International Journal of
eISSN: 2381-1803


Research Article Volume 11 Issue 3
1Physical Therapy and Occupational Therapy Department, S
2Laboratory of Investigation in Biocomunication, Physical Exercise and Cardiac Autonomic Modulation (LIBEM) 3Physical Education Department, Marilia University (UNIMAR), Brazil
3Physical Education Department, Marilia University (UNIMAR), Brazil
Correspondence: Jose Alfredo Ordenes Mora, Physical Therapy and Occupational Therapy Department, S, Tel +5514 3402 1331
Received: April 20, 2018 | Published: May 18, 2018
Citation: Mora JAO, Chagas EFB, Camilo GF, et al. Acute effect of Quantec therapy on cardiovascular risk factors and autonomous modulation of heart rate. Int J Complement Alt Med. 2018;11(3):149-153. DOI: 10.15406/ijcam.2018.11.00387
Background: Quantec is a new instrumental bioinformation therapy, that acts on the patient's electromagnetic fields to restore the body's normal functions. Heart rate variability (HRV) is an important biomarker applied in research to measure physiological effects.
Method: Approved by the Ethics Committee (1068/2014). 10 individuals, mean age 60.4±6.4 years, with at least one cardiovascular risk. An instrumental biocommunication device (Quantec 6.0-R2-08, Munich, Germany) was used for an acute application of 12 seconds of treatment. The recording of the HR and the RR intervals (Polar RS800CX, Polar Electro Oy, Kempele, Finland) was done with the volunteer sitting in a state of rest for 10 minutes before application and 5 minutes afterwards. Only the RRi series with more than 95% sinus beats were analyzed, having selected the 256 most stable points and calculated the HRV indices (Software Kubios HRV, version 2.0, University of Kuopio, Finland)
Results: Δ variation between pre and post moments of the LH/HF ratio had a significant negative correlation (p = 0.006). Glycemia showed a significant reduction (p = 0.010) as did the Triglycerides (p = 0.024).
Discussion: Quantec had a positive effect on blood concentration values of cholesterol, triglycerides and glycemia. In the altered LH/HF values, it showed greater reductions in sympathetic activity and an increase in parasympathetic activity.
Conclusion: Acute treatment with Quantec was effective in reducing metabolic imbalances.Keywords: hypertension, additional therapies, dyslipidemia, diabetes mellitus, holistic health
Despite advances in scientific research, the prevalence of dyslipidemias (DLP), Hypertension (SAH) and Diabetes Mellitus (DM) continues to increase worldwide.1–6 These are the main risk factors for the cardiovascular diseases that generally affect the heart's autonomic nervous system, this being the subject of intensive scientific research. These studies suggest that a decrease in the vagal tone may precede the development of one of these critical risk factors for cardiovascular diseases. Thus, over the last few years this system has been the subject of intensive research. One of the outstanding methods used in the research was the Heart Rate Variability (HRV) study, due to its great disease forecasting power, a lower HRV being associated with greater cardiovascular morbidity and mortality.7–10 As metabolic and cardiovascular diseases have reached epidemic proportions worldwide and are difficult to cure, complementary medicine based on quantum physics has awakened great interest and opened up new research perspectives and areas, such as magnetobiology and biomagnetism.11,12
The theory proposes acting on diseases through the transmission of specific electronic vibrations, to bring the atom back to the normal vibration; thereby eliminating the disease.13 This technique involves using instrumental biocommunication devices that are capable of interpreting imbalances in the body's electromagnetic fields, re-sending electronic vibration patterns in order to restore normal patterns.
Quantec is an instrumental bioinformation equipment, which through the white noise diode can capture the subtle bodies and connect with the consciousness. It has been used as a direct interface between an information generator and the patient's subconscious to perform treatment modifying altered patterns of functioning through change in the internal information of each individual.14,15
As the heart generates a huge source of bioinformation for the whole body and is responsible for the being's functioning as a whole, it delivers biological information through heart sounds, pulse and the heart rate,16 this study's hypothesis is that a vibration therapy session by instrumental biocommunication increases the heart's parasympathetic modulation and shows an improvement in the clinical characteristics of individuals with hypertension, diabetes and dyslipidemia.
The study concerned 10 individuals of both sex, aged between 52 and 67 with a previous clinical diagnosis of imbalance in at least one of the risk factors listed: SAH, DLP and DM. It did not include those with respiratory, neurological and metabolic diseases of a different nature. All were informed about the experimental procedures and signed the free and informed consent form. Research study approved under the number1068/2014. The assessments were performed during the morning, in order to formally record the circadian variations in the organism17. The experiment was performed in an air-conditioned environment, temperature at 23+2°C and air relative humidity at 50+10%.
Application of Instrumental Bioinformation
On the second evaluation, 2 days after the last detection, the patient was asked to remove any kind of device or instrument that might generate any kind of electromagnetic interference (mobile, watch, iPad, etc). The patient’s blood pressure was measured by the auscultatory method, after remaining in a seated position for 20 minutes. The pressoric levels were classified according to the 6th Brazilian Arterial Hypertension Directive18; Cholesterol, triglycerides and glycemia by means of a reflectance spectrophotometry biochemical analyzer (Accutrend Plus, Roche Diagnostics, 2007). The total cholesterol and triglycerides concentrations were classified according to the 5th Brazilian Dyslipidemia and Aterosclerosis Prevention Directive,19 and the glycemia was classified according to the Brazilian Cardiology Society Directive.20
Then the RR interval (RRi) transmitter was placed on the patient’s chest at the height of the xiphoid process (Polar RS800CX, Polar ElectroOy, Kempele, Finland). The receiver was held by the researcher and the patient remained seated and held on the palm of his hand the device's gold clip, which contains the white noise diode.
The RRi was recorded for 10 minutes, with the volunteer breathing spontaneously and after stabilization of the HR. The Quantec treatment starts at the minute 10 and lasted for 12 seconds. The recording of the RRi was interrupted at minute 10 and the BP and the blood biochemistry measured again. These measurements were repeated after 30 minutes.
Analysis of the HRV data
The instantaneous HR and RRi were converted into text files and analyzed (Kubios HRV, version 2.0, University of Kuopio, Finland). Only the series with over 95% of sinus rhythm beats and the 256 most stable points of the stretches were selected: before and after the application of bioinformation.
In the time domain, the following statistical calculations were carried out: average and standard deviation of the HR values in beats per minute (bpm) and of the RRi (ms); standard deviation of the square root of the mean of the squares of the differences between the successive normal intervals (RMSSD), expressed in milliseconds (ms); this last index representing the parasympathetic modulation.21,22
We also calculated the SD1 and SD2 indices of the Poincaré plot, which is a map of points in Cartesian coordinates, where every point is represented on the horizontal X axis (abscissae) by the previous normal RRi and on the Y axis (ordinate) by the following RRi. The standard deviation of the perpendicular points and along the length of the identity line give rise to the SD1 and SD2 indices respectively. The SD1 index measures the standard deviation of the distances of the points towards the diagonal y=x, is related to the short-term variability, is influenced by the respiratory sinus arrhythmia and represents the parasympathetic activity. The SD2 measures the standard deviation of the distances from the points towards the straight line y =-x+RRm, where RRav is the mean of the RRi, with long-term variability and reflects the overall variability. The relationship between them (SD1/SD2) shows the ratio between the short and long variations of the RR intervals.22,23
For the spectral analysis, an autoregressive model was used and the following spectral indices calculated: high frequency (HF – 0.15 at 0.4Hz) which corresponds to the respiratory modulation and to the parasympathetic modulation of the vagus nerve on the heart; low frequency (LF–0.04 at 0.15Hz), which represents sympathetic and parasympathetic modulation, with sympathetic predominance; and the LF/HF ratio, which represents the sympathovagal balance.19 The LF data was presented in absolute values (ms2) and the HF as a standardized unit (un). The standardized data was calculated by dividing the spectral power density of a given band (i.e. HF) by the total power, subtracting the very low fre
Statistical analysis
The results were organized in the descriptive statistical form, with mean, standard deviation (SD) and confidence interval (CI 95%) values. The standard distribution was checked by the Shapiro-Wilk with Lillifors correction. In order to analyze the variation between the pre (M1) and post operation (M2) moments, and also 30 minutes after the end of the operation (M3), the delta variation (Δ) (post-pre) was calculated. The variation in relation to the initial values are graphically represented with their respective moment correlation x Pearson product coefficients. To analyze the acute effect of the intervention on the HRV indices, the t student test was applied for paired samples and their non-parametric similar (Wilcoxon) when the data did not represent the normal distribution. An ANOVA was constructed for repetitive measurements in order to test the time effects on SBP, DBP, GL, TG and TC Mauchly's test was used to test the sphericity hypothesis. If the sphericity hypothesis was rejected, the analyses were based on the Greenhouse-Geisser multivaried test. When the time effect was statistically significant, the multiple LSD comparison test was carried out. For all the analyses the SPSS software version 19.0 Windows version was used, adopting a significance level of 5%.quency band and multiplying by 100.24
The average age of the sample elements was 60.4±6.4, with minimum age 52 and maximum age 67 years. The sample was composed of 6 men (60%) and 4 women (40%). SAH (80%) was the most prevalent factor, followed by DM (40%) and DLP (40%). Table 1 presents the systolic arterial pressure (SBP) values, Diastolic blood pressure (DBP), GL, TG and TC for moments M1, M2 and M3. A significant reduction was identified between M1 and M2, and between M1 and M3 for SBP. GL presented similar reduction behavior (p=0.010), being significant between M1 and M2, and M1 and M3. The variation between the moments was significant (p = 0.024) for the TG values, a significant difference being observed between moments M2 and M3.
The Δ variations of intervals M2-M1 and M3-M1 in relation to the initial M1 value for the variable, TC, GL and TG, are graphically represented with their respective moment correlation x Pearson product coefficient (r) and significance value (p) in Figure 1. The significant correlation between the initial values and the Δ variation were not verified. This relationship with the initial values was only non-identifiable for the TG values in the analysis of the Δ variation between the M3 and M1 moments in relation to the initial M1 values. There are good correlation values despite a reduced size of the sample, which does not permit statistical significance. The Δ variations of intervals M2-M1 and M3-M1 in relation to the initial M1 value for the variable, SBP and DBP, are graphically represented with their respective moment correlation x Pearson product coefficient (r) and significance value (p) in Figure 2. The Δ variation between the M1 and M3 moments of the DBP presented negative and significant correlation (p = 0.012) with the initial M1 values.
Table 2 presents average and standard deviation (SD) of the HRV indices in the pre and post operation moments, followed by the average delta (Δ) variation (post – pre) value and its respective Confidence Interval of 95% (lower | higher). Statistically significant differences between the pre and post operation moments were not observed. Insofar as the delta variation values indicate a reduction trend in the HRV indices measured. Figure 3 present the pre and post-intervention moments in relation to the initial values for the HRV indices referring to parasympathetic and sympathetic values, with their respective Pearson product moment correlation values and significance value (p). A significant correlation between the delta variations and the initial values of the parasympathetic (Figure 1) and sympathetic indices (Figure 2) of the HRV was not observed, indicating that the variations observed were independent of the initial values.
|
Pre |
|
Post |
|
Δ (post-pre) |
|
|
|
MEAN±SD |
|
MEAN±SD |
|
MEAN |
ΔCI 95% |
P value |
MeanHR |
65.4±9.4 |
|
65.0±9.3 |
|
-0.34 |
-0.91 | 0.22 |
0.200t |
RMSSDw |
27.9±19.5 |
|
27.6±21.2 |
|
-0.28 |
-5.42 | 4.86 |
0.721w |
pNN50 |
13.0±21.6 |
|
11.5±22.4 |
|
-1.42 |
-5.44 | 2.58 |
0.442t |
LH |
223.7±153 |
|
217±169 |
|
- 6.70 |
-105 | 91.8 |
0.881t |
HF |
52.8±25.5 |
|
51.2±22.5 |
|
-0.80 |
-9.51 | 7.91 |
0.840t |
LH/HFw |
1.58±1.76 |
|
1.36±1.08 |
|
-0.21 |
-1.13 | 0.70 |
0.959w |
SD1 |
19.7±13.8 |
|
18.5±13.7 |
|
-1.20 |
-6.25 | 3.85 |
0.604t |
SD2 |
42.0±14.0 |
37.3±18.2 |
-4.69 |
-12.3 | 2.99 |
0.201t |
||
Table 2 followed by the average delta (Δ) variation (post – pre) value and its respective Confidence Interval (CI) of 95% (lower|higher)
Note: *p≤ 0.05 significant difference between M1 and M2. t student t test. wWilcoxon test.
SD, standard deviation; RMSSD, root mean square of successive differences; pNN50, the proportion of NN50 divided by total number of NNs; LH, low frequency; HF, High frequency; LF/HF, sympathovagalbalance; SD1, standard deviation of instantaneous beat-to-beat interval variability; SD2, the continuous long-term R/R interval variability.
The Δ variations of the post-pre intervals in relation to the initial values of the LH/HF ratio are graphically represented with their respective moment correlation x Pearson product coefficient (r) and significance value (p) in Figure 4. The Δ variation between the pre and post-intervention moments of the LH/HF ratio presented negative and significant correlation (p=0.006) with the initial values.

Figure 1 Delta variation (Δ) of the Total Cholesterol (TC), Glycemia (GL) and Triglycerides (TG) for the moment immediately after the operation (M2-M1) and 30 minutes after the intervention (M3-M1) in relation to the initial values (M1).
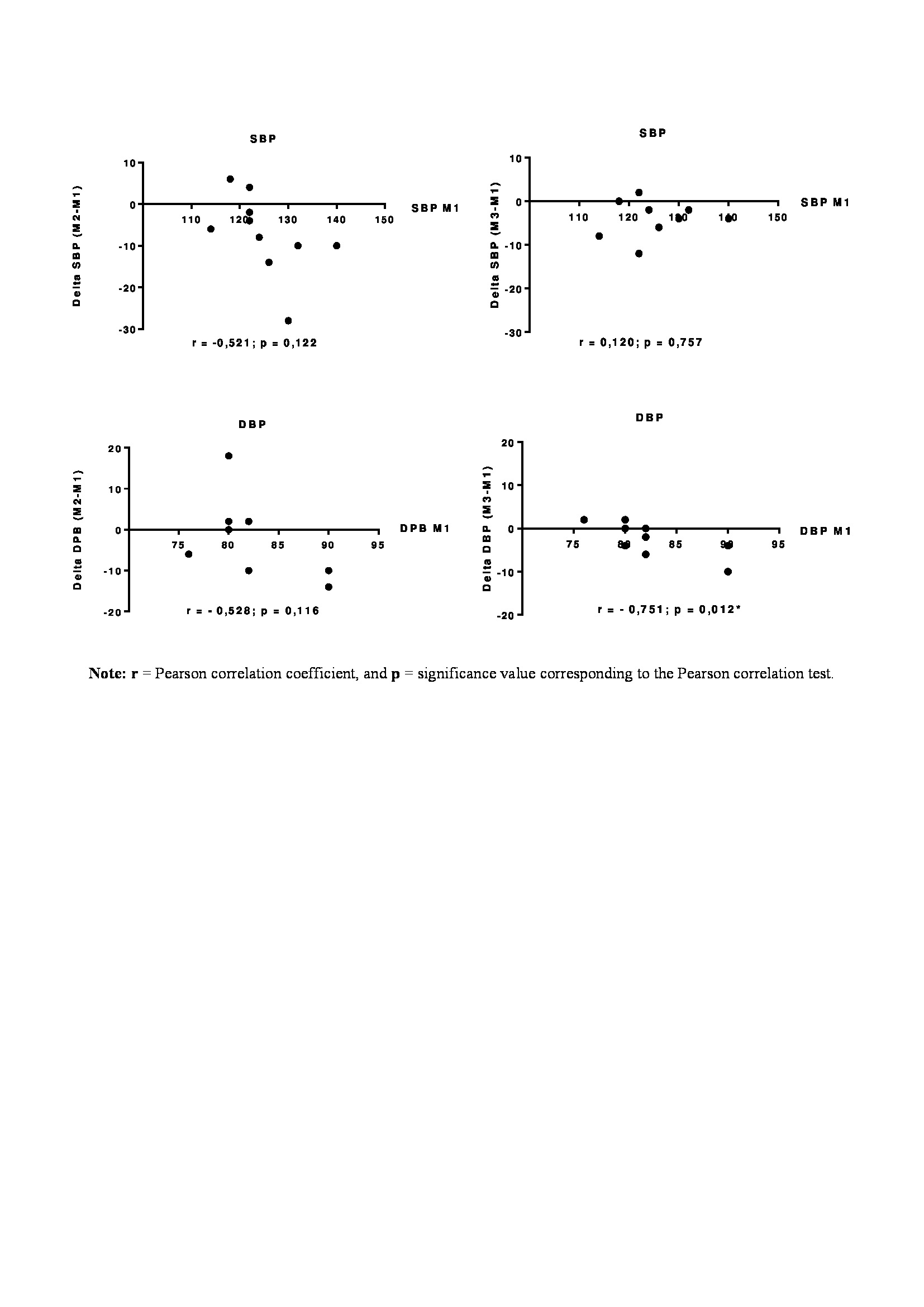
Figure 2 Delta variation (Δ) of the Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) for the moment immediately after the intervention (M2-M1) and 30 minutes after the operation (M3-M1) in relation to the initial values (M1).
All the variables studied (SBP, DBP, GL, TG, TC) decreased after the acute intervention, and according to Table 1, only GL and TG reached statistical significance between the initial moment and at the moments immediately afterwards (M2) and the late moment (M3). There was also a decrease in the sympathetic modulation of the heart rate. SBP presented a significant difference between M1 and M2 and between M1 and M3, demonstrating an effect that was maintained for 30 minutes. DBP did not presents significant difference between the moments, despite the reduction trend. Glycemia presented a significant reduction between M1 and M2, and M1 and M3. TC did not present a significant difference, despite the reduction trend. TG presented a significant increase between the M2 and M3 moments, but not between M1 and M3, suggesting that the effects of the intervention were not maintained 30 minutes after the treatment. The Δ variation between the M1 and M3 moments of the DBP presented a negative and significant correlation (p=0.012) with the initial M1 values, demonstrating that despite the fact that it did not present significant difference in the group, Quantec was selective for the reduction of DBP only in patients who presented alterations in this variable.
|
M1 |
M2 |
M3 |
|
|
||
|
MEAN±PD |
MEAN±PD |
MEAN±PD |
|
p-value |
||
SBP |
125.0±7.4a |
117.8±8.5b |
121.2±5.7b |
0.053 |
|||
DBP |
82.2±4.6 |
80.6±7.7 |
80.0±2.9 |
0.530 |
|||
GL |
95.1±22.3a |
81.2±22.3b |
72.7,4±19.3b |
0.010* |
|||
TG |
210.8±55.7 |
203.6±48.0a |
224.2±59.3b |
0.024* |
|||
TC |
174.9±21.1 |
|
169.0±17.9 |
|
171.9±18.7 |
|
0.324 |
Table 1 Arterial Pressure and biochemical variables for the initial pre- operation moment (M1), after the operation (M2) and 30 minutes after the operation (M3)
Note: * p≤0.05 significant difference between the moments (Anova repeated measurements test). Different letters overwritten indicate significant differences (p≤0.05) between the moments, and the same letters overwritten indicate the absence of significant differences between the moments, (multiple LSD comparison test).
TC, Cholesterol Total; DB, Diastolic Blood Pressure; GL, Glycemia; SBP, Systolic Blood Pressure; TG, Triglycerides
In Figure 4 a negative correlation was observed between the initial values and the delta variation of the values of the LH/HF ratio that represents the sympathovagal balance. These results indicate that patients with very high initial LH/HF values present more reduction in sympathetic activity and an increase in parasympathetic activity. Patients without alterations did not change their initial values, suggesting that the intervention had an individualized positive effect on the sympathovagal balance of each participant. We therefore propose that the observed effects result from a balancing of the biological information of each individual, given that research studies with other forms of bioinformation managed to balance alterations in blood pressure.25,26
Quantec had a positive effect on the values of the blood concentrations of cholesterol, triglycerides and glycemia, demonstrating the ability to act at a cellular level. We noticed that deeper studies are required to understand how each shift in value takes place and why this is different in each Glycemia, Triglyceride and cholesterol molecule, thus making another study with a prolonged treatment is necessary to look at Quantec's efficacy through a constant modulation in the electromagnetic field. Future studies must examine whether the large-scale implementation of these techniques based on the circulatory and autonomous apparatus have a significant impact on reducing the mortality and morbidity risk in patients.
Instrumental bioinformation using Quantec had an effective approach for reducing Blood Pressure, Glycemia, triglycerides and cholesterol and offers a new treatment method with encouraging results for those with cardiovascular risk factors.
None
Author declare there is no conflict of interest

©2018 Mora, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.