eISSN: 2469-2778


Research Article Volume 1 Issue 2
1Clinic of Digestive Surgery, Clinical Center of Serbia, Serbia
2Faculty of Medicine, University of Belgrade, Serbia
3Clinic of Gastroenterology and Hepatology, Clinical Center of Serbia, Serbia
4Institute of Pathology, Serbia
5Department of Medical Biochemistry, University of Belgrade, Serbia
6Center for Medical Biochemistry, Clinical Center of Serbia, Serbia
7Clinic of Hematology, Clinical Center of Serbia, Serbia
Correspondence: Dragica Vucelic, Clinic of Digestive Surgery, Clinical Center of Serbia, Belgrade, Serbia, Koste Todorovic St. 611.000 Belgrade, Serbia, Tel 381(11)3663757, Fax 381(11)3065967
Received: June 18, 2015 | Published: July 14, 2015
Citation: Vucelic D, Jesic R, Zivotic M, et al. Diverse utility of endogenous thrombin potential and thromboelastometry in the assessment of patients with alcoholic cirrhosis. Hematol Transfus Int J. 2015;1(2):34-44. DOI: 10.15406/htij.2015.01.00009
Background and rationale: Diagnosis and treatment of a wide spectrum of abnormalities in the coagulation system in patients suffering from cirrhosis still remain a challenge to physicians. Using endogenous thrombin potential (ETP) method and thromboelastometry, we assessed coagulation profile in 60 adult patients with alcoholic cirrhosis and 50 healthy subjects. We evaluated coagulation profile of patients with these global hemostatic methods, link between ETP/thromboelastometry profiles and standard coagulation tests, relationship between ETP and thromboelastometry parameters with different degrees of liver lesions and correlation between these assays and biochemical liver function.
Main results: In most patients, ETP parameters were consistent with the hypocoagulable profile. The majorities of patients were identified as having decreased Cmax (n=55/60) and AUC (n=49/60) as well as increased t-lag values (n=39/60). There was significance between ETP parameters in two groups (p<0.001). The t-lag was higher in cirrhosis (30.1±10.8 vs. 25.6±14.2s). Both Cmax (peak height) and AUC (area under the curve) were higher in controls (112.0±20.9 vs. 98.3±10.9%; 68.3±28.2 vs. 67.9±16.4%). AUC correlated with cholinesterase (r=0.610; p<0.001), albumin (r=0.462; p<0.001), and total bilirubin (r=-0.281; p=0.031). Using thromboelastometry, we found hypocoagulability represented by reduced MCF (maximum clot firmness) in 33.3% (n=20/60) of patients in extrinsic, and 41.7% (n=25/60) of patients in intrinsic activated test. In patients, CFT (clot formation time) values were significantly higher, whereas MCF values were lower (extrinsic test: 116.6±45.6 vs. 79.2±16.9s; 55.9±8.9 vs. 66.2±4.0mm; p<0.001) compared to controls. There was a weak correlation (r=0.272; p=0.037) between cholinesterase activity and MCF in extrinsic test.
Conclusion: ETP may be an additional alternative for estimating impairment of synthesis liver function and severity degree of cirrhosis caused by alcohol. Thromboelastometry is superior to ETP for investigating coagulopathy in cirrhosis as it provides supplemental information such as maximum clot firmness and stability.
Keywords: Global hemostatic methods; Hepatic disease
Diverse spectrum of hemostatic abnormalities in chronic liver disease has long been considered a key cofactor in the determination of bleeding. There was a solid belief that hemostatic screening profile, consisting of standard coagulation tests, may provide useful information regarding the nature of hemostatic impairment and the extent of the hepatocellular damage, and could be used for clinical decision making related to surgery and invasive procedure treatment approaches.1 However, it has been shown that the results of standard hemostasis tests are poorly correlated with the onset and duration of bleeding after liver biopsy and other potentially hemorrhagic procedures as well as the occurrence of gastrointestinal bleeding or bleeding during liver transplantation.2–7
In recent decades, the old dogma shift associated with the increased appreciation of the rebalanced hemostasis has led to the reevaluation of previously the widely accepted concept of a causal relationship between hemostasis abnormalities and bleeding complications in chronic liver disease.8–17 Restored balance in the hemostatic systemin patients with cirrhosis is provided in several ways including: elevated levels of the platelet adhesive protein von Willebrand factor (vWF), reduced activity of vWF-cleaving protease ADAMTS13 (Adisintegrin And Metalloproteinase with ThromboSpondin motif-13), deficiencies of naturally occurring anticoagulants, elevation of FVIII, and decrease of antifibrinolytics.7–19 There are no widely available and fully standardized methodologies for quantitative assessment of overall hemostasis potential within individual. There is a growing interest in using more global hemostatic assays such as thrombin generation and thromboelastometry/thromboelastograhy.20–25
Thrombin generation assays measure the in vitro capacity of plasma to produce thrombin over time, known as endogenous thrombin potential (ETP). Thrombin generation assays differ from thromboelastometry. Instead of looking at the whole thrombin generation dynamics, thromboelastometry is dependent on thrombin generation measuring its effect on clot formation.26,27 Thromboelastometry considers the cumulative effects of all components of whole blood including cells, plasma proteases and their inhibitors on hemostasis, and thereby it has unique ability to study the clotting process starting with fibrin formation and continue through the clot retraction and fibrinolysis.26,28
We conducted this study in order to evaluate coagulation profile of patients with alcoholic cirrhosis using both unmodified thrombin generation assay and thromboelastometry which are available as routine laboratory tests. Additionally, we correlated these global assays parameters with standard coagulation tests. Finally, ETP, thromboelastometry and some parameters of synthesis and metabolic functions of the liver were compared with disease severity, based on Child-Pugh score (CPs)29,30 among patients. Moreover, global assays results were correlated with parameters of biochemical liver function.
A cross-sectional single center study involved 60 patients with alcoholic cirrhosis and 50 healthy individuals. Following approval of the Institutional Review Board of the Faculty of Medicine, University of Belgrade and the Local Medical Ethics Committee, written informed consent was obtained from the majority of the patients prior to inclusion in the study. In the cases presented with quantitative disturbance of consciousness close relatives, who were completely informed about the aim of the study, provided consent.
Healthy individuals
Fifty healthy volunteers (17males and 33females) with a mean age of 36±8years (range, 20-58years), represented a control group. They were selected among the medical staff of Clinic of Digestive Surgery, Clinical Center of Serbia in Belgrade. None of the volunteers had a history of hematological, hepatic or other disorders, as well as any known treatment which could influence hemostasis.
Patients
Sixty adult patients (57males and 3females) with alcoholic cirrhosis admitted to Clinic of Gastroenterology and Hepatology, Clinical Center of Serbia, Belgrade between March 2011 to June 2013, were enrolled in the study. They were in a mean age of 54±11years (range, 29-79years). Exclusion criteria from the study were: history of hereditary bleeding disorders, use of medications that affect hemostasis, known hereditary thrombophilia factors, cirrhosis associated with other diseases (hepatocellular carcinoma/extrahepatic malignant disease, viral hepatitis, metabolic diseases), primary biliary cirrhosis, primary sclerosing cholangitis, cryptogenic cirrhosis and postoperative states.
Diagnosis of cirrhosis was based on anamnesis, clinical features, laboratory tests, upper digestive endoscopy, imaging diagnostics, and, whenever possible, liver histology. The degree of liver failure was assessed according to Child-Turcotte-Pugh (a.k.a. Child-Pugh) classification, based on the levels of serum bilirubin and albumin, and prothrombin time, and the degree of ascites and encephalopathy. A total score of 5-6 is considered as grade A (well-compensated disease), 7-9 as grade B (significant functional compromise) and 10-15 as grade C (decompensated disease).29,30 Hemostasis was assessed using standard coagulation testing, ETP and thromboelastometry. Blood samples were taken at admission.
Blood sampling and plasma preparation
Peripheral venous blood was collected into BD Vacutainer® Plus citrate tubes containing sodium citrate solution at 0.109mol/L, pH 7.4 (Becton Dickinson, Plymouth, UK). For the ETP and standard coagulation tests, within 60minutes of sampling, platelet-poor plasma was obtained by centrifugation of citrated blood at 2000×g for 15minutes at room temperature. Plasma samples were divided into aliquots of 0.5mL and deep frozen at–70°C until the assays were performed.
Serum samples for biochemical analysis were collected into BD Vacutainer® plastic serum tubes (Becton Dickinson, Plymouth, UK) and centrifuged at 1500×g for 10minutes at room temperature. Samples for full blood count determination were collected using BD Vacutainer® Plastic K2EDTA tubes containing 3.6mg K2EDTA (Becton Dickinson, Plymouth, UK), and analysed on a Coulter®HmX Haematology Analyzer (Beckman Coulter, Inc., Fullerton, CA, USA). For thromboelastometric examination, peripheral venous blood was collected into BD Vacutainer® Plus citrate tubes containing sodium citrate solution 0.109mol/L, pH 7.4 (Becton Dickinson, BD-Plymouth, UK).
Measurements
Conventional coagulation tests and biochemical parameters: Assays were performed using a BCS® XP automated coagulation analyzer (Siemens Healthcare Diagnostics GmbH, Marburg, Germany). Prothrombin time (PT), activated partial thromboplastin time (APTT), and fibrinogen were measured by means of a clotting method using Thromborel® S, Pathromtin® SL, and Multifibren® U reagents, respectively (Siemens Healthcare Diagnostics GmbH, Marburg, Germany). Coagulation factors were assayed by using a PT-based clotting assay with Thromborel® S reagent for factor (F) II, FV, FVII and FX, as well as an APTT-based clotting assay with Pathromtin® SL reagent for FVIII, FIX, FXI, and FXII. Berichrom® FXIII reagent (Siemens Healthcare Diagnostics GmbH, Marburg, Germany) was used for spectrophotometric determination of FXIII activity. D-dimer and von Willebrand factor antigen (vWF Ag) concentrations were measured using immunoturbidimetric assays (vWFAg® and Innovance® D-dimer, respectively; Siemens Healthcare Diagnostics GmbH, Marburg, Germany). Antithrombin (AT) and protein C (PC) were determined by chromogenic assays (Berichrom®AntithrombinIII and Berichrom® Protein C, respectively). Concentrations of albumin, bilirubin, and activities of cholinesterase were determined using standard spectrophotometric methods and commercial reagents (Beckman Coulter, Inc., Brea, CA, USA). Reference values for parameters determined with Siemens reagents (coagulation factors, PT, APTT, AT, PC) are reported by Siemens, and the values for full blood count were provided by Beckman Coulter. All the reference values were validated on the local reference population, during the method validation process in the Center for Medical Biochemistry, Clinical Center of Serbia, where all these analysis were performed.
ETP: The ETP was measured in platelet-poor plasma using a commercially available assay (Innovance® ETP, Siemens Healthcare Diagnostics GmbH, Marburg, Germany). The ETP assay was performed on BCS® XP automated coagulation analyzer (Siemens Healthcare Diagnostics GmbH, Marburg, Germany) according to manufacturer`s instructions. Coagulation activation was initiated by incubation of plasma with Dade®Innovin® Reagent (human recombinant tissue factor and phospholipids) and calcium chloride in the absence of thrombomodulin. Briefly, thrombin generation and subsequent inactivation was recorded by the conversion kinetics of a synthetic thrombin substrate (specific slow reacting chromogenic substrate: H-ß-Ala-Gly-Arg-pNA), which was measured by the release of a chromophore into plasma sample at the wavelength of 405 nm over time. The reference values were validated on the local voluntary non-remunerated repeat blood donors population (n=100), after informed consent was provided, during the method validation process in the Center for Medical Biochemistry, Clinical Center of Serbia, where all these analysis were performed. Blood donors were recruited in Blood Transfusion Institute of Serbia, Belgrade. This was approved by the Institutional Ethical Committee. The parameters that have been investigated on the thrombin generation curve were: lag time (t-lag, describing the time from starting the reaction until thrombin generation is observed, equivalent to clotting time, representing the initiation phase, reference range 17-26s), peak height (Cmax, representing the peak of thrombin generation and reflecting maximal prothrombinase activity, which is the measure of the propagation phase, reference range 102-144%), and area under the curve (ETP-AUC, representing the total amount of active thrombin formed, reference range 82-125%).30 The thrombin burst is finally inhibited by plasma protease inhibitors (termination), and ETP represents the balance between the action of procoagulants and anticoagulants in the plasma.
Thromboelastometry: For thromboelastometric examination, recalcified citrated blood (300μL) was used, within one hour after venepuncture. A TEM® computerised analyser and a set of standard reagents (TEM® International GmbH, Munich, Germany) were employed according to the manufacturer’s recommendations.All analyses were performed in TEM® pin and cups at 37°C. After blood sample recalcification (20µl CaCl2 0.2mol/l) TEM® tests were started, and accelerated by adding an activator (20µl) such as rabbit brain tissue factor (extrinsic activation: EXTEM test) or ellagic acid (intrinsic activation: INTEM test). Two basic tests using EXTEM and INTEM provide information about general coagulation status. The graphical plot of the clot firmness against the time displayed on the TEM® screen defines various parameters in order to describe the dynamics and size of clot firmness during clot formation and lysis. After two hours of measuring, we analyzed the parameters such as the follows: the clotting time (CT: represents the rate of initial fibrin formation; reference range 38-79s in EXTEM and 100-240s in INTEM, respectively), the clot formation time (CFT: defined as the time necessary to attain a clot firmness of 20mm, reflecting an early fibrin polymerization; reference range 34-159s in EXTEM and 30-110s in INTEM, respectively), the maximum clot firmness (MCF: defined as the maximum strength that the clot achieves during the measurement, reflecting the absolute strenght and stability of the fibrin clot; reference range 50-72mm in both tests). Reference ranges for thromboelastometric measurements were previously determined in a multicenter investigation.31 Reference values were validated in the local reference population comprising 50 healthy individuals. Analyses were performed in the Department for Transfusion Medicine, Clinic for Digestive Surgery, Clinical Centre of Serbia.
Statistics: Statistical analyses were performed using the IBM SPSS software, version 20.0. Numerical data with normal distribution are presented as mean±SD, sometimes followed by range, while data without normal distribution are shown as median and range. Normality of numerical data is assessed by Kolmogorov-Smirnov and Shapiro-Wilk tests, as well as considering skewness and kurtosis. Data in Tables are presented as median and range. Categorical variables are presented as frequencies or percentages. In order to examine differences between groups we applied χ2 test, Student’s t test, Kruskal-Wallis, Mann-Whitney test and ANOVA, depending on the data types and number of groups. Assessing the correlations we used Pearson’s and Spearmans’s tests. P values<0.05 were considered to be significant. Graphs were made using IBM SPSS, Microsoft Office Excel and R statistical environment software packages.
Demographic, clinical and laboratory characteristics of healthy individuals and patients with cirrhosis (classified according to CPs into three groups) are shown in Table 1.
Variables |
Healthy Individuals [n=50] |
A [n=5] |
Child-Pugh Score |
C [n=27] |
Age |
32 (24-55) |
44 (29-57) |
52 (32-76) |
56 (41-79) |
Gender Male |
17 |
5 |
27 |
25 |
(number) Female |
33 |
0 |
1 |
2 |
APTT |
35.0 (28.0-39.5) |
35.4 (27.4-43.5) |
43.7 (28.6-57.2) |
52.0 (32.6-86.6) |
PT |
11.9 (10.8-11.3) |
13.2 (12.2-14.5) |
17.1 (11.2-21.0) |
20.1 (13.3-34.9) |
Hematocrit |
0.40 (0.37-0.47) |
0.36 (0.25-0.41) |
0.34 (0.23-0.43) |
0.29 (0.19-0.47) |
Platelets |
230.0 (184-288) |
78.5 (34-114) |
79 (39-315) |
92.5 (31-254) |
Fibrinogen |
3.0 (2.0-3.7) |
3.9 (3.3-5.0) |
3.2 (1.7-7.0) |
2.6 (1.1-6.6) |
Factor II# |
127.0 (101-154) |
97 (79-125) |
67 (33-123) |
44 (17-112) |
Factor V# |
101 (82-125) |
96 (65-136) |
62 (30-129) |
41 (14-134) |
Factor VII# |
109 (90-129) |
81.5 (66-135) |
51 (20-111) |
43.5 (7-181) |
Factor VIII# |
99 (47-152) |
202.5 (119-453) |
147 (38-278) |
167 (24-478) |
Factor IX# |
100 (80-120) |
126.5 (79-146) |
69 (43-150) |
55 (29-153) |
Factor X# |
106 (82-121) |
100 (80132) |
71 (43-136) |
55.5 (25-137) |
Factor XI# |
97 (71-112) |
113 (74-128) |
67 (37-142) |
42 (18-207) |
Factor XII# |
107 (85-129) |
120 (79-146) |
69 (37-123) |
51 (33-213) |
Factor XIII# |
105 (80-131) |
92 (83-138) |
89 (40-155) |
57 (30-141) |
vWF# |
116 (62-149) |
344.5 (177-469) |
305 (123-599) |
407.5 (200-599) |
Antithrombin# |
98 (92-120) |
87.5 (84-93) |
57 (23-125) |
37 (14-88) |
Protein C# |
119 (83-150) |
92 (53-102) |
46 (22-150) |
29.5 (13-86) |
D-dimer |
0.23 (0.17-0.61) |
0.42 (0.26-2.43) |
1.56 (0.33-13.81) |
4.05 (0.7-24.42) |
Table 1 Demographic, clinical and standard hemostasis tests characteristics presented as median (range, minimum-maximum) of healthy individuals and patients with alcoholic cirrhosis
APTT- activated partial thromboplastin time; PT-prothrombin time; #- % of the pooled normal plasma
Standard coagulation tests
When compared with healthy subjects, patients had significantly prolonged PT, APTT, decreased hematocrit, reduced platelet count as well as levels of FII, FV, FVII, FIX, FX, FXI, FXII, FXIII, AT, PC, and increased levels of FVIII, vWF and D-dimer (p<0.001 for all parameters). Median values and range of the all mentioned parameters for healthy individuals and CPs groups of patients are presented in Table 1. Prolonged PT and APTT were noted in 58/60 (96.7%) and in 53/60 (88.3%) patients, respectively. Thrombocytopenia was observed in 52/60 (86.7%) patients.
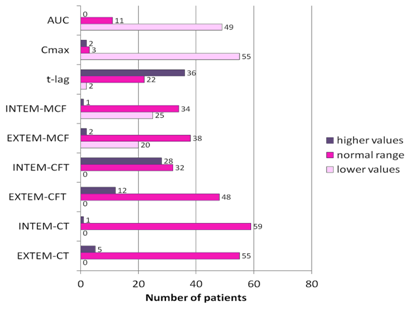
ETP
The distribution of ETP parameters values among CPs groups and controlsis shown in Figure 1 (A-C). The frequencies of patients with abnormal values of ETP parameters are shown in Figure 2. The majority of patients had decreased Cmax (55/60) and AUC (49/60) as well as increased t-lag values (36/60). Compared to healthy individuals, patients had significantly higher t-lag values (30.1±10.8s vs. 25.6±14.2s, p<0.001), and lower both Cmax (68.3±28.2% vs.112.0±20.9%, p<0.001) and AUC (67.9±16.4% vs. 98.3±10.9%, p<0.001) values.
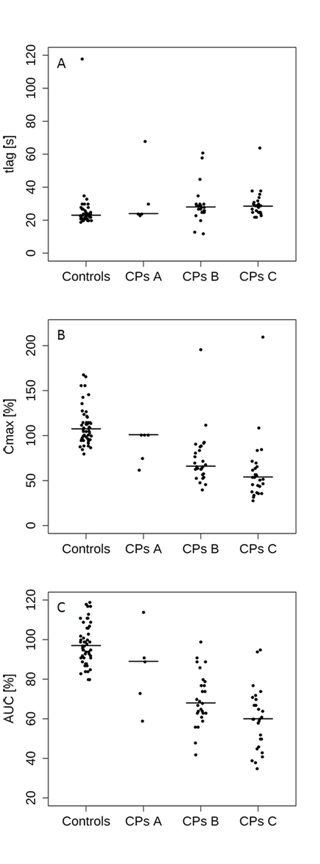
Among CPs groups of patients, there was no significant difference in terms of t-lag [CPsA: 24s (23-68%); CPsB: 28s (12-61%), CPsC: 28.5s (22-64%)]. With increasing of cirrhosis severity, significant gradually decrement for Cmax [CPsA:101% (62-101%); CPsB:66% (40-112%); CPsC:54% (28-210%)] and AUC values[CPsA:89% (59-114%); CPsB:69% (42-99%); CPsC:60% (35-95%)] was observed (Figure 1, Table 2).
|
A [n=5] |
Child-Pugh Score |
C [n=27] |
P Value |
t-lag |
24 (23-68) |
28 (12-61) |
29 (22-64) |
0.831 |
Cmax |
101 (62-101) |
66 (40-112) |
54 (28-210) |
0.002* |
AUC |
89 (59-114) |
69 (42-99) |
60 (35-95) |
0.001* |
EXTEM-CT |
55 (46-80) |
49 (39-103) |
63 (42-94) |
0.323 |
INTEM-CT |
186 (140-231) |
179 (146-219) |
192 (129-240) |
0.114 |
EXTEM-CFT |
120 (78-227) |
108 (44-207) |
110 (61-223) |
0.686 |
INTEM-CFT |
124 (63-254) |
103 (49-220) |
110 (61-240) |
0.340 |
EXTEM-MCF |
56 (42-69) |
57 (43-76) |
55 (33-68) |
0.228 |
INTEM-MCF |
54 (39-64) |
55 (41-73) |
52 (31-67) |
0.205 |
Table 2 Distribution of median values and range of ETP and thromboelastometric parameters according to Child-Pugh score groups
Differences of EXTEM-CT, t-lag and Cmax were testing by Kruskal-Wallis, followed by Mann-Whitney U test, while in other variables ANOVA was applied
With the exception for CPsA and CPsB cirrhosis categories, significant differences among CPs groups of patients were found with regard to AUC (CPsA vs. CPsC, p=0.003; CPsB vs. CPsC, p=0.037).Similar pattern was also shown for Cmax, whereby differences between CPsB and CPsC groups of patients were statistically stronger (CPsA vs. CPsB, p=0.091; CPsA vs. CPsC, p=0.011; CPsB vs. CPsC, p=0.004)
On the whole, only two patients classified with CPsC cirrhosis were hypercoagulable assessed by ETP (Cmax, Figure 2). Clinically, these two patients did not develop any thrombotic complication. Eight patients who had thrombosis of portal vein displayed normal both AUC and Cmax.
Thromboelastometry
Results of the various thromboelastometric parameters (CT, CFT and MCF) in EXTEM, INTEM tests are shown in Figure 3 (A-G).The distribution of patients with abnormal values for the thromboelastometric parametersis shown in Figure 2. CT values in EXTEM/INTEM tests remained within the normal range in the majority of the patients [55/60 (91.7%) and 59/60 (98.3%), respectively] (Figure 2). Consequently, CT values were not significantly different between patients and controls, (Figure 3A-B). The CFT values, both in EXTEM and INTEM, were significantly higher (p<0.001) in patients than in controls, (Figure 3C-D). However, among CPs groups of patients there were no significant differences concerning median CFT values (Table 2).
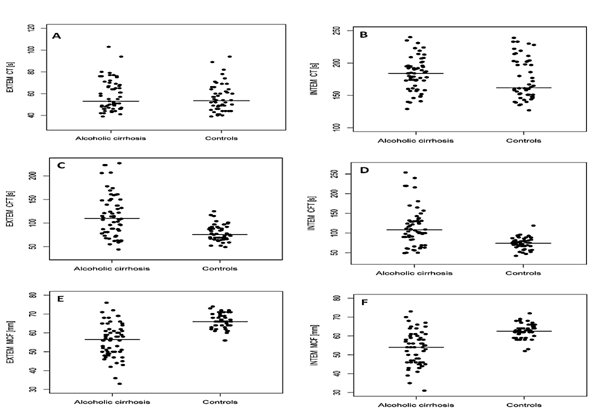
Prolonged EXTEM-CFT was identified among 12/60 patients, whereas approximately half of the patients (28/60) had prolonged INTEM-CFT (Figure 2). In extrinsic and intrinsic activated tests, average values of CFT were 116.6±45.6s (range, 44-227s) and 113.9±47.6s (range, 49-254s), respectively. Pearson’s regression coefficient showed strong correlation between EXTEM-CFT and INTEM-CFT in patients (r=0.905; p<0.001) and controls (r=0.720; p<0.001), respectively. Concerning MCF values both in EXTEM and INTEM tests, patients had significantly lower mean values compared to healthy individuals (p<0.001), (Figure 3E-F).
Among different CPs groups of patients, median MCF values were not significantly different (Table 2). In patients, average MCF values were 55.9±8.9mm (range, 33-76mm) in EXTEM, and 53.2±8.9mm (range, 31-73mm) in INTEM. Significantly strong correlations were observed between MCF values in the extrinsic and intrinsic triggered systems in controls (r=0.907; p<0.001) as well as in patients (r=0.972; p<0.001).
Overall, more than a half of the patients had normal hemostasis assessed by thromboelastometry. In others, tests frequently suggested hypocoagulable profile (number of patients with decreased MCF and/or increased CFT values) rather than hypercoagulable state detected with increased MCF. The majority of patients who were marked as hypocoagulable, using decreased EXTEM-MCF as a marker, suffered from the most severe cirrhosis (CPsC, 11/20-55% of patients). Seven of them (35%) had moderate cirrhosis (CPsB) and only two patients had mild disease (CPsA). Similar patterns were obtained using decreased INTEM-MCF (CPsA, 2/25-8%; CPsB, 9/25-36%; CPsC, 14/25-56%). Two hypercoagulable patients were detected using EXTEM and one patient using INTEM values, and they belonged to CPsB group.
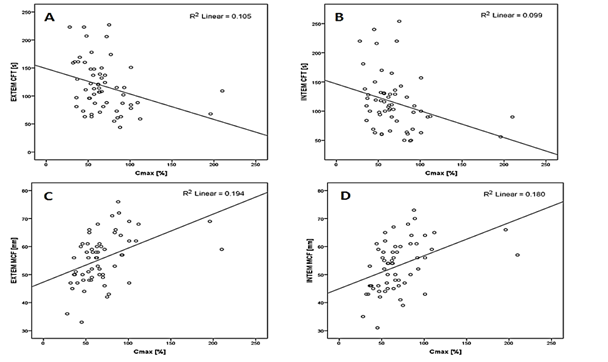
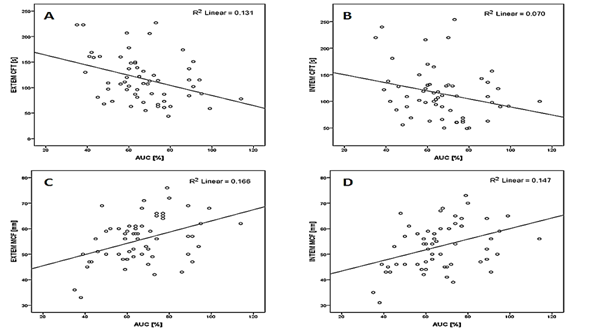
ETP and thromboelastometry relationship
Overall, a higher percentage of patients had ETP parameters out of reference range, whereas thromboelastometric variables were affected in significantly lower proportion. Since some ETP and thromboelastometric parameters reflect similar physiologic phases of hemostasis, we further investigated their correlations applying statistical methods. We did not find correlation between t-lag and CT values either in EXTEM or INTEM. On the other hand, relationships between Cmax and CFT/MCF were statistically significant (p<0.001) in patients (Figure 4), as well as in controls. Significant correlations of AUC and CFT/MCF in patients were also observed, as it is presented in Figure 5. Overall, both Cmax and AUC showed the best correlations for EXTEM-MCF (p<0.001), as illustrated in Table 3.
TEM |
ETP Parameters |
|
C-max |
AUC |
|
EXTEM-CFT |
-0.363 (0.005*) |
-0.509 (<0.001*) |
INTEM-CFT |
-0.350 (0.007*) |
-0.466 (<0.001*) |
EXTEM-MCF |
0.683 (<0.001*) |
0.608 (<0.001*) |
INTEM-MCF |
0.631 (<0.001*) |
0.545 (<0.001*) |
Table 3 Correlations between ETP and TEM parameters, Spearman’s regression coefficient (p value)
Relationship of standard coagulation tests with ETP and TEM parameters
Correlations of standard coagulation tests with ETP and TEM variables are presented in details in Table 4. Thromboelastometric parameters are presented as EXTEM (strong correlations were observed between CFT and MCF in EXTEM and INTEM). Both platelets and fibrinogen showed the strongest positive correlations with MCF (r=0.693 and r=0.594; p<0.001). The other coagulation factors showed the best correlations with ETP parameters. Relationship of AUC to individual standard parameters revealed the best positive correlation for FII (r=0.822; p<0.001). Coagulation proteases FXI, FXII and FXIII correlated slightly better with Cmax compared to AUC. Unlike AUC, but not Cmax, MCF was not influenced by FVIII.
|
Cmax |
AUC |
EXTEM-CFT |
EXTEM-MCF |
Platelets |
0.349 (0.007*) |
0.644 (<0.001*) |
-0.606 (<0.001*) |
0.693 (<0.001*) |
Fibrinogen |
0.406 (0.001*) |
0.356 (<0.001*) |
-0.470 (<0.001*) |
0.594 (<0.001*) |
FII |
0.438 (0.001*) |
0.822 (<0.001*) |
-0.312 (0.016*) |
0.477 (<0.001*) |
FV |
0.317 (0.015*) |
0.692 (<0.001*) |
-0.232 (0.077) |
0.389 (0.002*) |
FVII |
0.538 (<0.001*) |
0.539 (<0.001*) |
-0.384 (0.003*) |
0.440 (<0.001*) |
FVIII |
0.159 (0.233) |
0.554 (<0.001*) |
-0.138 (0.297) |
0.179 (0.174) |
FIX |
0.428 (0.001*) |
0.619 (<0.001*) |
-0.350 (0.007*) |
0.466 (<0.001*) |
FX |
0.254 (0.054) |
0.665 (<0.001*) |
-0.360 (0.005*) |
0.466 (<0.001*) |
FXI |
0.587 (<0.001*) |
0.542 (<0.001*) |
-0.369 (0.004*) |
0.453 (<0.001*) |
FXII |
0.594 (<0.001*) |
0.561 (<0.001*) |
-0.270 (0.038*) |
0.369 (0.004*) |
FXIII |
0.417 (0.001*) |
0.354 (0.006*) |
-0.294 (0.024*) |
0.330 (0.011*) |
vWF |
-0.186 (0.162) |
-0.198 (0.137) |
-0.150 (0.257) |
0.162 (0.220) |
Table 4 Correlations between standard coagulation tests and ETP/TEM parameters
Assessment of synthesis and metabolic functions of the liver according to disease severity and correlations of biochemical liver function with global assays
With increasing severity of cirrhosis based on CPs, there was a significant accretion of total bilirubin levels while the albumin and cholinesterase levels significantly declined, (Figure 6). Median values and frequencies of patients with these parameters out of normal range are shown in Table 5. Since ETP parameters were also significantly different among CPs groups, as previously shown, we further analyzed correlations of Cmax and AUC with total bilirubin, albumin and cholinesterase levels. Cholinesterase correlated moderately (r=0.348; p=0.007) with Cmax and highly (r=0.610; p<0.001) with AUC. We found correlation of albumin with AUC (r=0.462; p<0.001). There was a weak correlation (r=-0.281; p=0.031) between total bilirubin and AUC. The correlations between CFT and MCF and total bilirubin and albumin were not found in this study. There was a weak correlation (r=0.272; p=0.037) between cholinesterase and EXTEM-MCF.
Variables |
Child-Pugh Score |
||||
|
A |
B |
C |
p |
|
Total bilirubin |
Median (range) |
19.3 (12.4-2.6) |
40.2 (8.6-308) |
64.7 (4.4-2.4) |
0.001* |
Normal |
3 (33.3%) |
4 (44.4%) |
2 (22.2%) |
0.011* |
|
Albumin |
Median (range) |
36 (32-42) |
29 (21-36) |
23 (11-32) |
<0.001* |
Decreased |
1 (1.8%) |
27 (49.1%) |
27 (49.1%) |
<0.001* |
|
Cholinesterase |
Median (range) |
4554 (2346-5762) |
3068 (734-8697) |
2145 (910-6826) |
0.003* |
Decreased |
1 (2.1%) |
21 (44.7%) |
25 (53.2%) |
0.001* |
|
Table 5 Parameters of synthesis function of the liver among CP score categories
In spite the fact that there has been a tremendous progress in the understanding of the hemostatic abnormalities in patients with liver disease, there is still scarce information on usefulness of global hemostatic assays in homogenous group of patients with cirrhosis related to alcohol. In addition, data on the correlation of ETP versus standard thromboelastometry measurements in this cirrhosis etiology is lacking. Using these global assays, we investigated coagulation profile in a relatively large number of patients with alcoholic cirrhosis and normal subjects. The main aim of our study was to compare the coagulopathy indicated by ETP with standard thromboelastometry measurement which is in routinely use. Ultimately, we wished to see how results of global assays correlate with clinical phenotypes of these patients and liver synthesis and metabolic functions. We found a large proportion of patients to be hypocoagulableas suggested by the standard laboratory tests (platelet count, PT, APTT). Prolonged PT and APTT were noted in 58/60(96.7%) and in 53/60(88.3%) patients, respectively. Thrombocytopenia was observed in 52/60(86.7%) patients.
Like standard coagulation tests, we have also detected hypocoagulable thrombin generation profile in plasma indicated by prolonged t-lag and decreased peak thrombin and total amount of thrombin produced. Prolonged t-lag was observed in 36/60 (60%) cases while decreased Cmax and AUC under the lower limit of normal were measured in 55/60(91%) and 49/60(81.6%) patients, respectively. Both Cmax and AUC showed tendency for gradually decreasing in a more severe disease, contributing to hypocoagulability. However, Cmax and AUC were not significantly different among patients with CPsA and CPsB. In our thrombin generation test, we used platelet-poor plasma samples. The ETP parameters were measured using a commercially available assay Innovance®. Human recombinant tissue factor and phospholipids, in the absence of thrombomodulin, were the trigger reagents used. Compared to healthy individuals, our patients had significantly higher t-lag values (30.1±10.8s vs. 25.6±14.2s, p<0.001), and lower both Cmax (68.3±28.2% vs.112.0±20.9%, p<0.001) and AUC (67.9±16.4% vs. 98.3±10.9%, p<0.001) values. Possible explanation for this observation in our study is absence of soluble thrombomodulin in ETP measurement and consequently impaired thrombin generation, as it was formerly suggested by Tripodi et al.22
By adding thrombomodulin (under these experimental conditions PC is fully activated, and coagulation is rebalanced due to the concomitant reduction of both pro- and anti-coagulants that occurs in cirrhosis), patients generated as much thrombin as controls.22 Using unmodified thrombin generation method (without thrombomodulin), Gatt et al.24 found no difference between the mean ETP levels of the patients with cirrhosis and the controls. In addition, only 8.2% of patients had reduced ETP levels, but the authors didn’t discuss whether there were any differences concerning ETP by etiology (they explored heterogeneous group of patients with different causes of cirrhosis). The reason for condition of inequality in proportion of patients with affected thrombin generation potential compared to our study may be due to differences in selection of patients or methodology. We explored homogenous group of patients with cirrhosis related to alcohol. Due to known different impact on hemostasis system by etiology, we excluded patients with other etiologies such as primary biliary cirrhosis, primary sclerosing cholangitis, cryptogenic cirrhosis and cirrhosis associated with viral hepatitis and malignant disease, some of which are known to produce hypercoagulabile state. In modified thrombin generation assay (with adding Protac-a non-physiologic activator of PC), Gatt et al.24 found the coagulation system in plasma of patients with cirrhosis to be procoagulant. Namely, ETP was increased when compared with normal and consistent with hypercoagulable profile in cirrhosis-related coagulopathy.
In a study which explored patients with all-cause cirrhosis, Kleinegriset et al.32 found that patients with cirrhosis show a prothrombotic state in plasma even in the measurements conducted without thrombomodulin which is not in line with Tripodi et al.22 observation. These contrary results were explained by different concentration of added phospholipids (4µM vs. 0.5µM) to the thrombin generation measurements. In the present study, there was a greater proportion of patients classified with CPsB (N=28) and CPsC (n=27) in comparison with Kleinegriset et al.32 study (n=15 and n=6, respectively) in which the majority of patients had well compensated disease (n=52). In patients with increasing severity of cirrhosis, Kleinegriset et al.32 detected the reduction in ETP by thrombomodulin to be diminished, contributing to the hypercoagulability.
In the absence of specific reason for more thrombin generation, the potential to hypercoagulability (procoagulant imbalance) in cirrhosis was interpreted by ‘partial resistance’ pattern to PC activator (resistance to in vitro anticoagulant action of thrombomodulin) in cirrhotics. This reduction in endogenous thrombin potential by thrombomodulin may be in line with significantly decreased PC levels in cirrhosis.24,32,33 In addition, increased FVIII may leads to activated PC resistance. Elevated levels of FVIII (procoagulant driver) in combinationwith decreased PC (anticoagulant driver) aretypically found in patients with cirrhosis.24,33 Additionally, it was suggested that the degree of resistance to thrombomodulin or Protac increases with the severity of liver impairment as classified with the Child-Pugh score, and is directly correlated with the levels of FVIII and inversely correlated with the levels of PC.FVIII in cirrhosis increases with the severity of the disease, reaching median values as high as 200% in the most severe CPsC cirrhosis, while at the same time PC decreases with the severity of the disease, reaching median values close to 40% in CPsC patients. So, the ratio between the two moieties (FVIII: PC ratio) was recommended as an index of procoagulant imbalance.13,33 Furthermore, the reduction of FV (when inactivated it acts as a cofactor to activated PC in the inactivation of FVIII) was indicated as a possible reason for resistance pattern to PC activator.24 But, it remains to be established whether this in vitro hypercoagulability is trulyrepresentative of what occurs in vivo.33
In the present study, only two patients classified with CPsC cirrhosis were hypercoagulable represented by increased value of Cmax. Clinically, these two patients did not develop portal vein thrombosis or any thrombotic events in other localization. On the other hand, none of the patients presented with thrombosis phenotype (n=8 presented with portal vein thrombosis) showed the signs of increased thrombin generation potential. Unlike ETP and standard tests, the signs of hypocoagulability, represented by reduced MCF, were demonstrable in a total of 33.3% in EXTEM and 41.7% in INTEM, respectively. Overall, more than a half of the patients had normal clot firmness assessed by thromboelastometry. Of the remaining patients, the majority showed hypocoagulabile profile (patients with decreased MCF and/or increased CFT values) rather than hypercogulabile state detected with increased MCF. Possible explanation for detecting more patients with reduced MCF in intrinsic system may be the influence of circulating endogenous heparinoids associated with cirrhosis, whose impact on coagulation balance is blocked by a heparin inhibitor in EXTEM. Previously, endogenous heparinoids effects have been postulated as a contributor for hemostasis deterioration in those cirrhotics who suffer portal hemodynamic alterations, endothelial dysfunction or bacterial infection.20,34
The blood clotting process coincides with the transition between the initiation and amplification/propagation phases of reaction. The coagulation phases are intrinsically intertwined, and the amount of thrombin generated during hemostasis determines whether clotting is effective, which is reflected by the structure and stability of a fibrin clot. The amount of thrombin is constantly changing during the process of clot formation. Thus, the ultimate clot structure is a complex function of the pattern of thrombin generation.35–37 So, we investigated the impact of both the peak activity (Cmax) and total amount of thrombin (AUC) achieved during clot generation on the structure and stability of the resulting fibrin clot (MCF).
Using parameters such as MCF, Cmax and AUC, we were able to observe significant correlations of both Cmax and AUC with MCF. The best correlations were obtained for EXTEM-MCF (p<0.001). We observed better MCF correlation with Cmax than with AUC in both patients and controls. This observation is based on the higher regression coefficient for Cmax. Our results suggest that peak of thrombin generation is a major determinant of the ultimate clot structure.
In searching for the relationships between global tests and coagulation factors activity, for majority of coagulation proteases we observed better correlations with ETP compared to MCF. As expected, the prothrombin was the most consistent determinant of the amount of thrombin generated, as quantified by AUC (r=0.822; p<0.001), followed by FV(r=0.692; p<0.001) and FX (r=0.665; p<0.001). Actually, a wide range of factor levels is compatible with normal hemostasis. For most coagulation factors, changing the level between 50% and 150% has little effect on the pattern of thrombin generation. Any variation in prothrombin level is reflected in the pattern of thrombin formation.36,38 The strongest positive determinants for Cmax were FXII (r=0.594; p<0.001), FXI (r=0.587; p<0.001) and FVII (r=0.538; p<0.001). These findings may address the suggested role of contact activation in increasing the thrombin generation39 as well as the role of FXI in coagulation as a ‘booster’ mechanism of thrombin formation in procoagulant responses.37 Concerning MCF, the major predictors were platelets count and fibrinogen (r=0.693; p<0.001 and r=0.594; p<0.001, respectively). These results indicate that platelets and fibrinogen rather than levels of coagulation factors were crucial for clot formation.
Above described differences concerning correlations of these two global assays with standard measurements underlines the fact that ETP and thromboelastometrymethods differ in measuring principle. The ETP and thromboelastometry represent manifold methods which determine different physical properties in diverse circumstances (centrifuged plasma vs. whole blood). While ETP measures in vitro capacity of plasma to produce thrombin, thromboelastometry is viscoelastic method which provides measurement of interactive dynamic hemostatic process in whole blood. Thromboelastometry investigates the global clot formation considering most aspects of hemostasis, including blood cells-specifically platelets, coagulation factors and their inhibitors and subsequent fibrinolysis, reflecting overall clot elasticity. It is direct function of fibrinogen level/fibrin polymerisation and platelets count/function. The MCF is taken to represent the ultimate strength of the clot. Thromboelastometry is dependent on thrombin generation measuring its effect on clot formation.26,27,40 In this study, low fibrinogen level was detected in 9/60 (15%) patients. Taking into account that, in the presence of thrombocytopenia in 86.7% cases, ETP levels were reduced in the majority of our patients while MCF values were decreased in less than a half of patients, it can be presumed that, in addition to platelets, fibrinogen presents the important rate-limiting factor to determine clot firmness.
In contrast to former study,20 we didn’t find significant correlations of CFT and MCF parameters with disease severity estimated by CPs. In addition, in this study the correlations between CFT/MCF and biochemical liver function was not found for albumin and total bilirubin. Only a weak correlation between cholinesterase and EXTEM-MCF was observed. On the other hand, ETP parameters correlated with all explored biochemical variables. Better correlations were noted for AUC than Cmax. Cholinesterase correlated with both Cmax and AUC, while albumin and total bilirubin correlated with AUC. Among investigated parameters of biochemical liver function, the best correlation was obtained for cholinesterase (r=0.610; p<0.001). On the whole, we observed that ETP parameters correlated with both CPs and synthesis function of the liver. So, we hypothesized that ETP may be a potential indicator of cirrhosis severity due to Cmax and AUC represent what happens after PT. We were not able to find literature data on similar investigation in cirrhosis.
Our results suggest the clinical utility of thromboelastometry as a functional assay in providing supplemental information such as maximal clot firmness and stability over time, which cannot be derived from ETP. The clinical decision can be taken for the most targeted therapy, leading clinicians to avoid administration of unneeded prohemostatic factors or delay important diagnostic/therapeutic procedures. In those patients who still might require prohemostatic support, monitoring of therapy can be guided by thromboelastometry. This is of particular importance for patients planning for invasive procedures or major surgery. The primary intention should be focused at defining a coagulation profile at a patient level as it can vary greatly among cirrhotics. Unlike thromboelastometry, ETP could be potentially useful candidate to asses disease severity/liver synthesis function in cirrhotics. With regard to above mentioned, prospective clinical studies are now needed.
None.
The author declares no conflict of interest.

©2015 Vucelic, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.