eISSN: 2469-2778


Case Report Volume 11 Issue 4
Oncological surgery service, Spanish Hospital of Mexico City, Mexico
Correspondence: Gallardo Navarro Elias, Oncological surgery service, Spanish Hospital of Mexico City, Mexico, Tel 2227642945
Received: December 01, 2023 | Published: December 13, 2023
Citation: Elias GN, Francisco GR, Carlos MS. Bilateral renal oncocytosis treated by nephrectomy. Hematol Transfus Int. 2023;11(4):115-117. DOI: 10.15406/htij.2023.11.00317
Renal oncocytosis is a rare disorder in which numerous oncocytic nodules develop in the kidney. It is a benign tumor that is occasionally discovered incidentally when performing an imaging test for other reasons. The clinical case of a patient who presented hematuria of 6 months of evolution is presented. After complementary studies, a right renal mass was discovered, for which he underwent radical nephrectomy, with histological result of carcinoma with an oncocytic appearance compatible with chromophobe carcinoma. He presented in the emergency department 3 months after surgery, presenting with anuria accompanied by renal failure. Imaging studies were again requested and a mass dependence on the left kidney was observed. The same surgical procedure was performed and histopathological study demonstrated that the lesion removed corresponded to oncocytosis. Both kidneys are evaluated with immunohistochemistry, being definitive of bilateral renal oncocytosis.
Keywords: renal oncocytosis, renal neoplasms, benign renal tumor, bilateral nephrectomy
Renal oncocytosis is a rare and recently established condition, characterized by numerous oncocytic tumors in which a spectrum of lesions diffusely affect the renal parenchyma. They are more common in men than in women, sex ratio 2:1, although the age range of presentation is wide, there is a maximum incidence in the seventh decade.1 Clinically, renal oncocytosis may occur sporadically without any underlying disease or may be associated with Birt-Hogg-Dube syndrome, however the genetics of oncocytosis are unknown. It is a tumor composed exclusively of large polygonal cells with eosinophilic granular cytoplasm, they are distinguished by the presence of a large number of mitochondria and abundant oxidative enzymes with adenosine triphosphate, macroscopically they are usually light brown in color and commonly exhibit a dense central area of scarring. , with fibrous trabeculae that extend from this central area in a stellate manner. The prognosis after surgical removal is excellent, since most cases of oncocytosis are confined to the renal parenchyma, so capsular or vascular invasion is rare.2 In this case report, we review this pathology with a focus on its diagnosis and histologically and immune histochemically, given the difficult pre-surgical diagnosis of this neoplasm, the management is generally common with that of the rest of solid kidney neoplasms. The therapeutic criteria tend to individualize cases according to the size of the degree of affection of the renal parenchyma, the symptoms and the impact on function. These criteria allow considering expectant management with close surveillance applicable in small, confined lesions and with minor symptoms to total nephrectomy in advanced and extensive cases such as the present case, where the renal parenchyma presented total replacement due to the size of the neoplasia and impacted the function, leading the patient to renal failure.
The patient presents as a 78-year-old male, allergic to iodine, with a history of systemic arterial hypertension, hypothyroidism, ex-smoker with a smoking index of 12.5 2 years ago, who began his current condition 6 months ago with the presence of macroscopic hematuria accompanied by clots, therefore who goes to consultation and a renal ultrasound is requested with a report of a nodular lesion in the lower pole of the right kidney measuring 6.2 x6 cm, vascularized with the presence of cysts (Figure 1), and magnetic resonance imaging that reports bilateral polycystic kidney disease, solid-looking tumor lesions at the level of the segment. interpolar and lower pole of the right kidney, with a diagnosis suggestive of renal cancer, surgical treatment was decided based on right radical nephrectomy (Figure 2), which proceeded without incident, with a histopathological result compatible with carcinoma with an oncocytic appearance compatible with chromophobe carcinoma, subsequently The patient did not attend a follow-up appointment and presented to the hospital emergency department due to anuria and difficulty urinating. Blood tests were requested with an increase in creatinine of 3.3, which was increasing, accompanied by an increase in nitrogen levels, suggesting failure. renal, ultrasound imaging studies (Figure 1) and magnetic resonance imaging (Figure 3) were requested again and surgical management was decided based on left radical nephrectomy (Figure 4), the histopathological study of the removed lesion established the diagnosis of renal oncocytosis, and was performed. immunohistochemistry of both kidneys confirming CD117+ WEAK/PAX-2+/CK7 + PATCHES (Figure 5) with a definitive result of bilateral renal oncocytomatosis, the patient was discharged in adequate conditions together with the nephrology service to evaluate renal replacement therapy by no longer having kidneys, it is reviewed at 7, 30 days and 3 months post-surgery, observing the patient in adequate conditions as a candidate for kidney transplant.
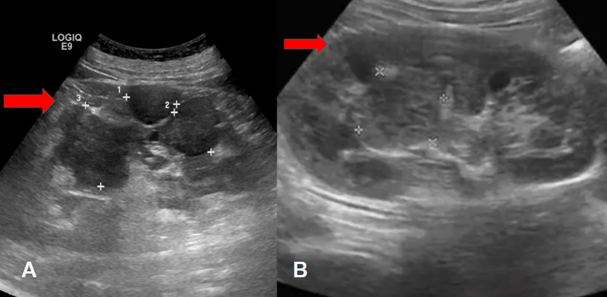
Figure 1 Kidney ultrasound.
A) Left kidney with reported nodular lesion in the lower pole measuring 6.2 x 6 cm with the presence of simple cysts
B) Right kidney nodular lesions with a cystic appearance at the level of the interpolar segment and lower pole of the kidney.
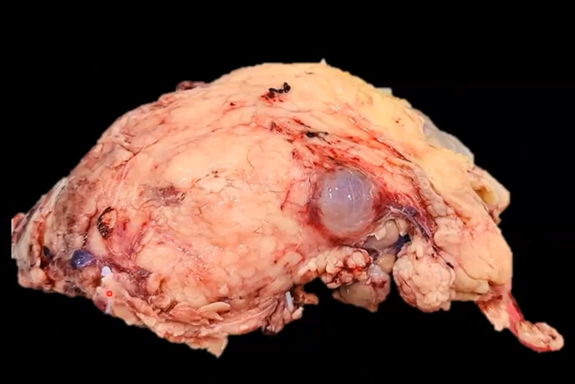
Figure 2 Product of right radical nephrectomy, macroscopic appearance of oncocytomas. Weight 1050 grams. The kidney measures 14 x 12 x 7 cm, its surface is brown, it is covered by abundant yellowish and lobulated adipose tissue with the presence of solid cysts.
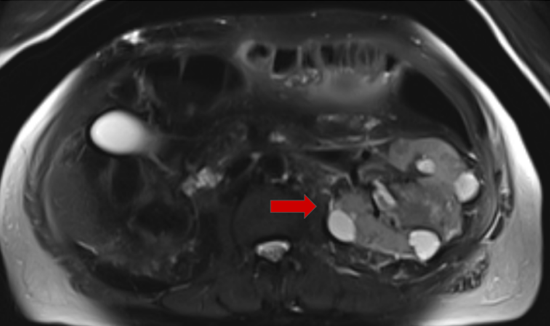
Figure 3 Axial section of abdominal MRI in T1, showing the appearance of oncocytomas (arrow) of the left kidney. Note the hyposignal of oncocytomas compared to the renal cortex.
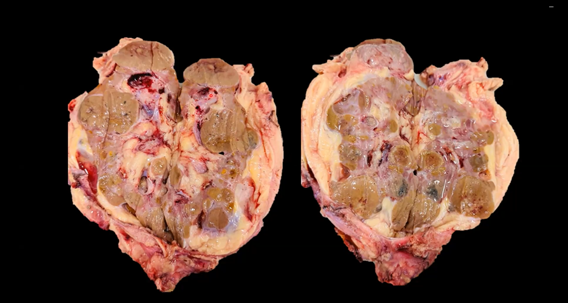
Figure 4 Product of left radical nephrectomy, macroscopic appearance of oncocytomas, brown tumor, well circumscribed, with small foci of intratumoral hemorrhage, Weight 900 grams. Size: multiple nodules from 0.5 cm to 3.5 cm in long axis, residual renal tissue with focal sclerosis, chronic interstitial inflammation, ureter with urothelial hyperplasia and von Brunn nests, renal artery with intimal hyperplasia, negative for malignant neoplasia.
The published series of this pathology in the Spanish literature are few; in 1982, Warfel et al.3 reported the only case of bilateral diffuse renal involvement due to oncocytomas when they reported the case of a 67-year-old woman who presented more than 200 oncocytomas. kidneys, later the Tickoo series,4 the first published, in which, in addition, the authors draw attention to a series of associated changes in the renal parenchyma, defining the condition under the term renal oncocytosis, it is currently considered as a benign epithelial renal neoplasm, and its possible bilaterality, multifocality and association with Birt-Hogg Dubé syndrome has been described, which is described by the development of dermatological lesions such as fibrofolliculomas, trichodiscomas, skin tags, pulmonary cysts with spontaneous pneumothorax, colonic polyps. and also renal tumors, mainly hybrid oncocytic neoplasms, clear cell carcinomas, oncocytomas and papillary renal cell carcinomas.5 As already mentioned, these tumors are macroscopically observed in the affected renal parenchyma, multiple brown nodules of variable size, and microscopically, the oncocyte is observed as an eosinophilic epithelial cell whose cytoplasm is characterized by its high content of megamitochondria.6 Due to the lack of diagnosis, renal oncocytosis has been confused with other tumors such as renal cell carcinoma and chromophobe oncocytoma, so histological, immunohistochemical and molecular genetic characteristics are the tools to differentiate them, an example is colloidal iron staining. Hale test that is positive in renal cell carcinoma and is the useful histochemical characteristic to differentiate it from renal oncocytoma. The association of numerous renal oncocytoma-like nodules with lesions that have a mixed morphology or a pure chromophobe renal cell carcinoma morphology suggests that they may constitute a morphologic spectrum of oncocytic tumors and that renal oncocytoma and chromophobe renal cell carcinoma They can arise from a common progenitor lesion.7–9
Clinically, renal oncocytosis is usually renal masses discovered incidentally without presenting any symptoms, however hematuria may exist as a clinical sign of renal oncocytoma in 3% of cases.10 The diagnostic sequence of this pathology is the same as that used in kidney tumors in general. Kidney ultrasound is a simple, innocuous, economical examination and shows renal oncocytoma as a well-defined, echogenic mass, with solid characteristics in relation to renal parenchyma, isoechogenic, have described the presence of a hypoechoic central scar in large tumors.8 No Doppler criterion confirms the diagnosis of oncocytosis, there are only elements of orientation between benign and malignant tumors.7 In the computed tomography it appears as a mass with well-defined contours, isodense to the renal parenchyma, in the vascular cortical phase contrast uptake is observed that is homogeneous, with the exception of the central stellar hypodensity and in the excretory phase, the tumor is hypodense in the cortex, Based on a study carried out in 2005 on 69 cases of renal oncocytomas, D Eiss et al.,11 attempted to determine the different aspects of the stellar scar, found for oncocytomas larger than 3 cm to improve the diagnostic value, they were able to improve the diagnostic value. distinguish 3 categories, type I a small central star scar is observed with a scar/tumor ratio of less than 50%, type II presents a scar/tumor ratio equal to 50%, type III a star scar greater than 50% is observed, the scar It is defined in this study by a single hypodense range without visible interruption in the different sections performed. Magnetic resonance imaging is a relatively limited study because this pathology does not occur frequently, but the advantages have been described in comparison with the previously described studies, such as absence of ionizing radiation, greater resolution of anatomical structures and better study of blood vascularization. and the ability to obtain information on other axes, William J et al.12 studied the characteristics of the magnetic resonance image of 11 oncocytic tumors, the most common appearance is that of a mass with hyposignal on T1 that increases in intensity on T2, of these 11 cases of oncocytomas, 5 cases (45%) had a well-defined capsule surrounding the tumor and appearing in hyposignal on both T1 and T2, the presence of a homogeneous mass in hyposignal in T1, and in hypersignal in T2 with a central scar or stellar image and the absence of hemorrhage or necrosis suggests the diagnosis of oncocytomas, in the angiography the pattern in wheel spokes is observed, highly suggestive of this pathology, but no imaging study mentioned above is pathognomonic. For Wood BJ et al.13 performing a percutaneous biopsy of a kidney tumor has made it possible to improve therapeutic indications since the preoperative histological diagnosis of oncocytomas makes it possible to avoid radical intervention and expand the indications for conservative surgery due to the benignity of this pathology. However, in the absence of consensus, biopsy cannot be proposed systematically. Currently, the treatment of renal oncocytosis is often based on the size of the tumors and the involvement of the renal parenchyma. In the literature, therapeutic attitudes are observed that are managed on an individualized basis in relation to the renal involvement and symptoms of the disease. patient at the time of diagnosis, the case reports mentioned describe total radical nephrectomy being the most common indication, followed by conservative surgery and surveillance, the literature review attests to the good prognosis of this tumor, and the reason is unknown of the wide range of histological subtypes that occur in renal oncocytosis and no clinical data allows us to predict the oncocytic nature of this tumor.10,14–16
Thanks for the images to the clinical pathology service of the Spanish hospital in Mexico City.
The authors declare that there is no conflicts of interest.
None.

©2023 Elias, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.