eISSN: 2469-2778


Case Report Volume 10 Issue 1
Servicio de Hematología y hemoterapia- Unidad de trombosis y hemostasia. Complexo Hospitalario Universitario de Ourense
Correspondence: Picallo Lombardía P, Servicio de Hematología y hemoterapia- Unidad de trombosis y hemostasia. Complexo Hospitalario Universitario de Ourense, Spain
Received: October 01, 2021 | Published: January 10, 2022
Citation: Lombardía PP, Sanchez PM, Caneiro AM, et al. Incidental thrombosis in oncologic patient. Hematol Transfus Int J. 2022;10(1):1-3. DOI: 10.15406/htij.2022.10.00271
We present a 64 year-old woman case report with lung cancer and active chemotherapy treatment, who developed a Superior Vena Cava Syndrome (SVCS). During the follow up, being with anticoagulant therapy, she presented an incidental thrombosis. This event was discovered at control doppler image of previous SVCS. All hemostasia studies were normal.
Anticoagulant therapies in Oncological and Hematological patients are essential and needed. Some issues such as prophylactic and treatment of thrombotic diseases will be discussed, also when and which should be used.
Keywords: thrombosis, oncology, incidental, anticoagulant therapy
64 year-old woman, smoker since teenage diagnosed in 2017 of squamous right lung cancer, stage IIIb. She received radiotherapy and chemotherapy (Vinorelbine-cisplatine), finished at December 2017, achieving partial response. In March 2018 she started Durvalumab 10 mg per Kilogram every two weeks during twelve months.
She went to emergency department a month after finishing Durvalumab because of purplish face and edema. Also she had problems with swallowing. No fever nor other symptomatology appeared. Blood tests and X ray were done (Table 1). Ten days before, subcutaneous device for treatment was implanted. Chest X-ray control was normal (Figure 1).
|
Clinical manifestation |
Lab tests |
Image studies |
Treatment |
Time |
|
Purplish Face |
Blood tests |
CT Scan |
LWMH 80/mg 24 hr |
Emergency Room |
|
Facial Edema |
D-dimer |
X Ray |
||
|
Swallow difficulty |
Thrombophilia Study |
EKG |
||
|
Cianosis |
Control CT Scan |
Tinzaparin 10,000 UI/24 hr |
24 hr late |
|
|
Collateral Circulation |
Control CT Scan |
3 months later during a year |
||
|
Yugular Ingurgitation |
Doppler image |
6 months later |
||
|
AVK Treatment |
2019 undefined |
Table 1 Clinical, diagnosis and laboratory findings
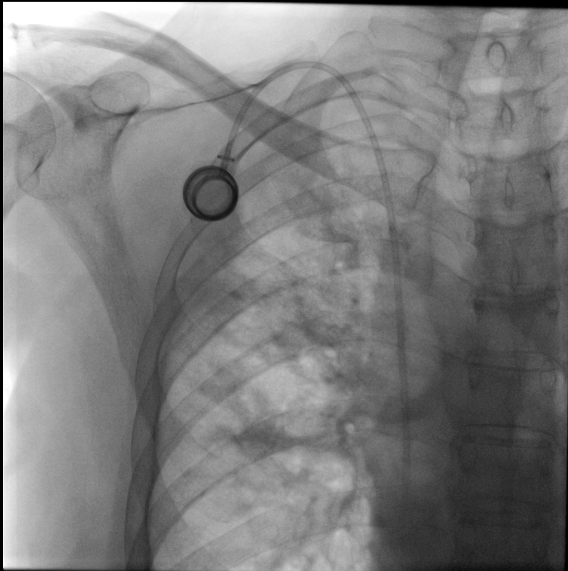
Figure 1 Chest X-ray control after implant of subcutaneous device. No radiological changes or patologic signs were present.
Physical examination was done. Patient was stable, without fever or any other symptoms. Facial and chest cyanosis appeared. Collateral circulation and jugular ingurgitation were present. No other signs of thrombosis were present. All pulses were symmetric. Control blood tests were normal, including D-Dymer.
She was admitted to Oncology service, where a scan was done. It revealed a filling defect at left subclavia vein suggestive of thrombosis (Figure 2). Subcutaneous device was withdrawal. We started anticoagulant therapy with subcutaneous Tinzaparin 10,000 UI, every 24 hours. Three months later, a new control scan was done: collateral circulation was still present.
Thrombophilia studies revealed Hyperhomocysteinemia of 17.2 μmol/L (normal values 3.0 - 15.0), Total Protein S 54.1 % (normal values 65.0 - 140.0), and weak positiveness of a lupic anticoagulant. Six months after the episode, all parameters were normalized. Doppler ecography was done, in which an incidental jugular vein thrombosis was discovered (Figure 3 & 4).
She was followed up at Hematology service three months after the starting event. After a year of anticoagulant therapy (therapeutic dose) with Tinzaparin, without any new thrombotic episode, we explained to patient undefined anticoagulant therapy was necessary. Treatment with Rivaroxaban 20 mg per day was started in December 2019. Now a days, cancer activity remains stable, and no other thrombotic episodes appeared.
Oncologic patients have more risk of thrombosis, with or without chemotherapy, (4.5% -6.1% higher than han patients without malignant disease). This risk is higher in case of metastasis, first three months since diagnosis and also at hematologic malignancies.1
These thrombotic events are the second death cause after their own disease.2 Usually, thrombosis is asymptomatic (around 5%), being more common in big veins, such as inferior cava, or lung embolism.3 Metastatic patients have 28% of these events. Lot of factors help to trigger thrombosis in oncological patients, such as age, high weight, or another related directly to cancer or treatment.
Neoplastic cells have a prothrombotic effect, produced by some mechanisms that participate at the coagulation cascade. They can appearin such a numerous ways. Bleeding, thrombosis, or disseminated intravascular coagulation (DIC) are some examples. Using of systemic chemotherapy, haematopoyesis stimulation, or venous devices increase notoriously thrombotic risk.
Evidence also supports there are some genetic mutations related to oncogenes activation and hemostasia control, such as RAS or p53.4 Cancer location also plays a role in deep vein thrombosis (DVP). Pancreas, brain, stomach or ovaries have 10% more risk of DVP than prostate cáncer.5 Highest incidence of thrombosis belongs to Pancreatic cancer, being between 17% and 57%.6 Related to lung cancer, incidence reaches 13.9%.4
Venous devices are widely used in oncohematology. Almost 4% of thrombosis are caused by these objects.
Thrombosis events secondary to these devices force to withdrawal the device if it does not work because of thrombosis or if any infection sign is present.7
There are lots of treatment strategies for oncologic patients with thrombotic events, based on use of low molecular weight heparin (LMWH), pentasacarid (Fondaparinux) or oral anticoagulants, always individualizing each patient and situation.8
Several studies have shown similar ratios of mortality to symptomatic Venous Thrombotic Event (VTE).9 This is why it is important to treat these events like a symptomatic one. LMWH is usually chosen when a long-term treatment is required, at least 6 first months.
One randomized study of 900 patients with oncologic neoplasms compared treatment of Tinzaparin (treatment dose) during 6 months, with Tinzaparin 10 days followed by Warfarin. VTE incidence decreases 10% on Warfarin group, and 6.9% on Tinzaparin group (Hazard Ratio, 0,65, 95% CI, 0,411,03; p=0,07 ). Bleeding was significantly lower on Tinzaparin-treated patients.10 Anti-vitamin K therapy could be useful in case of no availability of LMWH or Oral Anticoagulants.
So, prevention of VTE must be done in oncologic patients?
It is mandatory to do thrombotic prophylaxis in patients at Hospital. However, several studies have shown that, in ambulatory patients, it is important to individualize the risk. Thrombotic profilaxis is not recommended in ambulatory patients.4 Otherwise, we should individualize each case, prophylaxis on the thrombotic risk (cancer location, etc). There are many stratification scales for this patients. Several guidelines (NCCN guidelines, American Society of Clinical Oncology), recommend Khorana model to predict thrombotic risk in these type of patients.8–10
We can clonclude, supported by literature, anticoagulation therapy in oncological patients should be adjusted to patient profile and should be revaluated periodically by specialized professionals.
None.
The authors declare no conflicts of interest.
None.

©2022 Lombardía, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.