eISSN: 2469-2778


Case Report Volume 5 Issue 1
Hospital de la Vega Lorenzo Guirao, Spain
Correspondence: Santiago Nieto Fernandez, Hospital de la Vega Lorenzo Guirao, CTRA. ABARAN S/N 30530 CIEZA, Spain, Tel 34 627641086
Received: September 26, 2016 | Published: July 12, 2017
Citation: Fernandez SN. IgG4-AIP and APS. Hematol Transfus Int J. 2017;5(1):170-172. DOI: 10.15406/htij.2017.05.00106
Our case unique in the literature involves incidental venous splenic infarction by APS, with sub-capsular hemorrhage without solution of continuity with pancreas, as antigenic trigger and possible IgG4 related disease perpetuating.
Keywords: anti-phospholipid syndrome, NIDDM, thrombocytopenia, RAEB-1, IgG4
Male in Sept. 2009 (58 years), debuts 13,000 platelets/µL associating 13.5 cm domed splenomegaly without focal lesions after routine analysis for controlling NIDDM. Serological studies and autoimmunity were negative. Prolonged exposure to asbestos led to bone marrow biopsy, reporting myelodysplastic syndrome (presence of 3% blasts and absence of lymphoid infiltration). The histopathological and immuno-phenotypic study suggests RAEB-1. Given the absence of bleeding diathesis and other symptoms, only close observation was recommended.
Diagnosis
Anti-phospholipid syndrome (APS) with complete thrombosis of splenic vein. Left-sided hypertension with gastric fundus varices and splenic cavernoma.1,2 After 2 episodes of upper gastrointestinal bleeding (January and October 2014), APS serological triple positivity is confirmed in November 2014 (IgM-ACA 29, IgG-ACA 70 AEU; Beta2-GPI IgG antibodies and LAC very positive) associating mild to moderate thrombocytopenia, splenomegaly 15cm, high MPV, and no mutation JAK2V617F.3–6 In early 2015 APS is confirmed by CT and MR angiography (lack criteria for SLE): complete thrombosis of splenic vein (spleen 16cm)+splenic artery vasculitis. MRI: Superior mesenteric venous thrombosis after suspension of heparin by acute gastrointestinal bleeding. PET-CT 14/08/2015: metabolic increase pancreatic tail mass/splenic hilum 5x6cm, SUV max 2.8.7–9
Organ-A partial pancreatectomy: Autoimmune pancreatitis (AIP) lympho-plasmocytic SCLEROSING ASSOCIATED PLASMA IgG4 (IgG4 AIP), in development since December 2014, after splenic infarction complicated with subcapsular haemorrhage without interruption to tail of the pancreas. Pre-surgery: Quotient CD4/CD8 usual. Post-surgical: Serum IgG4 serial 194mg/dl(1-135), with 0.06% CD19+CD27+Plasmablasts CD38++CD20-(1750/ML). CD4/CD8 ratio 0.7 (decreased by increasing lymphocytes T SUP. CD3+CD8/CD45 +).
Pathological diagnosis (pancreatic tumour mass 5x3.3cm) splenectomy plus body and tail pancreatectomy
The surgical specimen referred corresponds to the body and tail of the pancreas with a spleen in which the identified tumour formation corresponds to a mesenchymal proliferation of partially hyalinized fibrous stroma. Areas of cell proliferation with areas of storiform pattern are observed.10,11 The cells are spindle-shaped of eosinophil cytoplasm without atypia, without mitosis, and in which some area of necrosis is focally observed. In the middle of the stromal component there is a moderate inflammatory in filtrate of chronic predominance (lympho-plasmocytic) that is accompanied by some eosinophils.
Description
The surgical margin that would have continuity with the body of the pancreas is painted blue. At the cut the spleen presents numerous areas of splenic infarction as a whitish nodule of dimensions varying between 5 and 10mm. In adjacent adipose tissue between the pancreas and the spleen, whitish tumor formation of 5x4cm fibrous appearance is identified which, without infiltrating, protrudes into the spleen. The perimeter margin is painted.
Microscopic description
After inclusion in paraffin of the material sent for intraoperative, the absence of malignancy is confirmed in both intraoperative n.1 and intraoperative n.2. The surgical specimen referred corresponds to the body and tail of the pancreas with a spleen in which the identified tumor formation corresponds to a mesenchymal proliferation of partially hyalinized fibrous stroma. Areas of cell proliferation with areas of storiform pattern are observed. The cells are spindle-shaped of eosinophil cytoplasm without atypia, without mitosis, and in which some area of necrosis is focally observed. In the middle of the stromal component there is a moderate inflammatory infiltrate of chronic predominance (lympho-plasmocytic) that is accompanied by some eosinophils.
Inflammatory lesions of the venous vascular component (phlebitis), some of obliterated-obstructive type with chronic and acute involvement of the wall and the endothelial portion that are also affected by the eosinophil component, are observed. The mass extends to the spleen that shows infarct areas. An immune-histochemical study showing positivity of the mesenchymal component for CD-31, Vimentin, smooth muscle actin and focally for CD-31 has been performed. The presence of numerous IgG 4 positive plasma cells is also observed. There is also focal positivity for Cytokeratin AE1/AE3 and BCL2. The immune-histochemical study is negative for CD34, MDM2, CD117, Desmin, Calretinin, HMB45, S100 protein, Cytokeratin 5-6, Thrombomodulin, NCL-2-1, ALK.12–14 Histochemical techniques are performed showing the presence of fibrosis areas and there is no deposit of amyloid-type material in red Congo (Figures 1–3).
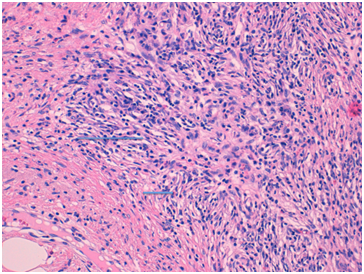
Figure 1 Discard pancreatic carcinoma (Two fragments of 1.5 and 0.8cm of greater dimension are received without evidence of malignancy in any of them).
Treatment
Apixaban 10 mg daily since October 2015 (500,000 Platelets/µL), and in 20months has not been objectified any new thrombo-haemorrhagic episode. May 2016:1st hyperthyroidism and Eco neck: Left thyroid micro-nodule (5mm) only associated with multiple lateral cervical<1cm with lymph benignity criteria. Hashimoto's thyroiditis is diagnosed in the euthyroid phase with likely previous hashitoxicosis. We maintain intensive, active observation pending plasmablastic control.
Assumptions physiopathology immuno-allergic: Late APS diagnosis, causes a bleeding subcapsular splenic infarct uninterruptedly to pancreatic tail, which acts antigenic trigger and triggers immune activation first cell helper Th2, and later of regulatory T cells (Treg) with over-expression Interleukins 4, 5, 10 and 13, along with TGF-Beta. This leads to eosinophilia, elevated IgE and IgG4 and fibrosis progression characteristic IgG4 related disease. Picture: inflammatory pseudo-tumour and A.P: storiform fibrosis, obliterated phlebitis and plasma cell infiltration IgG4 (Figure 4).
The AIP-IgG4 is classified in the IgG4 related new disease entity that may further include retroperitoneal fibrosis, cholangitis, nephritis, sialadenitis, dacryoadenitis, thyroiditis. Our case unique in the literature involves incidental venous splenic infarction by APS, with subcapsular haemorrhage without solution of continuity with pancreas, as antigenic trigger and possible IgG4 related disease perpetuating. Differential Diagnosis remains incipient confirm hyperthyroidism: autoimmune thyroiditis or Hashimoto related IgG4 type. Initial treatment with methimazole.
None.
The author declares no conflict of interest.

©2017 Fernandez. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.