eISSN: 2469-2778


Case Report Volume 13 Issue 1
Department of Medical Research, Universidad Francisco Marroquin, Guatemala
Correspondence: Daila Marianne Ismatul, Cabrera Department of Medical Research, Universidad Francisco Marroquin, Guatemala, Tel 58702602
Received: November 15, 2024 | Published: January 21, 2025
Citation: Ismatul DM, Ismatul DI. Multisystem langerhans cell histiocytosis in an infant: a case report. Hematol Transfus Int. 2025;13(1):1‒3. DOI: 10.15406/htij.2025.13.00343
Langerhans cell histiocytosis (LCH) is a rare disorder characterized by abnormal proliferation of Langerhans cells, leading to multisystem involvement, particularly affecting bones, skin, and the central nervous system. While its presentation can be highly variable, diagnosis can be challenging due to its similarity to other conditions such as malignant tumors. Here, we report the case of an 11-month-old female patient with a progressive retro auricular mass, osteolytic bone lesions, and temporal bone involvement. Following biopsy and immunohistochemical analysis, the patient was diagnosed with multisystem LCH. The patient responded well to chemotherapy, showing disease stabilization. This case emphasizes the importance of considering LCH in the differential diagnosis of osteolytic lesions in pediatric patients and highlights the role of early biopsy and imaging in achieving an accurate diagnosis.
Keywords: langerhans cell histiocytosis, retroauricular mass, pediatric, multisystem disease, osteolytic lesions
Langerhans cell histiocytosis (LCH) is a rare clonal disorder characterized by abnormal proliferation of Langerhans cells, a type of dendritic cell involved in immune regulation. Historically classified under "histiocytosis X," which includes eosinophilic granuloma and Hand-Schüller-Christian disease, LCH has an incidence of 2-9 cases per million children annually, but it can also affect adults. Mutations in the MAPK pathway, particularly in BRAF V600E, have been implicated in its pathogenesis. LCH presents with a wide range of clinical manifestations, from isolated organ involvement to multisystem disease affecting vital organs such as the liver and CNS. Diagnostic challenges arise from its variability and potential for aggressive progression, especially in cases of bone or multisystem involvement. While chemotherapy has improved outcomes, long-term complications, such as infections and skeletal deformities, persist. This case report describes an 11-month-old female with multisystem LCH and significant bone involvement, highlighting the complexities of managing this disease.
A previously healthy 11-month-old female presented to the clinic with a progressively enlarging retroauricular mass on the left side, noted by her parents for the past two months. There was no associated lymphadenopathy, and the remaining physical examination was unremarkable. Initial laboratory investigations, including complete blood count and inflammatory markers levels, were within normal limits. Given the persistent nature of the mass, biopsy was performed. Histopathological analysis of the biopsy specimen revealed proliferation of atypical cells. Immunohistochemical staining was inconclusive, and further imaging was warranted to characterize the lesion. A metastatic bone series was ordered, revealing two small osteolytic lesions in the neck and right intertrochanteric region of the femur, measuring 1.28 x 0.53 cm and 0.51 x 0.19 cm, respectively (Figure 1). Based on these findings, a preliminary diagnosis of a malignant process, such as a rhabdoid tumor, was considered.

Figure 1 X-ray images of the patient: Evidence of two small osteolytic lesions in the neck and right intertrochanteric region of the femur, measuring 1.28 x 0.53 cm and 0.51 x 0.19 cm, respectively.
A subsequent CT scan of the brain, complete abdomen, and thorax showed soft tissue lesions that were homogeneous, well defined, and exhibited mild enhancement with contrast, eroding and altering the morphology of the skull cortex without infiltrating the brain parenchyma (Figure 2A & 2B). Additionally, multiple lytic lesions were identified in the sphenoid bone and vertebral bodies of C2, C3, and C5 vertebrae. Thoracic CT revealed lytic lesions in the vertebral bodies of T1, T3, T4, T6, and T7, along with pathological fractures of T5 and T9 (Figure 3A & 3B). Given the extensive bone involvement, the possibility of aggressive systemic disease was considered, including LCH, neuroblastoma, and metastatic rhabdoid tumors. Definitive histopathological examination of the previously biopsied tissue, complemented by immunohistochemistry, confirmed the diagnosis of Langerhans cell histiocytosis (LCH). Immunohistochemical staining was positive for S-100, CD68, PD-L1, and CD1a, which further confirmed the diagnosis. Due to the patient developing bilateral ear discharge, a mastoid CT scan was performed. The scan showed a loss of normal mastoid morphology with bony erosion caused by homogeneous soft tissue lesions bilaterally (right mastoid: 2.9 x 1.8 cm, left mastoid: 3.4 x 2.3 cm) (Figure 4A & 4B). These findings are consistent with the systemic spread of LCH, which affects the temporal bones.
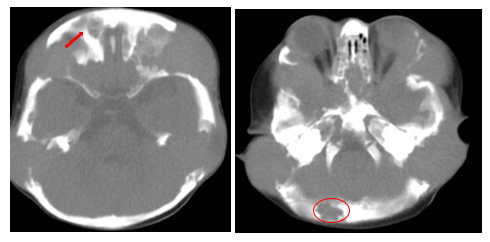
Figure 2A&2B Cerebral CT scan of the patient- Evidence of soft tissue lesions, homogeneous, with well-defined borders, showing mild contrast enhancement in the occipital and frontal regions.
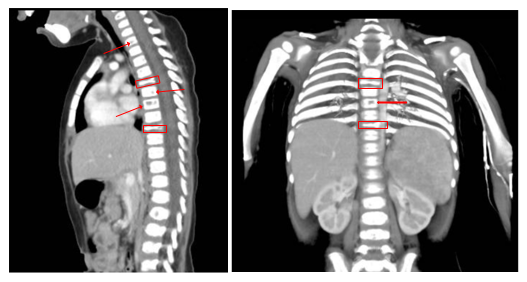
Figure 3A&3B Thoracic CT of the patient revealed lytic lesions in the vertebral bodies of T1, T3, T4, T6, and T7, along with pathological fractures of T5 and T9.
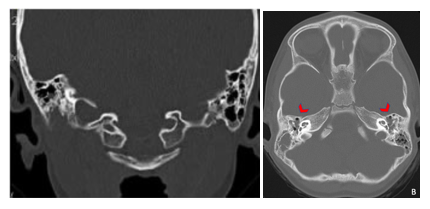
Figure 4A&4B Mastoid CT of the patient revealed total opacification of the remaining mastoid air cells and loss of morphology of both mastoid portions of the temporal bone.
The patient was started on a standard chemotherapy regimen for multisystem LCH, consisting of an induction phase with vinblastine (6 mg/m² intravenously once weekly for 6 weeks) and prednisone (40 mg/m² orally daily for 4 weeks, followed by a gradual taper over 2 weeks). This was followed by a continuation phase with vinblastine (6 mg/m² every 3 weeks) and prednisone (5 days per cycle) for a total duration of 12 months. Initial response to chemotherapy was promising, with stabilization of the disease and improvement in clinical symptoms. However, the patient remains under close surveillance due to recurrent acute otomastoiditis.
Langerhans cell histiocytosis (LCH) is a rare clonal disorder of the monocyte-macrophage system characterized by the accumulation of pathological Langerhans cells. Mutations in the MAPK signaling pathway, particularly the BRAF V600E mutation, are believed to play a crucial role in the etiology of LCH.1 LCH presents with a wide clinical spectrum, ranging from single-organ involvement to aggressive multisystem disease. Bone involvement is common in children, particularly in the skull.2 Diagnosing LCH can be challenging because of its overlap with other conditions such as infectious osteomyelitis or malignancies.3 Radiologically, osteolytic lesions, as seen in this patient, are hallmark features of LCH, but they are not specific. Several conditions must be considered as part of the differential diagnosis. Infectious osteomyelitis, for example, can mimic LCH radiologically and clinically, particularly in the presence of systemic signs of infection. Malignancies such as Ewing sarcoma and leukemia can also present with lytic bone lesions and systemic symptoms, requiring careful evaluation of imaging, laboratory results, and biopsy findings.4
Neuroblastoma, a common pediatric malignancy, often presents with metastatic bone lesions that may appear similar to LCH on imaging. Benign conditions, such as eosinophilic granuloma (a localized form of LCH), must also be differentiated. While eosinophilic granuloma typically presents with solitary or limited lesions, systemic workup is crucial to exclude multisystem disease.5 The definitive diagnosis of LCH relies on histopathological examination, in which the characteristic proliferation of Langerhans cells can be identified. Immunohistochemical staining is essential, with positive staining for CD1a and CD207 (Langerin) confirming the diagnosis. In our case, the initial biopsy findings were suggestive of a proliferative process, and immunohistochemical staining ultimately led a diagnosis of LCH.6 Treatment of LCH varies depending on the extent of the disease. Single-system LCH may be treated with local therapies, whereas multisystem disease generally requires systemic chemotherapy, with vinblastine and corticosteroids being the standard regimens.7 In this case, temporal bone involvement, which can lead to complications, such as chronic otitis media and mastoiditis, underscores the need for close monitoring.8,9
Long-term prognosis of LCH depends largely on the extent of organ involvement at the time of diagnosis and the patient's response to initial treatment. Patients with multisystem LCH, particularly those with involvement of risk organs (liver, spleen, and bone marrow), have a more guarded prognosis. While our patient showed an initial good response to chemotherapy, recurrent otomastoiditis remains a concern, and she continues to be closely monitored for disease recurrence and potential complications.7
Parental consent was obtained for this case report.
None.
The authors declare that there are no conflicts of interest.

©2025 Ismatul, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.