arm as well as on the right antecubital fossa and forearm (Figures 1 & 2). The lesions were persistent and non progressive. The patient denied any history of epistaxis or bleeding from natural orifices, trauma, or surgery. There is no positive family history of bleeding disorders. There was no hepatosplenomegaly and lymphadenopathy. The patient denied any history of fever, night sweats and weight loss. There is no history of tenderness, joint swelling, and mucocutaneous bleeding. Heart rate, respiratory rate, blood pressure, Sp02, body temperature and other vital signs were within normal limits. The patient was overweight (90kg). The investigation reports have revealed extremely low platelet counts (9700 to 10000/mcL), elevated ESR levels (38mm/hr), positive ANA, decreased hemoglobin (9.8g/dL) levels, negative Anti-dsDNA and mild anisopoikilocytosis (Table 1). Peripheral smear has revealed reduced number of platelets along with plenty of giant platelets. Activated partial thromboplastin time (APTT) levels were high and anti globulin test was negative. HIV I & II, HBsAg and HCV I & II were negative (Table 1).
|
Date |
Name of the investigation |
Report |
|
17.08.2021 & 18.08.2021 |
LFT (total bilirubin, direct & indirect bilirubin, SGOT (AST), SGPT (ALT), ALP, total protein, serum albumin, globulin and A/G ratio) |
WNL |
|
Malaria antigen test (MP/PF) Pan PV PF |
Positive Positive Negative |
|
|
Random plasma glucose |
224 mg/dl (H) |
|
|
Serum electrolytes (Sodium - Na+, Potassium - K+) |
WNL |
|
|
Urine analysis (color, appearance, specific gravity, pH, protein, sugar, ketone bodies, nitrites, leukocytes, urobilinogen and urine bilirubin); Urine microscopic examination (pus cells, epithelial cells and RBC); Urine culture & sensitivity |
WNL
WNL
Negative |
|
|
Total count & Differential count (total leukocyte count, neutrophils, lymphocytes, eosinophils, monocytes); Platelets Hemoglobin |
WNL 61000 /mcL (L) 11.7 g/dl (L) |
|
|
Blood grouping Blood group Rh type |
O Positive |
|
|
Scrub typhus rapid card test (serum scrub typhus antibodies by immunochromatography assay) |
Negative |
|
|
Dengue IgG, IgM, NS1 rapid test |
Negative |
|
|
IDV rapid test (HIV I & HIV II) |
Non reactive |
|
|
HBsAg card test & Anti HCV rapid test |
Non reactive |
|
|
NCCT chest report |
Few fine reticular opacities in bilateral basal segments (CO-RADS 1). Mild haziness in lingular segments of left lung adjacent to the left oblique fissure (fissural effusion). Cardiomegaly; |
|
|
USG abdomen |
No abnormality detected |
|
|
2D Echo report |
EF - 60%; Mild concentric LVH; Mild MR, TR & PAH; |
|
|
07.11.2021 & 08.11.2021 |
Total count & Differential count |
WNL |
|
Total RBC count |
3.4 million/mm3 (L) |
|
|
ESR |
16 mm for first hour (H) |
|
|
Hemoglobin |
9.6 g/dl (L) |
|
|
Platelet count |
11000 /mcL (L) |
|
|
Malaria parasite |
Negative |
|
|
Bleeding time |
13.10 minutes |
|
|
Clotting time |
9.05 minutes |
|
|
Prothrombin time Control value Test value INR value |
14 seconds 28 seconds 2 seconds |
|
|
Activated partial thromboplastin time (APTT) Control value Test value |
21 seconds (H) 37 seconds |
|
|
HbA1c |
6.5 % |
|
|
CRP |
1.9 mg / dL |
|
|
LFT, Serum creatinine & BUN |
WNL |
|
|
Ferritin (IFA method) |
37.8 ng / mL (L) |
|
|
Dengue antigen antibodies test - Rapid test |
Negative |
|
|
Anti globulin test (direct & indirect) |
Negative |
|
|
HIV I & II, HBsAg, HCV I & II |
Negative |
|
|
Peripheral smear Platelets
Platelet count |
Reduced on smear, plenty of giant platelets are seen; Severe thrombocytopenia; 25000 /mcL |
|
|
Anti-Nuclear antibodies (ANA) Double standed DNA (Anti-ds DNA) |
1.8 (Positive) 10.0 IU (Negative) |
|
|
12.11.2021 |
Platelet count |
9700 /mcL (L) |
|
15.11.2021 |
ESR |
38 mm / hr (H) |
|
Hemoglobin |
9.8 g / dL (L) |
|
|
MCHC |
27 g / dl (L) |
|
|
RDW-SD |
54.4 fL (H) |
|
|
RDW-CV |
16 % (H) |
|
|
Vitamin B 12 |
> 2000 pg / mL (H) |
|
|
Platelet count |
10000 /mcL (L) |
|
|
26.11.2021 & 27.11.2021 |
Urine culture and sensitivity
|
Escherichia Coli isolated; Colony count - 10*5 CFU / ML Sensitive to Imipenem, Pipevacillin, Tazobactam, Amikacin, Gentamicin, Cefepine; |
|
Complete urine analysis |
WNL |
|
|
Hemoglobin |
10.4 g / dL (L) |
|
|
PCV (Hematocrit) |
24.6 % (L) |
|
|
Platelet count |
50000 /mcL (L) |
|
|
MCH |
25.4 pg / cell (L) |
|
|
MCHC |
30.2 g / dL (L) |
|
|
ANA |
1.31 (Positive) |
|
|
29.11.2021 |
ESR |
70 mm / hr (H) |
|
10.12.2021 |
Hemoglobin |
9.6 g / dL (L) |
|
Platelet count |
30000 / μL (L) |
|
|
03.01.2022 |
ESR |
80 mm / hr (H) |
|
Hemoglobin |
10 g / dl (L) |
|
|
Platelet count |
30000 /mcL (L) |
|
|
22.02.2022 |
HbA1c |
4.80 % |
|
Fasting blood sugar |
80.9 mg / dL |
|
|
Lipid profile |
WNL |
|
|
Serum iron |
43.5 mcg / dL (L) |
|
|
TIBC (total iron binding capacity) |
WNL |
|
|
KFT (serum creatinine, uric acid, blood urea and BUN) |
WNL |
|
|
Vitamin B12 & Serum calcium |
WNL |
|
|
25-hydroxy Vitamin D |
17.71 ng / ml (L) |
|
|
Thyroid stimulating hormone (TSH) |
7.87 μ IU / ml (H) |
|
|
ESR |
6 mm / hr |
|
|
16.09.2022 |
Hemoglobin |
11.1 g / dL (L) |
|
Urine routine & microscopic examination |
WNL |
|
|
Platelet count |
50000 / mcL (L) |
|
|
03.01.2023 |
Lipid profile, Serum electrolytes, FBS, Thyroid profile, LFT, KFT, urine routine and microscopic examination |
WNL |
|
Hemoglobin |
10.8 g / dL (L) |
|
|
Platelet count |
27000 / mcL (L) |
Table 1 Investigation reports
LFT-liver function tests; SGOT-serum glutamic oxaloacetic transaminase; AST-aspartate transaminase; SGPT-serum glutamic pyruvic transaminase; ALT-alanine transaminase; ALP-alkaline phosphatase; A/G ratio-albumin/globulin ratio; WNL-within normal limits; MP-malarial parasite; PF-Plasmodium falciparum; PV-plasmodium vivax; H-high; RBC-red blood cells; L-Low; IgG-immunoglobulin G; IgM-Immunoglobuliln M; NS1-non-structural protein of dengue virus; IDV-indinavir; HIV-human immunodeficiency virus; HBsAg-hepatitis B surface antigen; HCV-hepatitis C virus; NCCT-non-contrast computerized tomography; CO-RADS-corona virus disease (COVID-19) reporting and data system; USG-ultrasonogram; 2D echo-two dimensional echocardiography; EF-ejection fraction; LVH-left ventricular hypertrophy; TR-Tricuspid regurgitation; MR-mitral regurgitation; PAH-pulmonary arterial hypertension; ESR-erythrocyte sedimentation rate; INR-international normalized ratio; HbA1C-hemoglobin A1C; CRP-C-Reactive protein; BUN-blood urea nitrogen; IFA-immunofluoroscence assay; MCHC-mean corpuscular haemoglobin concentration; RDW-SD-Red cell distribution width standard deviation; RDW-CV-Red cell distribution width standard deviation corpuscular volume; PCV-packed cell volume; MCH-mean corpuscular haemoglobin; KFT-kidney function tests; FBS-fasting blood sugar
Based on history, examination, and investigation reports, the patient was diagnosed as a case of chronic ITP. The diagnosis of ITP is a diagnosis of exclusion. Isolated thrombocytopenia without any physical signs (except for signs of bleeding) is important for diagnosing ITP. The secondary causes of ITP should be excluded such as leukemia, systemic lupus erythematosus (SLE), medications, cirrhosis, HIV, HCV, antiphospholipid syndrome, von Willebrand factor deficiency etc. Platelets are abnormal in size and appearance with the counts usually around 20,000/mcL. About 10% of patients with ITP are also anemic. Bleeding time is prolonged in ITP patients. A bone marrow examination may be performed when the diagnosis is in doubt. Detection of antiplatelet antibodies in the blood is considered to confirm the diagnosis of ITP.2 but according to some other studies the measurement of platelet-associated antibodies is not helpful as it lacks both specificity and sensitivity.1 In present case, the diagnosis of chronic ITP has been made based on the clinical features and investigation findings (Table 1). Due to the patient’s unwillingness bone marrow biopsy has not been conducted. Ayurvedic diagnosis of Tiryak Raktapitta has been made based on the clinical features (Figures 1 & 2). No assessments were carried out except laboratory investigations (platelet counts and other hematological indices). Ayurvedic treatment was planned and implemented by considering age of the patient, lifestyle, bleeding risk and patient preference.
Bleeding is the most common clinical manifestation of ITP and elderly patients are more at the risk of bleeding and related morbidity. The pathogenesis of ITP is complex, involving alterations in immunity (both humoral and cellular). Adult patients with ITP have increased morbidity and mortality especially those unable to maintain a stable platelet counts more than 30 × 109/L despite therapy. Bleeding is the most common clinical manifestation of ITP. Purpura, usually on the extremities (dry purpura) may often appear without any precipitating event. Some patients may display oral hemorrhagic bullae (wet purpura), which may be a harbinger of more severe bleeding manifestations elsewhere. Fatigue is an underappreciated symptom in patients with ITP. Significant improvements in several health-related quality of life measurements and also in fatigue have been observed in successfully-treated patients.4 The present case also an elderly patient had dry purpura, fatigue and severe thrombocytopenia.
ITP can be correlated with a disease condition called Raktapitta in Ayurveda. Raktapitta is a bleeding disorder caused by the vitiation of Rakta (blood) and Pitta (heat energy in the body). Raktapitta is classified in to three groups i.e., Urdhwagata (epistaxis, hemetemesis etc), Adhogata (melena, hematochezia, hematuria etc) and Tiryaggata (purpura, ecchymosis etc). ITP comes under the domain of Tiryaggata Raktapitta and it is considered as Yaapya (treatable but not curable). Raktapitta is an umbrella term that includes various bleeding disorders, such as epistaxis, hemetmesis, menorrhagia, melena, hematochezia, hematuria etc. Pitta gets vitiated by the Ushna (hot), Teekshna (sharp), Amla (sour), Katu (spicy), and Lavana (salty) predominant dietary habits and activities that cause excessive heat in the body. Vitiated Pitta further vitiates the Rakta and leads to the manifestation of Raktapitta. Raktapitta disease mainly affects Raktavaha Srotas (blood vessels, heart, liver and spleen) and eventually leads to bleeding from various sites. Prognosis of Raktapitta depends on the association of Dosha, strength of the patient, track involved in bleeding, and severity of symptoms. Pandu Roga (anemia) is a complication of Raktapitta. Both Shodhana (purificatory) and Shamana Chikitsa (pacifying therapy) are mentioned for Raktapitta and they should be implemented by considering various factors such as patient’s age, comorbidities, physical strength, season etc..7 Tiryaggata Raktapitta is a Tridoshaja (three body humors) disease characterized by bleeding into skin pores or subcutaneous tissue.10
Patient was hospitalized (17.08.2021 to 22.08.2021) and received treatment for Plasmodium vivax malaria (Vishama Jwara) and urinary tract infection (Table 1) before approaching us (18.11.2021). Approximately after three months of hospitalization (07.11.2021), the patient has developed ecchymosis on both upper extremities (Figure 1&2). During the post hospitalization period or post malarial fever period (22.08.2021 to 17.11.2021), patient has consumed excessive spicy, sour and salty foods such as pickles, potato chips etc that might have caused Pitta Prakopa and Rakta Dushti (vitiation of Pitta and blood) and ultimately the manifestation of Raktapitta. The present case is one of the best example for Nidaanaarthakara Roga (a disease causing another disease) i.e., Jwara/Vishama Jwara (malarial fever) causing Raktapitta (ITP). Based on the purple patches (ecchymosis) on peripheral body parts (upper extremities) (Figure 1&2) and absence of bleeding from any other sites, the present case has been diagnosed as Tiryaggata Raktapitta. Patient has been taking OHAs and antipsychotics at the time of visit (18.11.2021) and those drugs were not stopped during Ayurvedic treatment. Shodhana treatment was not planned as the patient was unfit due to an elderly age, medical comorbidities such as obesity and T2DM and also patient’s preferences. Shamana treatment is given by using the formulations that are having Pitta and Rakta Shamaka (pacifying) properties. Putapakwa Vishama Jwarantaka Loha (PVJL) tablets, Raktashamak tablets, Platenza tablets and Samshamani Vati were prescribed for the period of 10 days (18.11.2021 to 27.11.2021) (Table 2). Strict dietary restrictions were followed throughout the treatment and follow up period especially for sour, salty, spicy food items.
|
Duration |
Medicine |
Dose |
Frequency |
|
18.11.2021 to 27.11.2021 |
1. Putapakwa Vishama Jwarantaka Loha tablets |
125 mg |
Twice daily |
|
2. Raktastambhak tablets |
700 mg |
Twice daily |
|
|
3. Platenza tablets |
500 mg |
Twice daily |
|
|
4. Samshamani Vati |
1 gm |
Twice daily |
|
|
28.11.2021 to 17.12.2021 |
1. Putapakwa Vishama Jwarantaka Loha tablets |
125 mg |
Once daily |
|
2. Raktastambhak tablets |
350 mg |
Twice daily |
|
|
3. Platenza tablets |
500 mg |
Twice daily |
|
|
4. Chandraprabha vati |
1 gm |
Twice daily |
|
|
18.12.2021 to 25.02.2022 |
1. Raktastambhak tablets |
350 mg |
Twice daily |
|
2. Platenza tablets |
500 mg |
Twice daily |
|
|
3. Abhra Loha tablets |
350 mg |
Twice daily |
|
|
26.02.2022 to 31.10.2022 |
1. Abhra Loha tablets |
350 mg |
Twice daily (intermittently) |
|
2. Raktastambhak tablets |
350 mg |
Once daily (intermittently) |
|
|
3. Platenza tablets |
500 mg |
Once daily (intermittently) |
|
|
4. Asthiposhak tablets |
500 mg |
Once daily |
|
|
01.11.2022 to 31.03.2023 |
Follow up period (no Ayurvedic medicines have been prescribed during this period) |
||
Table 2 Intervention
By considering that the present case of ITP (Raktapitta) is a Nidaanaarthakara Roga and it has occurred due to the consequences (complication) of malarial fever (Vishama Jwara), PVJL has been prescribed. Shuddha Parada (purified mercury), Shuddha Gandhaka (purified sulfur), Bhasmas (calces) of Swarna (gold), Loha (iron), Tamra (copper), Abhraka (mica), Vanga (tin) etc are the main ingredients of PVJL. PVJL is indicated for all types of fevers (chronic and intermittent), anemia, splenomegaly, and jaundice.11 Raktastambhak tablets are proprietary Ayurvedic medicine and it is indicated in bleeding disorders. Nagakeshara (Mesua ferrea), Shuddha Laksha (Laccifer lacca), Mocharasa (Bombax malabaricum), Shuddha Gairika (purified red ochre) are the main ingredients of Raktastambhak tablets.12 Platenza tablets contain Eranda Karkati (Carica papaya leaf extract) along with Bhudhatri (Phyllanthus maderaspatensis), Maricha (Piper nigrum) and Guduchi (Tinospora cordifolia) and it is known to increase the platelet count along with symptomatic relief in dengue fever associated with thrombocytopenia.13 Guduchi is the only ingredient of Samshamani Vati and it is having Jwaraghna (antipyretic) and Rakta Shamaka properties.14 PVJL has been prescribed to manage the consequences (complications) of Vishama Jwara; Raktastambhak tablets were prescribed to control the ecchymosis on upper extremities; Platenza tablets were prescribed to improve the platelet count and Samshamani Vati has been prescribed for its Rakta Shamaka property. After consuming these medicines for the period of ten days (18.11.2021 to 27.11.2021), the patient has developed UTI and the treatment has been revised (Table 2).
The patient came with fever, chills, dysuria and diagnosed as having UTI on 27.11.2021 (Table 1). Chandraprabha Vati has been prescribed to manage the UTI for 3weeks (28.11.2021 to 17.12.2021). Treatment was revised again on 18.12.2021, after getting relief in UTI (Table 2). The patient took medicines regularly from 18.11.2021 to 25.02.2022 (more than 3 months) and after that the medicines were taken intermittently for the period of 8 months (from 26.02.2022 to 31.10.2022). No medicines were prescribed (except OHAs and antipsychotics) for the period of 5months (from 01.11.2022 to 31.03.2023) (follow up period) (Table 2). No adverse effects were reported with the any of the above Ayurvedic formulations by the patient during treatment period. The patient got clinically meaningful improvement with Ayurvedic medicines especially in UTI, fatigue and general quality of life (though it was not assessed by using any measuring scale or questionnaire). Platelet counts were improved from initial 9700-10000/mcL to 30000-50000/mcL (Table 1), ESR levels were reduced from 80mm/hr to 6mm/hr, and hemoglobin levels were improved from initial 9.8g/ dL to 11.1g/ dL. HbA1c levels were also improved though no Ayurvedic medicines were prescribed for the management of T2DM. Ecchymotic patches on both upper extremities were completely disappeared (Figures 1 & 2) with no further recurrences. The patient was stable with improved quality of life and energy levels and also satisfied with her condition during follow up period. Ayurvedic treatment seems to be promising in the management of chronic ITP and generates hope for those patients who are having extreme thrombocytopenia, multiple comorbidities (such as obesity, T2DM and UTI in present case), not willing or unfit for corticosteroids and invasive diagnostic procedures like bone marrow biopsy, and not getting satisfactory relief in modern medicine.
Ayurvedic treatment has improved the platelet counts, hematological indices and quality of life in an elderly, chronic ITP (Tiryaggata Raktapitta) patient having multiple comorbidities (such as obesity, T2DM, UTI and Schizophrenia). Ecchymotic patches were completely disappeared without any further recurrences by Ayurvedic treatment. The present case of ITP (Raktapitta) is a good example for Nidaanaarthakara Roga as it has occurred due to the consequences of malarial fever (Vishama Jwara). Ayurvedic treatment seems to be promising in the management of chronic ITP and generates hope for those patients who are having extreme thrombocytopenia, multiple comorbidities, reluctant (or unfit) for corticosteroids and invasive diagnostic procedures like bone marrow biopsy, and not getting satisfactory relief in modern medicine. Though the present case study findings can’t be generalized, further clinical trials with large sample size are required to substantiate the present study findings.
The authors are grateful to Dr P Hima Sagara Chandra Murthy, Retired Professor, PG department of Rasa Shastra, Dr N.R.S. Government Ayurvedic College, Vijayawada, for his help in planning the treatment for the present case.
There is no conflicts of interest.
None.

©2023 Gupta, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.