eISSN: 2469-2778


Research Article Volume 4 Issue 1
1Department of Clinical and Chemical Pathology, Beni-Suef University, Egypt
2Department of Clinical Oncology, Cairo University, Egypt
Correspondence: Shereen Mohamed Elhoseiny, Assistant Professor of Clinical and Chemical Pathology, Beni Suef Teaching Hospital, Faculty of Medicine Beni Suef University, Egypt, Tel 002-01005256182
Received: January 19, 2017 | Published: January 31, 2017
Citation: Elhoseiny MS, Abdelfattah MR, Gendy OES. Hypoxia-inducible factor 1 alpha (HIF-1 ? ) and its prognostic value in acute myeloid leukemia. Hematol Transfus Int J. 2017;4(1):19-25. DOI: 10.15406/htij.2017.04.00073
Background: Bone marrow microenvironment which is the principal site of acute myeloid leukemia (AML) initiation and expansion is characterized by hypoxia. The major mediator of hypoxic responses is hypoxia-inducible factor-1alpha (HIF-1α). Hypoxic tumors are resistant to radiotherapy and chemotherapy and are associated with poor prognosis.
Patients and methods: We investigated the expression level of HIF-1α mRNA in 60 de novo AML patients, together with 20 healthy controls using a Real-Time Quantitative Reverse-Transcriptase Polymerase Chain Reaction (RTQ-PCR) aiming of determining its relation to clinical features and laboratory findings at diagnosis and its impact on patients' outcome.
Results: HIF-1α mRNA expression level was significantly higher in AML patients than in controls (p=˂0.001). Higher levels of HIF-1α was found in patients with extra medullary infiltrations (HSM and LNs enlargement) (p<0.001). HIF-1α mean expression level was significantly higher in patients who didn't achieve CR (11.55±4.74) compared to (3.0±1.78) in CR patients, the difference was highly statistically significant (p<0.001). Higher HIF-1α levels were associated with shorter overall survival (OS) and both poorer disease free survival (DFS) and event free survival (EFS) (p<0.001).
Conclusion: HIF-1α is over expressed in AML patients; its level might serve as an early indicator for extra medullary infiltration and disease progression. HIF-1α might be used as a valuable new marker for poor prognosis and treatment resistance in AML patient; therefore, anti HIF-1α might represent a novel therapeutic approach for treatment of AML patients.
Keywords: HIF-1α, hypoxia, normoxia, heterodimer, idarubicin
AML, acute myeloid leukemia; RTQ-PCR, real-time quantitative reverse-transcriptase polymerase chain reaction; OS, overall survival; EFS, event free survival; DFS, disease free survival; BM, bone marrow; HREs, hypoxia-response elements; MPO, myeloperoxidase; SBB, sudan black B; IPT, immune phenol typing; CR, complete remission; GAPDH, glyceraldehyde -3-phosphate dehydrogenase; MNCs, mononuclear cells; PB, peripheral blood
Acute myeloid leukemia (AML) is an aggressive immature hematologic neoplasm which carries poor prognosis. AML therapy results in high initial response rates, associated with the elimination of leukemia cells, but with a high relapse rate.1 Multiple factors influencing treatment response, these factors include patient's age, clinical and hematologic conditions, molecular, cytogenetic features and cytotoxic treatments.2 Bone marrow (BM) microenvironment, the principal site of AML initiation and expansion, is characterized by low oxygen tension with mean oxygen partial pressure (40-50mmHg) and oxygen saturations (80-87%) lower than the arterial blood.3,4 Acute leukemic progression within the BM is associated with further decreases in marrow oxygenation and expansion of hypoxic BM areas.5 Cellular adaptation to hypoxia involves numerous mechanisms; the major mediator of hypoxic responses in both normal and malignant cells is hypoxia-inducible factor-1 alpha (HIF-1α), a member of the basic Helix-Loop-Helix transcription factor family.6 Under normal oxygen tension (normoxia), cytoplasmic HIF-1α protein remains low due to rapid degradation; but under hypoxia, hypoxia allows HIFs to escape from normoxia-mediated degradation in the cytoplasm and to trans locate to the nucleus.7 The stabilized HIF-1α protein trans locates into the nucleus forms a heterodimer with HIF-1β and modulates the expression of hundreds of genes through binding to DNA sequences, called hypoxia-response elements (HREs), within the regulatory regions of target genes.7,8 These HIF-1-targeted genes help the cell adapt to hypoxia by controlling different processes such as erythropoiesis, angiogenesis, cell metabolism, cell cycle, growth, apoptosis and differentiation.9,10
Hypoxic HIF activity is controlled mainly through post-translational modification and stabilization of HIF1α and HIF2α subunits, so that HIF-1α protein levels and HIF transcriptional activity increase as cells become more hypoxic.11 HIF-1α has been shown to contribute to the pathogenesis and progression of multiple kinds of diseases and cancer.9,10 It is commonly over-expressed in many types of tumors.12,13 HIF-1α is over expressed in leukemic blasts in the BM of acute lymphoblastic leukemia (ALL),14 AML15,16 and in chronic myeloid leukemia (CML).17 High levels of HIF-1α expression in primary cancer samples have been associated with poor prognosis, chemotherapy resistance and more aggressive tumor phenotype in multiple solid tumor types.18,19 Similar to solid tumor cells, it has been shown that molecular and biologic adaptations by AML cells to hypoxia also confer resistance to chemotherapy. Over expression of HIF-1α in primary ALL and AML correlated with poor chemotherapy outcomes.15,20 Hypoxic tumors are resistant to radiotherapy and chemotherapy and are associated with poor prognosis, suggesting hypoxia itself could be a therapeutic target.21,22 To our knowledge, the HIF-1α gene has never been studied in Egyptian AML patients. So, this study was done to investigate the expression level of hypoxia-inducible factor-1 alpha (HIF-1α) mRNA in 60 de novo acute myeloid leukemia (AML) patients, with a specific aim of determining its relation to clinical features and laboratory findings at diagnosis and its impact on the response to therapy.
Patients
The current study was conducted on 60 adult AML patients, together with 20 age and sex matched healthy controls. Both Patients and controls were recruited from the National Cancer Institute (NCI), Cairo University and Beni Suef University Hospital after taking their informed contest. Ethical considerations were done according to the Declaration of Helsinki of Bioethics (2008) [23]. AML was diagnosed according to morphologic findings from Giemsa-stained smears of BM aspirates; cytochemical stains criteria such as positivity of myeloperoxidase (MPO) and Sudan black B (SBB) and immune phenol typing (IPT) criteria as positivity of CD13 and CD33 by flow cytometry.
Therapy
Patients were treated according to the standard AML protocol of the National Cancer Institute (NCI), Cairo University. All patients received induction chemotherapy 7-3 protocol which consist of Idarubicin 12mg/m² short infusion on day 1, 2 and 3; Ara-C 100mg/m² continuous infusion 24 hours from day 1 through 7. If the patient didn't achieve complete remission (CR), this protocol was repeated. In case of complete response, patients were shifted to high dose Ara-C 3gm/m² every 12 hours’ days 1, 3 and 5 for 3 cycles.
Assessment of patients’ response to therapy
Remission status was assessed after completion of induction chemotherapy (28 days). Complete remission (CR) was defined as: granulocyte count of at least 1.5x109/L, platelet count of at least 100x109/L, no PB blasts, BM cellularity of at least 20% with maturation of all cell lines and less than 5% blasts and no extra medullary leukemia. Relapse was defined as reappearance of PB blasts, more than 5% blasts in BM, or appearance of extra medullary manifestations after CR was achieved. Overall survival (OS) was measured from the protocol on-study date until the date of death regardless of cause, censoring for patients alive at last follow-up. Disease-free survival (DFS) was defined only for those patients achieving a CR. It was measured from the CR date until date of relapse or death, regardless of cause, censoring for patients alive at last follow-up. Event-free survival (EFS) was defined for those achieving CR as the time from on-study until relapse or death regardless of cause, censoring for those alive at last follow-up. If a patient did not achieve CR but expired within 2 months of the on-study date, then EFS was defined as the time from on-study until death, regardless of cause.24
Methods
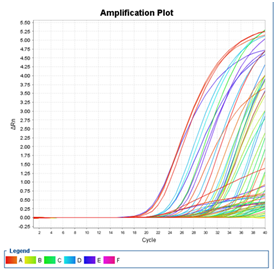
RNA isolation and Real-Time Quantitative Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR): Mononuclear cells (MNCs) were isolated from peripheral blood (PB) or BM aspirate by ficoll density gradient centrifugation at diagnosis before starting treatment. Follow up of patients was carried out for 2 years. Total RNA was extracted from MNCs using a QIA amp® RNA Blood Mini Kits (Catalog No. 52304), (Qiagen, Germany) according to the manufacturer's instructions. Complementary DNA (cDNA) was synthesized using (dt) 15-mer primer by Superscript III Reverse Transcriptase using High-Capacity cDNA Archieve Kit, Applied Biosystems (Part No. 4322171) and stored at -20°C till use. The mRNA expression levels of theHIF-1α gene and its housekeeping gene glyceraldehyde -3-phosphate dehydrogenase (GAPDH) were measured by quantitative RT-PCR using an ABI PRISM 7000 Sequence Detector System (Applied Biosystems, Foster City, CA). The quantitative RT-PCR amplification was performed using the pre-developed Assays-on –demand Gene Expression Set forHIF-1α (Assay ID: Hs00153153_m1, Part no. 4331182, Applied Biosystems) and TaqMan GAPDH control reagents (Applied Biosystems, TaqMan GAPDH control reagents (human) Part no.402869) in combination with the TaqMan Universal PCR Master Mix (Catalog no. 4440043, Applied Biosystems). RTQ-PCR assays were performed for HIF-1α and GAPDH in the same tube in a final reaction volume of 25ul containing 5ul cDNA. The reaction protocol used involved heating for 2 min at 50°C and 10 min at 95°C, followed by 40 PCR cycles of amplification (15 sec at 95°C and 1 min at 60°C). Analysis was performed using ABI PRISM 7000 Sequence Detection Software (Applied Biosystems) and Applied Biosystem Step OneTM Instrument (USA). The expression levels ofHIF-1α gene in tested samples were expressed in the form of CT (cycle threshold) level then Normalized copy number (Relative quantitation) was calculated using the ΔΔCT equation, Relative Quantification(RQ) =2-∆∆CT. A negative control without template was included in each experiment (Figure 1).
Statistical Methods: Data were analyzed using IBM SPSS advanced statistics version 22 (SPSS Inc., Chicago, IL). Numerical data were expressed as mean and standard deviation or median and range. Qualitative data were expressed as frequency and percentage. Chi-square test was used to examine the relation between qualitative variables. For not normally distributed quantitative data, comparison between two groups was done using Mann-Whitney test (non-parametric t-test). Comparison between 3 groups was done using Kruskal-Wallis test (non-parametric ANOVA). Spearman-rho method was used to test correlation between numerical variables. Univariate survival analysis was done using Kaplan-Meier method and comparison between two survival curves was done using log-rank test and Cox-regression analysis for numeric variables. Multivariate analysis was done using Cox-regression method for the significant factors affecting survival on univariate analysis. Hazard ratio (HR) with it 95% confidence interval (CI) were used for risk estimation. All tests were two-tailed. A p-value <0.05 was considered significant.
The current study was conducted on 60 de novo AML patients and 20 healthy controls. There was a highly statistically significant difference between HIF-1α mRNA gene expression level between AML patients and controls (p˂0.001).The mean expression level of HIF-1 α was 5.56± 4.93(range 1.28-19.52) and median 3.69 in AML patients, while it was of mean 0.16±0.10 (range 0.04-0.34) and median 0.14 in controls Table 1 shows AML patients characteristics.
Characteristic |
Value |
HIF-1α expression Level |
5.56± 4.93(1.28-19.52)* |
Median |
3.69 |
Gender: No (%) |
|
Male |
26 (43.3%) |
Female |
34 (56.7%) |
Age at diagnosis: (years) |
46.2±14.2 (19-76) |
Median |
48 |
Total leukocytic count x109/L |
60.6±77.6 (0.8-327.0) |
Median |
28.8 |
Hemoglobin gm/dl |
7.8±1.8(5.5-11.2) |
Median |
8 |
Platelets x109/L |
58.1±59.2(14-320) |
Median |
39.5 |
Bone Marrow blasts |
69.9±19.4(27-100)* |
Median |
74.5 |
Hepato splenomegaly (%) |
22 cases (36.7%) |
LN enlargement (%) |
10 cases (16.7%) |
FAB classification |
|
M0: No (%) |
3(5.0%) |
M1: No (%) |
17(28.3 %) |
M2: No (%) |
25 (41.7 %) |
M4: No (%) |
8(13.3 %) |
M5: No (%) |
5(8.3 %) |
M6: No (%) |
2 (3.3 %) |
Table 1 AML patients characteristics
*Mean ± SD (range); FAB classification: French American British classification
Follow up of AML patients
After 28 days of induction therapy; 42/60 (70%) of AML patients achieved CR, while 18/60 (30%) patients didn't achieve CR. Follow up of patients was carried out for 2 years. At the end of our study, 40/60 (66.7%) patients were alive, while 20/60 (33.3%) patients were dead with cumulative survival at 24 months 61.3% for OS. Cumulative survival at 24 months for disease free survival (DFS) was 67.2% and 46.8% for event free survival (EFS) (Table 2).
Characteristic |
Value |
Follow up time( months) |
20.34±9.14(3.55-38.09)* |
Median |
20.51 |
Complete Remission (CR): No (%) |
42 (70%) |
No CR: No (%) |
18 (30%) |
Overall Survival (OS) |
|
Alive: No (%) |
40 (66.7%) |
Dead: No (%) |
20 (33.3%) |
Cumulative survival at 2 years (24 months): % |
61.30% |
Disease Free Survival (DFS): of the 42 CR patients |
|
Relapse and/or Death: No (%) |
15 (35.7%) |
No Relapse or Death (Alive Free): No (%) |
27 (64.3%) |
Cumulative survival at 2 years (24 months): % |
67.20% |
Event Free Survival (EFS) |
|
CR: (Alive free; no relapse or death) No (%) |
27(45%) |
No CR, Relapse and/or Death: No (%) |
33(55%) |
Cumulative survival 2 years (24 months): % |
46.80% |
Table 2 Follow up of the 60 AML patients
*Mean ± SD (range)
Impact of HIF-1α Gene Expression on AML patients
There was a positive correlation between HIF-1α gene expression level and hepato splenomegaly (HSM). Mean expression level of HIF-1α was higher in patients with HSM (9.56±4.92) than those without HSM (3.24±3.15). The difference was highly statistically significant (p<0.001). Also patients with lymph nodes (LNs) enlargement showed a higher mean expression level for HIF-1α gene (13.64±4.92) than those without LNs enlargement (3.95±3.14). The difference was highly statistically significant (p<0.001). When follow up of AML patient s was considered; patients who didn't achieve CR showed higher mean expression level for HIF-1α gene (11.55±4.74) than those patients achieving CR (3.00±1.78). Again, the difference was highly statistically significant (p<0.001) (Table 3). We didn't find any correlation between HIF-1α gene expression level and other patients clinical or laboratory (p>0.05).
Characteristic |
HIF1-α Expression |
P value |
||
Mean ± SD |
Range |
Median |
||
Gender: No (%) |
||||
Male: 26 (43.3%) |
6.29±4.89 |
1.39-18.43 |
5.34 |
0.116 |
Female: 34 (56.7%) |
5.00±4.95 |
1.28-19.52 |
2.35 |
|
Hepato splenomegaly |
||||
Positive (22 cases 36.7%) |
9.56±4.92 |
3.68-19.52 |
7.42 |
<0.001 |
Negative (38 cases 63.3%) |
3.24±3.15 |
1.28-16.53 |
2.13 |
|
LN enlargement |
||||
Positive (10 cases 16.7%) |
13.64±4.92 |
7.19-19.52 |
13.92 |
<0.001 |
Negative (50 cases 83.3%) |
3.95±3.14 |
1.28-16.53 |
2.45 |
|
Complete Remission (CR) |
||||
CR (42 cases 70%) |
3.00±1.78 |
1.28-7.65 |
2.24 |
<0.001 |
No CR (18 cases 30%) |
11.55±4.74 |
3.51-19.52 |
10.99 |
|
Table 3 Impact of HIF-1α Gene Expression on different parameters in AML patients
Bold values are statistically significant.
Sig: P<0.05; HS: P<0.001; NS: P>0.05
Impact of HIF-1α Gene Expression on Overall Survival (OS) of AML patients
By using Cox Regression to find impact of HIF-1α gene expression level on OS of patients. HIF-1α gene was highly associated with OS (p<0.001). Patients with lowerHIF-1α expression level had better OS than patients with higherHIF-1α expression level. Hazards ratio was 1.349 (95% CI: 1.220-1.492). Hepato splenomegaly was an important risk factor for OS of AML patients, patients without HSM had longer OS than patients with HSM (p<0.001). Hazards ratio was 5.321 (95%CI: 2.091-13.543). LNs enlargement was also an important risk factor for OS of AML patients, patients without LNs enlargement had longer OS than patients with LNs enlargement (p<0.001). Hazards ratio was 7.365 (95%CI: 2.803-19.351). No other patients clinical or hematological parameters was associated with OS (p>0.05) (Table 4).
Parameters |
Overall Survival (OS) |
||
P-value |
Hazard Ratio (95% CI) |
||
HIF-1 gene level |
<0.001 |
1.349 |
1.220-1.492 |
Age |
0.405 |
1.013 |
0.982-1.046 |
Gender |
|||
Male versus Female |
0.731 |
1.168 |
0.482-2.829 |
Total leukocytic count |
0.247 |
1.003 |
0.998-1.007 |
Haemoglobin |
0.363 |
0.898 |
0.712-1.133 |
Platelets count |
0.714 |
1.001 |
0.995-1.008 |
BM blasts |
0.992 |
1 |
0.978-1.022 |
HSM |
|||
Positive vs Negative |
<0.001 |
5.321 |
2.091-13.543 |
LN enlargement |
|||
Positive vs Negative |
<0.001 |
7.365 |
2.803-19.351 |
Table 4 Impact of HIF-1α Gene Expression on Overall Survival (OS) of AML patients
Bold values are statistically significant
Sig: P<0.05; HS: P<0.001; NS: P>0.05
Impact of HIF-1 α Gene Expression on Disease Free Survival (DFS) of AML patients
HIF-1α gene was highly associated with DFS (p<0.001). Patients with higherHIF-1α expression level had shorter DFS; Hazards ratio was 2.192 (95% CI: 1.642-2.927). HSM was an important risk factor for DFS of AML patients, patients with HSM had shorter DFS than patients without HSM (p<0.001). Hazards ratio was 10.522(95% CI: 3.459-32.011). No other patients clinical or hematological parameters was associated with DFS (p>0.05) (Table 5).
Parameters |
Disease Free Survival (DFS) |
||
P-value |
Hazard Ratio (95% CI) |
||
HIF-1 gene level |
<0.001 |
2.192 |
1.642-2.927 |
Age |
0.08 |
1.037 |
0.996-1.080 |
Gender |
|||
Male versus Female |
0.249 |
0.547 |
0.196-1.525 |
Total leukocytic count |
0.098 |
1.004 |
0.999-1.009 |
Haemoglobin |
0.308 |
0.871 |
0.668-1.136 |
Platelets count |
0.215 |
1.004 |
0.998-1.011 |
BM blasts |
0.852 |
0.998 |
0.973-1.023 |
HSM |
|||
Positive vs Negative |
<0.001 |
10.522 |
3.459-32.011 |
LN enlargement |
|||
Positive vs Negative |
0.15 |
4.605 |
0.576-36.836 |
Table 5 Impact of HIF-1 α Gene Expression on Disease Free Survival (DFS) of AML patients
Bold values are statistically significant
Sig: P<0.05; HS: P<0.001; NS: P>0.05
Impact of HIF-1 α Gene Expression on Event Free Survival (EFS) of AML patients
HIF-1α gene was highly associated with EFS (p<0.001). Patients with higherHIF-1α expression level had shorter EFS; Hazards ratio was 1.193 (95%CI: 1.123-1.268) (Table 6). HSM was an important risk factor, patients with HSM had shorter EFS than patients without HSM (p<0.001). Hazards ratio was 5.845 (95% CI: 2.756-12.393). LNs enlargement was also an important risk factor for EFS of AML patients, patients with LNs enlargement had shorter EFS than patients without LNs enlargement (p<0.001). Hazards ratio was 3.515 (95%CI: 1.591-7.762). No other patients clinical or hematological parameters was associated with EFS (p>0.05).
Parameters |
Event Free Survival (EFS) |
||
P-value |
Hazard Ratio (95% CI) |
||
HIF-1 gene level |
<0.001 |
1.193 |
1.123-1.268 |
Age |
0.11 |
1.021 |
0.995-1.048 |
Gender |
|||
Male versus Female |
0.222 |
1.535 |
0.771-3.057 |
Total leukocytic count |
0.415 |
1.002 |
0.998-1.006 |
Haemoglobin |
0.603 |
0.949 |
0.781-1.155 |
Platelets count |
0.706 |
1.001 |
0.996-1.007 |
BM blasts |
0.852 |
0.998 |
0.982-1.015 |
HSM |
|||
Positive vs Negative |
<0.001 |
5.845 |
2.756-12.393 |
LN enlargement |
|||
Positive vs Negative |
0.002 |
3.515 |
1.591-7.762 |
Table 6 Impact of HIF-1 α Gene Expression on Event Free Survival (EFS) of AML patients
Bold values are statistically significant
Sig: P<0.05; HS: P<0.001; NS: P>0.05
Areas of severe oxygen deprivation (hypoxia) arise in tumors due to rapid cell division and abnormal blood vessel formation. The hypoxia-inducible factor-1 alpha (HIF-1α) is a transcriptional factor that mediates transcriptional responses to localized hypoxia in normal tissues and in cancers; it can promote tumor progression by altering cellular metabolism and stimulating angiogenesis.25 The hypoxic BM microenvironment has been shown to contribute to AML.26 In attempt to increase our understanding of the relation between HIF-1α and AML patients, we investigated HIF-1α gene expression in 60 de novo AML patients together with 20 controls by RTQ-PCR. The expression levels of HIF-1α mRNA were significantly higher in AML patients than controls (p<0.001). Our findings are in accordance with Deeb et al.,15 Song et al.27 and Chen et al.28 This finding could be explained by previous studies who found that oxygen supply in BM microenvironment is limited and hypoxia is considered as a physiological condition which leads to organization of a small population of resting hematopoietic stem cells (HSCs) localized in hypoxic niches in BM microenvironment.29 Acute leukemic progression within the BM is associated with further decreases in marrow oxygenation and expansion of hypoxic BM areas.5 These leukemic cells can infiltrate the hypoxic niches and use the homeostatic mechanisms of normal hematopoiesis leading to enhanced self-renewal, proliferation and even resistance to chemotherapeutic agents.30 Theoretically, such BM micro environmental changes may lead to the selective outgrowth of AML clones which are "better adapted" to survive within a severely hypoxic microenvironment than normal hematopoietic cells.5 Adaptation of leukemic cells to the BM microenvironment is an important force in the clonal selection that leads to leukemic cells homing, mobilization, survival and relapse observed in leukemia, such as in AMLs.31
HSCs and progenitors do exhibit a hypoxic profile and strongly express HIF-1α which is the major mediator of hypoxic responses in both normal and malignant cells.30 Hatfield et al.32 also found that culture of primary AML cells under hypoxia induces HIF-1α expression and increases the release of several cytokines, including proangiogenic mediators. In the current study, we found a positive correlation between HIF-1α gene expression level and extra medullary infiltrations (HSM and LNs enlargement). HIF-1α mean expression level was higher in patients with HSM and LNs enlargement than those without. The difference was highly statistically significant (p<0.001). Our findings are in agreement with Chen et al.28 who found higher expression of HIF-1α mRNA and protein in BM of AML patients with extra medullary infiltration. They stated that over expression of HIF-1α are closely related with extra medullary infiltration in AML patients. We didn't find any correlation between HIF-1α gene expression level and other patients clinical or laboratory parameters. Our findings are in agreement with Deeb et al.15 and Chen et al.28 In the current study, when response to treatment was considered, after 28 days of induction therapy; 70% of AML patient achieved CR while 30% didn't achieve CR. We found that HIF-1α gene could be associated with disease progression and bad prognosis as we observed higher HIF-1α mean expression level in patients who didn't achieved CR (11.55±4.74)compared to only (3.0±1.78) in patients who achieved CR. The difference was highly statistically significant (P<0.001). Our findings are in accordance with Song et al.27 who found that the level of HIF-1α mRNA was higher in patients who didn't achieve CR than patients who achieved partial remission (PR) which levels were higher than patients who achieved CR, which levels were higher than control group. As to say, RTQ-PCR revealed a rising tendency in mRNA expression of HIF-1α in healthy control, CR group, PR group and NR group. Their difference was highly statistically significant (p<0.000). Also Chen et al.28 found that higher level of HIF-1α was found in AML patients who did not achieve CR after one or two courses of chemotherapy, however, their difference was not statistically significant. Song et al.27 added that high levels of HIF-1α were associated with poor responsiveness to chemotherapy in AML. They concluded that their data revealed that over-expression of HIF-1α might play a role in the chemo resistance of AML.
Another evidence that HIF-1α gene could be associated with disease progression and poor prognosis, we found that HIF-1α gene was highly associated with OS, DFS and EFS (p<0.001). Hazards ratio was 1.349(95% CI:1.220-1.492) in OS, 2.192(95% CI:1.642-2.927) in DFS and 1.193(95%CI:1.123-1.268) in EFS. Patients with lower HIF-1α expression level had better OS, longer DFS and EFS than patients with higher HIF-1α expression level. Our findings are in accordance with Deeb et al.15 who found that low HIF-1α was associated with both improved OS and EFS. They added that HIF-1α was independently associated with poorer overall and EFS when multivariate analysis was performed. Their results support HIF-1α as an outcome marker for AML. These findings could be explained by previous studies who found that both solid tumors and hematological malignancies contain poorly vascularized regions characterized by severe hypoxia, acidosis and nutrient starvation.33 Tumor hypoxia is always associated with poor patient prognosis, may be because low oxygen levels reduce the effectiveness of radiation therapy, which kills tumor cells by generating reactive oxygen species (ROS).Hypoxic microenvironments leads to cancer progression by activating adaptive transcriptional programs that promote cell survival, motility and tumor angiogenesis.25 One of the major problems in cancer treatment is chemo resistance. Previous studies revealed that cancer cells undergo genetic and epigenetic alterations to adapt to chemotherapeutic stress for survival purposes. Such alterations include increases in drug efflux, increased drug inactivation, increased DNA damage repair, mutations of survival-related genes, abnormal growth factor signaling pathways, activation of intracellular survival signaling and increases in anti-apoptotic gene expressions.34
Hypoxia is closely associated with tumor resistance to anticancer drugs and HIF-1α is one of the major regulators involved in these mechanisms.35 Acute leukemia cells placed under hypoxic conditions up-regulate HIF-1α, undergo cell cycle arrest and show resistance to chemotherapy agents.5,16 As HIF-1 plays important roles in the expression of many genes associated with glycolysis and antiapoptosis, which allow the cancer cells to survive and leads to induction of drug resistance.35 HIF-1α is a transcription factor with multiple target genes, not only Glut-1 (a glucose transporter) and vascular endothelial growth factor (VEGF), but also P53 and Bcl-2. Thus, there are many possible mechanisms that might lead to chemo resistance and in fact there might be not only one mechanism but several mechanisms, depending on the cell type, the level of hypoxia (and HIF-1α as well) and other cofactors like stroma. On the other hand, HIF-1α and low levels of ROS are thought to affect quiescence and differentiation in HSCs. Hence, over expression of HIF-1α might render leukemic blasts more undifferentiated and therefore maintain a larger proportion of leukemic stem cells (which might lead to relapse) in the BM. This could explain the observation of a shortened disease and event free survival in both ALL and AML.15,36 Hypoxic tumors are resistant to chemotherapy and radiation and are associated with poor survival, suggesting hypoxia itself could be a therapeutic target.21,22 If all these hypotheses are shown to be correct, it would also suggest that HIF requirement will not only vary between patients, but also within a patient at different stages of the disease.37
Over expression of HIF-1α might be closely related to extra medullary infiltration and prognosis of AML. Higher HIF-1α gene expression levels are associated with bad prognosis as it was higher in patients who didn't achieve CR. Higher HIF-1α levels are also associated with shortened OS, DFS and EFS. So HIF-1α might be used as a valuable new marker and an early indicator of extra medullary infiltration and prognosis in AML patients.
Thanks to Dr. Seham Omar Mohamed, Professor of Hematology, Clinical and Chemical Pathology Department, Faculty of Medicine, Beni-Suef University for helping us throughout this study.
The author declares no conflict of interest.

©2017 Elhoseiny, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.