eISSN: 2469-2778


Research Article Volume 1 Issue 4
Clinical Laboratory of Sichuan Academy of Medical Science & Sichuan Provincial People
Correspondence: Mingyong, Clinical Laboratory of Sichuan Academy of Medical Science & Sichuan provincial People’s Hospital, No. 32 West Second Section First Ring Road, Chengdu, Sichuan, China, Tel 86 028-87394056, Fax 86 028-87394056
Received: November 19, 2015 | Published: December 29, 2015
Citation: Zhang J, Mingyong Li, Yuan H. Large population study for age- and gender- related variations of platelet indices in Southwest China healthy adults. Hematol Transfus Int J. 2015;1(4):108-114. DOI: 10.15406/htij.2015.01.00023
Aim: The present data on the evaluation of platelet parameters in Chinese Han population are still limited. This study was to identify age- and sex-specific variations of platelet indices in Southwest China, including platelet count (PLT), mean platelet volume (MPV), platelet distribution width (PDW), plateletcrit (PCT) and platelet-large cell ratio (P-LCR), through a large-scale investigation of healthy people.
Methods: We performed a retrospective analysis on 46872 local healthy individuals (men:n=26,582 and women n=20,290) aged >18yrs. All the subjects were healthy people through the health screening. PLT indices were measured with Sysmex XE-2100 blood cell automatic analyzer. Associations of platelet indices with dependent variables were investigated by ANOVA analysis. Correlation was assessed by the Pearson's correlation coefficient(r). Statistical analyses were performed with SPSS 20.0 software (Chicago, IL) and Excel 2007.
Results: The distribution of platelet count and PCT by age and gender shows a slow, progressive decline with aging in both males and females. On average, a 10-year increase in age corresponds to an average of 6×109/L decrease in platelet count, adjusting for gender (P<0.001). On the contrary, the distribution of MPV, PDW, P-LCR and MPV/PLT ratio by age and gender shows a slow, progressive increasing trend with aging in both genders. The age was negatively correlated with PLT(r=-0.23, P=0.000), PCT(r=-0.24, P=0.000). While age was positively correlated with either MPV (r=0.1, P=0.72), PDW (r=0.1, P=0.024), P-LCR (r=0.09, P=0.002), and MPV/PLT (r=0.21, P=0.001). A positive correlation between MPV and PDW, MPV and P-LCR, PDW and P-LCR was observed, while negative correlation between MPV and PLT, PDW and PLT, P-LCR and PLT was also presented. It’s very interesting that mean PLT in Southwest China Chengdu region was lower than other countries while the MPV, PDW, P-LCR, MPV/PLT values in our study was found to be higher than all other results reported. All of the platelet indices except for MPV showed significantly different distributions from males to females.
Conclusions: These findings suggest that the platelet indices could be greatly influenced in healthy subjects by age and sex. The lower platelet count accompanied with higher MPV, PDW and P-LCR, which were possibly the result of the adaption to the basin environment. Based on these findings, it would be reasonable to conduct formal prospective studies to determine the clinical significance. Further studies should be necessary to make additional verification. Unique reference ranges of some routine inspection items should also be established for people of different ethnic groups or in different regions.
Keywords: platelet count(PLT), mean platelet volume (MPV), platelet distribution width (PDW), plateletcrit (PCT), platelet-large cell ratio (P-LCR)
PLT, platelet count; MPV, mean platelet volume; PDW, platelet distribution width; PCT, plateletcrit; P-LCR, platelet-large cell ration; PT, proficiency test; EDTA, ethylene Di amine tetra acetic acid; ANOVA, analysis of variance; CI, confidence interval
Platelets play a pivotal role in atherothrombosis, the major cause of most unstable coronary syndromes. The clinical utility of newer hematological parameters such as the analyzer-derived PLT indices has been explored in the recent years.1 Mean platelet volume (MPV) and platelet distribution width (PDW) have been reported to be correlated with PLT function and may be more sensitive indices than PLT number as a marker of clinical interest in various disorders such as cardiovascular disease2 and stroke.3 Platelet-large cell ratio (P-LCR), MPV/PLT ratio, when analyzed along with the other PLT parameters, helps in the differential diagnosis of the thrombocytosis related diseases.4 Recent studies have explored the role of plateletcrit (PCT) as independent risk factors of spontaneous echo contrast in patients with mitral stenosis.5 Considering the role of the PLT indices in clinical practice, it is encouraging to research the variations for these newer parameters. However, PLT parameters are influenced by various factors such as age, gender, ethnicity origin, altitude, season and geographic locations6–9 and hence it is important to define the specific reference values. To our knowledge, few studies has yet focused on PCT, P-LCR and MPV/PLT ratio variations in healthy populations according to gender and age. Besides, reports on platelet indices are not univocal, and limited to small population. In our previous work10 studying on 11395 local healthy individuals, we found an interesting phenomenon that MPV in Chengdu plain is obviously higher than other countries. Therefore, our aim of this study was to further explore platelet indices on more large-scale.
In the present study, we performed a retrospective analysis on 46872 local healthy individuals from 2015.01- 09 aged > 18yrs and the mean age of patient group was 41.7 years and male to female ratio was 26582:20290. Every subject underwent a physical examination form. Exclusion criteria included body mass index ≥ 28, high blood pressure (systolic number ≥ 140 mmHg and/or diastolic number ≥ 90 mmHg), hypothyroidism and hyperthyroidism, diabetes, atherosclerosis and vascular disease, cardiopathy, chronic nephropathy, hepato biliary disease, allergic diseases, hematological disease, myopathy, autoimmune disease, burns and muscle trauma, the presence of acute and chronic infection, plasma fasting glucose > 7.0 mmol/l, serum creatinine > 120 μmol /l, serum creatinine kinase > 400 U/l, positive hepatitis B surface antigen, positive anti-hepatitis C virus antibody, positive anti-immunodeficiency virus antibody and positive urinalysis. Platelet values were measured within 2 hrs from blood collection and of K3 salt of ethylene di amine tetra acetic acid (EDTA) anti-coagulated at 8:00 - 9:00 am. All the tests were performed on two XE-2100 (Sysmex, Japan) hematological analyzers. The study population was homogenous for both ethnic origin (Southwest China) and geographic residence and was only studied once. Standardization and assurance of quality control before and after samples testing, three levels of controls (e-CHECK for XE were purchased from Sysmex, Japan) were performed. Dedicated reagents and standard methodologies were used, analyzers were all maintained according to the manufacturer’s instructions during the entire period of the study. Our clinical laboratory have regularly participated in proficiency test (PT) of Chinese Ministry of Health, and has gained accreditation from the Ministry of Public Health. The quality of results was validated by regular internal quality control procedures and participation in an external Quality Assessment scheme.
Statistical analysis
The significance of differences between population groups was assessed by one way analysis of variance (ANOVA). Correlation was assessed by the Pearson’s correlation coefficient(r). Statistical analyses were performed with SPSS20.0 software (Chicago, IL) and Excel 2007. Statistical significance was set at P<0.05. Data were reported as mean and 95% confidence interval (CI).
First, we observed the overall trend of the changes of platelet indices with age and gender. The distribution of platelet count and PCT show a slow, progressive decline with aging in both males and females. On the contrary, all of MPV, PDW, P-LCR, MPV/PLT indices display increasing trend with aging from males to females. Overall, women had significantly more platelets than men (201 vs. 189*109/L, P=0.000) (Figure 1, 2A & B), and platelet count decreased with aging both in males and females (P=0.000). The resulting of age - and sex - related mean platelet values, as well as the correlation analysis was shown in Figure 1-3. The age was negatively correlated with PLT (r = -0.23, P=0.000, Figure 3A), PCT (r = -0.24, P=0.000, Figure 3B). While age was positively correlated with either MPV (r = 0.1, P=0.72, Figure 3C), PDW (r = 0.1, P=0.024, Figure 3D), P-LCR (r = 0.09, P=0.002, Figure 3E), and MPV/PLT (r = 0.21, P=0.001, Figure 3F).
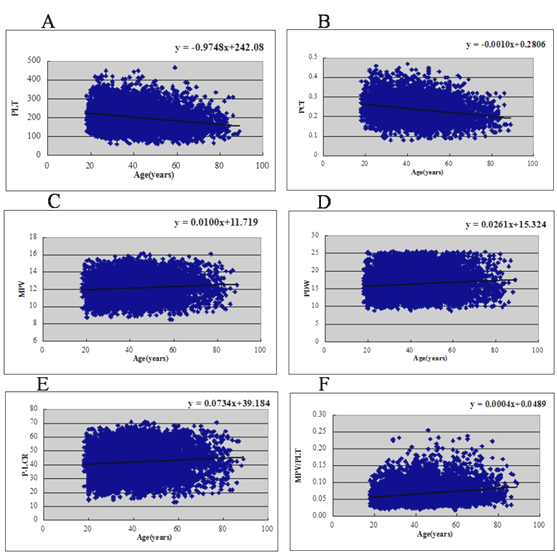
A, B: The PLT count and PCT were negatively correlated with age (r= -0.23, 0.24; P=0.000, 0.000, respectively).
C, D, E, F: MPV, PDW, P-LCR, MPV /PLT were positively correlated with age (r = 0.10, 0.10, 0.09, 0.21; P=0.72, 0.024, 0.002, 0.001).
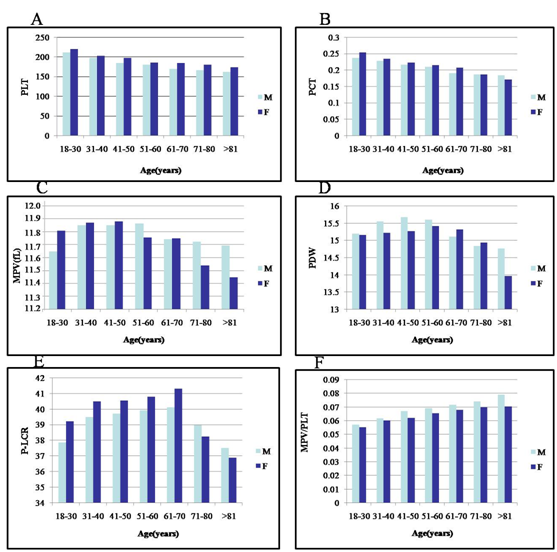
A, B: PLT and PCT by age and gender shows a slow decline with aging.
C: MPV display a increasing trend by age, with a reduction from 51years in female and 61years in male;
D: PDW show a slow increasing trend with aging, with a reduction from 61 years in female and 51 years in male;
E: P-LCR displays an increasing trend with aging and reached peak at 61-70 age class in both males and females.
F: The ratio of MPV/PLT increased with aging all the time.
The large sample size of our study allowed us to investigate narrow age classes, and this approach revealed that age-related changes in platelet counts are very large: the number of platelets in very old age (>81 years) is reduced by 22% in men and by 21% in women with respect to young (18-30 years). The observed age-related trend was common to all other investigated populations. On average, a 10-years increase in age corresponds to an average of 6×109/L decrease in platelet count, adjusting for gender (P<0.001). On the contrary, The distribution of MPV, PDW, P-LCR and MPV/PLT show a slow, progressive increasing trend with aging (Figure 1, 2C, D, E & F), with a reduction from 51 years in female and 61 years in male for MPV (Figure 2C) and from 61 years in female and 51 years in male for PDW (Figure 2D) . Besides, the P-LCR displays an increasing trend with aging and reached peak at 61-70 age class in both males and females (Figure 1, 2E). The ratio of MPV/PLT increased with aging all the time (Figure 1, 2F). Then, we estimated mean values of platelet indices stratifying by seven age classes and gender for individuals over 18 years, as illustrated in Table 1. Mean platelet count varied significantly in different age classes and, adjusting for age and sex, it ranged from 163 to 224*109/L.
Age |
Gender (n) |
PLT(*109) |
PCT (%) |
MPV (fL) |
PDW (%) |
P-LCR (%) |
MPV/PLT |
18-30 |
M(5347) |
209 |
23.29 |
11.65 |
15.24 |
37.85 |
0.0571 |
F(5194) |
224 |
25.17 |
11.81 |
15.22 |
39.20 |
0.0552 |
|
31-40 |
M(6228) |
197 |
22.48 |
11.85 |
15.66 |
39.47 |
0.0618 |
F(5000) |
206 |
23.10 |
11.87 |
15.50 |
40.54 |
0.0603 |
|
41-50 |
M(6824) |
188 |
21.21 |
11.86 |
15.71 |
39.70 |
0.0671 |
F(5094) |
201 |
22.31 |
11.89 |
15.33 |
40.77 |
0.0622 |
|
51-60 |
M(3952) |
183 |
20.66 |
11.87 |
15.65 |
39.91 |
0.0693 |
F(2642) |
190 |
21.19 |
11.76 |
15.41 |
40.78 |
0.0656 |
|
61-70 |
M(2355) |
170 |
19.15 |
11.73 |
15.23 |
40.11 |
0.0716 |
F(1477) |
184 |
21.16 |
11.75 |
15.34 |
41.31 |
0.0679 |
|
71-80 |
M(1446) |
166 |
18.66 |
11.72 |
14.84 |
38.98 |
0.0741 |
F(741) |
180 |
20.54 |
11.55 |
14.93 |
38.23 |
0.0699 |
|
>81 |
M(430) |
163 |
18.31 |
11.69 |
14.73 |
37.51 |
0.0791 |
F(142) |
176 |
19.96 |
11.45 |
13.93 |
36.89 |
0.0671 |
Table 1 Mean values of platelet indices according to age groups and gender
Age- and sex-adjusted ANOVA, performed on the overall sample, showed significant differences among the average platelet count (p=0.000), PCT (p=0.000), MPV (p=0.724), PDW (p=0.024), P-LCR (p=0.002) and MPV/PLT (p=0.000).
Correlation analysis
As shown in Figure 3,4 the PLT count was negatively correlated with MPV (r =- 0.6567, P<0.001, Figure 3A), and PDW (r =- 0.6503, P<0.001, Figure 3B) as well as P-LCR (r =- 0.6526, P<0.001, Figure 2C). While MPV were positively correlated with either PDW (r = 0.7319, P<0.001, Figure 2D) or P-LCR (r = 0.9623, P<0.001, Figure 2E). In addition, PDW was positively correlated with P-LCR (r = 0.6966, P<0.001, Figure 2F).
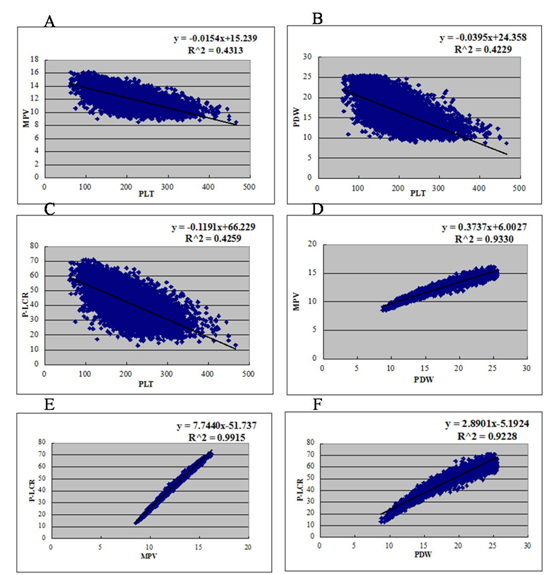
A: The PLT count was negatively correlated with MPV (r =- 0.6567, P<0.001);
B: The PLT count was negatively correlated with PDW (r =- 0.6503, P<0.001);
C: The PLT count was negatively correlated with P-LCR (r =- 0.6526, P<0.001);
D: MPV was positively correlated with PDW (r = 0.7319, P<0.001);
E: MPV was positively correlated with P-LCR(r = 0.9623, P<0.001);
F: PDW was positively correlated with P-LCR (r = 0.6966, P<0.001).
Although a various of studies allowed researchers to realize the distinctive physiological traits of platelet count in different nations and seasons,11–17 as for MPV, PDW, PCT and P-LCR, a limited number of studies are available. In our previous work,10 we observed an interesting phenomenon that the people in Southwest China of Chengdu plain had a lower mean value of PLT count and PCT but a higher MPV value than other populations. This was in agreement with the other observations that were made by other Chinese researchers.18–21 In order to further explore this unique difference and to meet the special requirement for the Sichuan basin on other platelet indices, we performed a much more large-scale retrospective analysis on as many as 46872 local healthy individuals (the largest scale so far reported) aged >18yrs, so as to exclude genetic and environmental factors, which were known to influence platelet indices. The study population was homogenous for both ethnic origin (Han people) and geographic residence. Our results demonstrated that there were age- and gender- related differences in platelet count, MPV, PDW, PCT, P-LCR and MPV/PLT ratio among healthy Chengdu plain adults.
As for platelet count, a limited number of studies are available. Analyses of small groups of healthy subjects initially suggested that platelet count varies by age and sex22 being higher in women than in men and in youth than in old age.23 Larger studies later confirming these findings.24–26 Additionally, significant differences in platelet count have been repeatedly observed in different ethnic populations and mainly attributed to genetic factors,27 which, however, remain largely unknown. In particular, both the lower and the upper limits of the normal range seem to be inappropriate for the Chinese population, especially Southwest Chengdu people.10,18–21 The mean PLT number of people living in Chengdu Plain [(83-268)×109/L] was lower than that of national average level [(125-325)×109/L] (Data was released by Chinese Ministry of Health), which was consistent with the previous finding of Qian Niu.21 This highlighted the necessity and importance of deriving new and region-specific reference ranges for PLT indices. Therefore, our study is divided into 7 age groups, so as to better research the variations details of platelet indices.
The large sample size of our study allowed us to investigate seven narrow age classes, and this approach revealed that age-related changes in platelet counts are very large: the number of platelets in very old age (>81years) is reduced by 22% in men and by 21% in women with respect to young (18-30years). The observed age-related trend was common to all other investigated populations.23–26 On average, a 10-year increase in age corresponds to an average of 6×109/L decrease in platelet count, adjusting for gender (P<0.001). Our results were similar to Biino G’s report on Italian people.25,26 Of note, most of the decrease occurs in 18-40 years (Table 1) for our adults research, comparing to Biino G’s report25 that decrease occurs in childhood and the number of platelets in old age is reduced by 35% in men and by 25% in women with respect to early infancy. As for the old age, our results are similar to Biino G’s25 that only minor decline (Table 1). Concerning the mechanisms that are responsible for the age related changes of reduction may reflect a reduction in hematopoietic stem cell reserve during aging. However, these are only hypotheses. Further investigation is required to identify the mechanisms underlying age-related changes.
Emerging evidence has shown that MPV, which was a measurement of the average size of platelet parameter, but generally overlooked, may be a risk factor of immunity, inflammation and angiogenic diseases.28,29 However, MPV reference ranges are not identical between different regions and populations. The mean of MPV values in our study was found to be 11.84 fL(N=46872), which was higher than all than other reports from abroad to domestic other areas to date, including the recent report from a study conducted by Demirin et al.30 (N=326, mean 8.9fL) in Turkey30 and the results (N=1822, mean 7.7fL) by Lippi et al.31 in Italy, as well as the results from Cho et al.32 (N=7044, mean 8.1fL) in Korea.32 Patients with higher values of MPV may have a higher incidence of arterial occlusive disease. This finding indicates that higher values of MPV may be a useful additional measure in assessing the risk variance of MPV associated clinical diseases. Further studies would be necessary to make additional verification on such possibilities. Since all the samples were analyzed strictly within 2hours, so increase in volume due to storage time was excluded. Our hematological analyzer (XE-2100, Sysmex, Japan) has good accuracy traceability and critical external and internal quality control. So, all of these factors have ensured the accuracy of the results. The cause of these differences is still unknown. While environmental factors and life styles have been suggested to explain the differences,28,29 genetic factors may also play a role.27,33 Besides, the possible influencing factors may also including the special diet habit, climate and the life styles of the basin, which deserve our next exploring work. Compared with the previous three studies, which showed controversy in the MPV change with aging. Our study showed the similar results with Lippi et al.31 and Cho et al.32 that MPV values might be dependent upon the age on the overall trend. However, when stratified by narrow age classes, we found there was a slight decline after 51years old in both genders (Figure 2C). Our results are quite agree with Jiang Hong’s.19
Platelet distribution width (PDW) is an indicator of variation in platelet size, reflecting the heterogeneity of platelets. MPV and PDW are widely and routinely used in clinical practice worldwide. Higher MPV and increased PDW have been found in some diseases.28 However, the distribution of these parameters in healthy adults have rarely been investigated. P-LCR is the proportion of large platelets. Generally, the more large platelets exist in blood, the higher MPV and PDW are. Our results indicated that the Southwest Chinese adults had higher P-LCR and PDW, which were in accord with the change of MPV. The correlation analysis verified that all of MPV, PDW, and P-LCR were all positively correlate with aging respectively. When stratified by narrow age classes, we found there was a slight decline from 61years in female and 51years in male for PDW (Figure 2D). Besides, the P-LCR displays an increasing trend with aging and reached peak at 61-70 age class in both males and females (Figure 1 & 2E). The ratio of MPV/PLT increased with aging all the time (Figure 1) (Figure 2F). All of these results are also consistent with Jiang Hong’s.19 However, the reasons are still unknown, maybe it is related to hormone levels fluctuation.
Another important finding of our study concerns gender-related differences in platelet count, MPV, PDW, PCT and P-LCR. Our research found that only MPV values seemed to have little association with gender while the other platelet count, PCT, PDW, P-LCR and the ratio of MPV/PLT showed significantly different distribution from males to females. Similarly to the age-related variability, the mechanisms responsible for sex-related differences are also unknown. Kadikoylu et al.34 have reported that the reduction of body iron in women is probably related to the higher platelet count for the iron deficiency may stimulate platelets production. In addition, the hormonal differences between men and women, could also be involved. In particular, in-vitro and in-vivo findings showed that estrogens favour platelets formation in mouse35 but no data in humans are available. Maybe the hormonal differences between men and women, which become larger after puberty, could be affected. Considering the clinically practical significance and convenience, the reference ranges of platelet indices regardless of gender were still widely used. However, our study can help clinicians to realize the different reference values in age and gender when diagnosis of platelet related diseases, though the clinical utility of platelet indices remains uncertain, despite a variety of papers suggesting possible useful correlations.
To our knowledge, this is the first report to explore the age- and gender- related differences in PLT indices in healthy individuals on so large-scale. The lower platelet count accompanied with higher MPV, PDW and P-LCR, which were possibly the result of the adaption to the basin environment. The phenomenon was worth further research. Unique reference ranges of some routine inspection items should also be established for people of different ethnic groups or in different regions.
None.
The author declares no conflict of interest.

©2015 Zhang, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.