eISSN: 2469-2778


Case Report Volume 8 Issue 2
Department of Clinical Pathology,Faculty of Medicine,University of Alexandria, Egypt
Correspondence: Akram Deghady, Department of Clinical Pathology,Faculty of Medicine,University of Alexandria, Egypt
Received: January 03, 2020 | Published: April 24, 2020
Citation: Deghady A, Farahat N, Elhadidy A, et al. Plasma cell leukemia with different expression of CD56 marker in the peripheral blood and bone marrow: A case report. HematolTransfusInt J. 2020;8(2):23-24. DOI: 10.15406/htij.2020.08.00217
Plasma cell leukemia (PCL) is a rare and aggressive entity of malignant plasma cell proliferation that corresponds to 2–4% of plasma cell myeloma (PCM) cases.1,2According to the World Health Organization (WHO), PCL is defined as a disorder in which clonal plasma cells constitute more than 20% of total leukocytes in the blood or their absolute count is more than 2.0x109/L.1,3The bone marrow is usually extensively and diffusely infiltrated. Neoplastic plasma cells are frequently present in extra-medullary sites such as the liver, spleen, body cavity effusions, and spinal fluid.PCL can be classified into: primary (de novo, 60-70% of all PCLs) or secondary which is a leukemic transformation occurring in approximately 1% of previously diagnosed PCMs.4 Patients with PCL have aggressive disease, poor response to therapy, and a relatively short survival.1
A 62-years-old female patient presented to the Hematology department at Alexandria main university hospital suffering from bone pain, fever,and dysuria. Past history and family history were irrelevant. On examination, chest and heart were free and there was no organomegaly (lymphadenopathy, hepatomegaly or splenomegaly). On laboratory evaluation, the complete blood picture revealed a hbmoglobin level of 8.3 g/dL,hematocrit of 25.2%, white blood cell count of 19.51 × 109 /L and platelet count of 114 × 109/L. Morphological examination of peripheral blood smear showed small to medium-sized a typical lymphoplasmacytoid cells (accounting for 85% of the differential WBCs count) with eccentric nuclei and basophilic cytoplasm,(Figure 1A). Bone marrow aspirate examination revealed that 47% of total nucleated marrow cells were atypical lymphoplasmacytoid cells with a morphology similar to those in the peripheral blood (Figure 1B), and 13% were lymphocytes. Granulocytic, erythroid and megakaryocytic lineages were depressed.
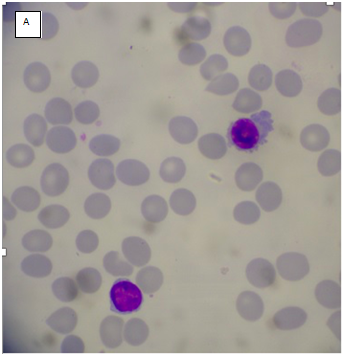
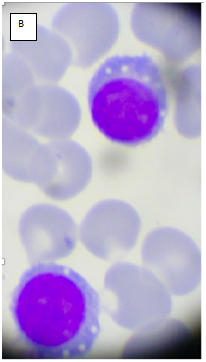
Figure 1 (A)PB smear showing small to medium-sized lymphoplasmacytoid cells with eccentric nucleus and basophilic cytoplasm. (B) BM aspirate showing atypical lymphoplasmacytoid cells with basophilic cytoplasm.
Other laboratory tests showed total serum proteins of 6.2 g/dL, albumin of 3.4 g/dL and a monoclonal band of IgG (lambda) by immunofixation (1.7g/dL). Total serum Calcium was normal (7.9 mg/dL),and renal functions were abnormal with increased blood urea (86 mg/dL) and serum creatinine (2 mg/dL).
Flowcytometeic immunophenotyoing of the bone marrow revealed the presence of clonal plasma cells expressing CD138, CD38, CD56 and Cytoplasmic lambda
light chain and negative for CD19 and Cytoplasmic kappa light chain, reflecting a plasma cell malignancy despite
the morphologic features of lymphoplasmacyticlymphoma(Figure 2). Additionally, immunophenotyping of the peripheral blood was also performed and revealed the presence of clonal plasma cells with the same immunophenotype as the previously identified plasma cells from the bone marrow except that they were CD56 negative(Figure 3). Based on the previous findings, the final diagnosis of the patient was released as plasma cell leukemia.
PCL is a rare disease with median patient age younger than myeloma at diagnosis. The bone marrow is usually extensively infiltrated which leads to bone marrow suppression and high incidence of anemia and thrombocytopenia.2,5,6Neoplastic plasma cells are frequently found in extramedullary sites such as the liver, spleen, body cavity effusions, and spinal fluid.1This appears to be the result of a lower expression of cell adhesion molecules, such as CD56, facilitating the release of leukemic plasma cells from the BM microenvironment.5,7
Our patient had no extramedullary involvement at diagnosis, but she presented with anemia, bone pains and renal affection. Her PB and BM aspirate showed extensive infiltration by lymphoplasmacytoid cells that had similar morphology, which made the differential diagnosis between lymphoplasmacytic lymphoma (LPL) and PCL difficult by morphological analysis alone. Normal plasma cells are CD19+/CD45+/CD38bright/CD56−while neoplastic plasma cells are usually CD19−/CD45−/CD38+ /CD56+.7,8However, in this case plasma cells in BM areCD56 positive, while in PB are CD56 negative.CD56 mediates cell-cell and cell-matrix interactions. So, loss of CD56 expression could accelerate the process of metastatic spread.9,10 The regulation of CD56 is controlled by a very precise mechanism. CD56 can be downregulated during migratory events and re-expressed when the cell reaches a specific site or organ.7This finding is also in accordance with study by Pellat-Deceunynck et al,7who found migrated plasma cells in the peritoneal cavity of multiple myeloma patients. Cells localized in the peritoneal cavity expressed CD56 and have high proliferation activity.7
None.
The author declares no conflict of interest.

©2020 Deghady, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.