eISSN: 2469-2778


Brief Report Volume 9 Issue 5
1Department of Internal Medicine, Tokyo Metropolitan Bokutoh Hospital, Japan
2School of Medicine, Toho University School of Medicine, Japan
3Graduate School of Media and Governance, Keio University, Japan
4Department of Clinical Pharmacy, Yokohama University of Pharmacy, Japan
5Clinical Laboratory, Tokyo Metropolitan Bokutoh Hospital, Japan
6Clinical Laboratory, Tokyo Metropolitan Bokutoh Hospital, Japan
7Center for Medical Education, Faculty of Medicine, Toho University, Japan
8Department of Transfusion Medicine, Tokyo Metropolitan Bokutoh Hospital, Japan
Correspondence: Fumiatsu Yakushiji, Tokyo Metropolitan Bokutoh Hospital, 4-23-15, Koutoubashi Sumida, Tokyo 130-8575, Japan
Received: September 20, 2021 | Published: October 20, 2021
Citation: Yakushiji F, Yakushiji K, Murata M, et al. Appropriate transport of whole blood by drones for cases of massive bleeding. Hematol Transfus Int J. 2021;9(5):105-110. DOI: 10.15406/htij.2021.09.00265
Background: Whole blood (WB) can be superior to red blood cell (RBC) solutions for transfusion in hemorrhage because it contains coagulation factors and platelets. A previous study reported that the quality of an RBC solution and WB can be maintained during transport by an uncrewed aerial vehicle (drone) at normal temperature. Therefore, we aimed to determine whether this approach could also be used for transport of WB for cases of massive bleeding on the hot and cold days that occur in Japan, by testing this approach twice, on hot and cold days.
Method: We used an automobile-transported WB packs obtained by phlebotomy and corresponding segments to a test place in Tomi at a distance of approximately 200 km from Tokyo. Subsequently, a drone (M1000) flight transported the WB and its segments.
Results: The influence of the drone flight on WB appeared to be minimal on lactate dehydrogenase (LDH) level, and the WB was confirmed to be problem-free in coagulation tests.
Conclusion: We transported WB by the drone and confirmed that there were little hemolysis of the WBs and little reduction in the levels of coagulants.
Keywords: whole blood, drone, transportation, coagulation factor, hemorrhage
Trials of blood transport by drones were initiated by Amukele et al. in 20161 and are currently in regular operation in Rwanda and other parts of Africa.2,3 Furthermore, the quality of red blood cell (RBC) solutions transported by a multi-copter type drone with appropriate temperature control has been reported to be maintained with only mild hemolysis.4, and the temperature during helicopter transportation has also attracted attention.5 In addition, a report comparing the time taken for land and drone transport, assuming an urgent demand for blood to deal with bleeding in a surgical operation, clearly showed the superiority of drone transport.6
RBC solutions are not suitable for use in cases of bleeding because they are obtained by removing coagulation factors and platelets from whole blood (WB). The coagulation factors in melted fresh frozen plasma (FFP) carried by drones were reported to be maintained.7 WB-containing coagulation factors and platelets stored at an appropriate temperature can be used for effective transfusion in cases of hemorrhage.8 In the United States, WB is used in initial resuscitation in cases of severe trauma with massive bleeding.
We reported the effectiveness of a multi-copter to transport WBs and their segments at appropriate temperatures in both hot and cold weather and confirmed the quality of the transported WBs by observing that the WBs showed minimal hemolysis with minimal reduction in the levels of coagulation factors.
Study design
We evaluated the quality of the WB by transporting it by a drone flight at the appropriate temperature in two conditions: cold (first) and hot (second).
Preparation and transport to the trial site
In the first study, two 400-mL packs (KBP-66D; Kawasumi Co. Ltd., Oita, Japan) of WB (non-leukocyte-removed, irradiated) obtained by phlebotomy were divided into three portions: one for drone flight, one for non-drone flight, and one for storage in the laboratory. The WB packs in all three groups were further categorized as WB-1 and WB-2. The puncture site was bent in WB-1 and not in WB-2 (Figure 1).
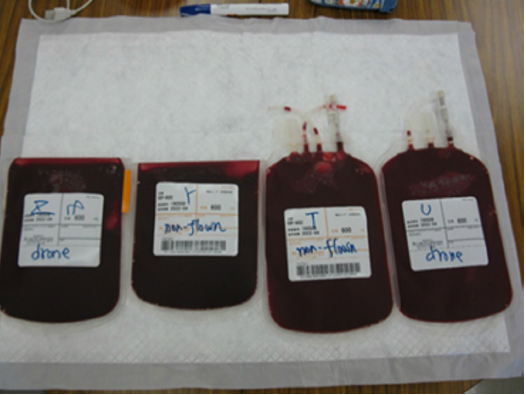
Figure 1 The two WB-1 packs with bending at the puncture site (left), and the two WB-2 packs with no bending at the puncture site (right).
In second study, one 400-mL pack of WB (non-leukocyte-removed, non-irradiated) obtained by phlebotomy was divided into three packs: two 180-mL packs were used in drone flight, of which WB-3 had and WB-4 did not have bent puncture site. The remaining 40 mL of WB was stored in laboratory. In both studies, the WB packs in the transport groups (flight and non-flight) were stored in an ATR700 (Blood transport device, FUJIFILM Toyama Chemical Co. Ltd., Tokyo Japan) set at 2 °C to 6 °C and transported by an automobile to Tomi City in Nagano Prefecture.
Drone flight
We used an M1000 quadcopter (Mazex Corp. Osaka, Japan) to transport the WB packs (Table 1). The WB packs in the drone flights were sandwiched between Type 3 (Type III; JSP Corp., Tokyo, Japan), which were temperature-buffering materials, and placed in a cool box (Campers Collection, Yamazen, Corp., Tokyo, Japan). The Type III which changed from solid to liquid states at approximately 4 °C.9 was pre-controlled by a portable refrigerator. The WBs after the flight and non-flight transport stored in the ATR 700 were transported to Tokyo by an automobile.
|
Drone overview |
|||||
|
Drone model |
M1000 quadcopter (Mazex Corp. Higashiosaka, Osaka, Japan) |
||||
|
Capability |
Load capability of up to 24.9 kg on take-off. Maximum speed of 58 km/h |
||||
|
Operation |
Under visual supervision |
||||
|
Flight information |
|||||
|
Study |
Date time |
Flight time |
Flight distance (m) |
Outside Temperature (℃) |
Cursing altitude (m) |
|
First |
December 29, 2019, |
15.29 |
2,300 |
0 |
10 |
|
Second |
April 3, 2021, |
16.37 |
2,250 |
28.2-32.2 |
10 |
|
Blood temperature optimization |
|||||
|
Method |
WBp swere sandwiched between cold-packs of Type III (coolant) in a cool box |
||||
|
Temperature stabilizer information |
|||||
|
Type III |
Solid–liquid states at approximately 4 °C9 |
||||
Table 1 Drone flights
WBC, white blood cells; Type III, Cold-packs Type; WBp, WB from phlebotomy
Processing of the blood samples
Part of the WBs in the packs were passed through a filter, transfusion set (Terumo Co. Ltd., Tokyo, Japan).10 The WB samples in the no-travel, flight, and non-flight groups, which were centrifuged at 3500 rpm for 10 min, underwent measurements of lactate dehydrogenase (LDH) and other biochemical indices and also subjected to coagulation tests.
Macroscopic findings and laboratory test
The serum and macroscopic findings were evaluated before and after the flights and after filtering (not fragments). Filtering through the transfusion set was supposed to simulate actual blood transfusion conditions. The hematological and biochemical indices and the activated partial thromboplastin time (aPTT) confirming coagulation were measured at BML Inc., Tokyo, Japan. The mean values of LDH and aPTT were tested by t-test using EXCEL 7.0 with a risk rate of 5%.
Temperature
In the first study, as per the temperature records of the ATR before and after the flight, the surface temperature of the WB was maintained at an appropriate value at low outdoor temperatures. In the second study, the surface temperature of the WB-3 was approximately 4 °C, which is appropriate to outdoor air above 30 °C (Figure 2).
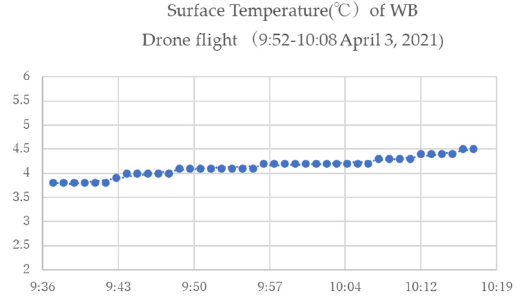
Figure 2 The surface temperature of WB-3 on drone flight at 9:52-10:08 on April 3, 2020 (ambient temperature, 28.2 ℃ to 32.2 ℃) in the second study.
Macroscopic findings for WB and corresponding segments
In the first study, the macroscopic findings of the supernatant of WB-1 and the corresponding fragments showed no clear difference in hemolysis between the stored WB-1 at the hospital and the blood dispensed form WB-1 transported by automobile to Tomi and then by drone flight (Figure 3A); similarly, there were no differences in the changes in WB-2 (Figure 3B). The macroscopic findings for hemolysis in the group with non-bent puncture sites (WB-2) after drone transport were similar to those in the group with bent puncture sites (WB-1), and the differences were minor, as with blood components.
In the second study, gross macroscopic assessments showed that hemolysis was not intensified by flight or road transport. We also observed no difference in relation to bending or unbending of the puncture site (Figures 3C, 3D). The findings for the fragments seemed to be the same.

Figure 3 (A) The macroscopic findings if the supernatants of the WB-1 samples. From left to right, hospital custody, non-drone flying group, and drone flying group. (B) The macroscopic findings of the supernatant in WB-2, in the same order as A. C. The WB-3. D. The WB-4.
Hematological and biochemical indices
The hematological indices evaluated in both studies are shown in the Table 2. The samples showed no differences in hemolytic signs.
|
Whole blood |
Travel |
Days after phlebotomy |
WBCs |
RBCs |
Hgb |
Hct |
MCV |
MCH |
MCHC |
Plt |
|
First study |
||||||||||
|
WB-1 (Bending) |
No travel |
15 |
11,660 |
486 |
16 |
50 |
103 |
32.9 |
32 |
21.6 |
|
Travel without flight |
15 |
11,120 |
488 |
16 |
50.2 |
103 |
32.8 |
31.9 |
23.4 |
|
|
Travel with flight |
15 |
11,670 |
496 |
16.2 |
51 |
103 |
32.7 |
31.8 |
21.3 |
|
|
WB-2 (No Bending) |
No travel |
11 |
7,410 |
455 |
13.5 |
45 |
99 |
29.7 |
30 |
37.4 |
|
Travel without flight |
11 |
7,450 |
429 |
12.8 |
42.6 |
99 |
29.8 |
30 |
34.9 |
|
|
Travel with flight |
11 |
7,430 |
511 |
15.3 |
50.3 |
98 |
29.9 |
30.4 |
34.4 |
|
|
Second study |
||||||||||
|
WBp |
Before travel |
3 |
7,030 |
553 |
14.6 |
47 |
85 |
26.4 |
31.1 |
18.2 |
|
Stored |
No travel* |
6 |
8,950 |
788 |
20.8 |
69 |
88 |
26.4 |
30.1 |
12.9 |
|
WB-3 |
Travel with flight |
6 |
6,570 |
554 |
14.4 |
48 |
89 |
26,5 |
29.0 |
17.9 |
|
WB-4 |
Travel with flight |
6 |
6,640 |
558 |
14.7 |
47.9 |
86 |
26.3 |
30.7 |
16.8 |
Table 2 Hematological indices
*Polycythemia probably occurred due to the unequal division (stored, 40 mL; WB-3, 180 mL; WB-4, 180 mL)
WBC, white blood cells; RBCs, red blood cells; Hgb, hemoglobin; Hct, hematocrit; MCV, mean corpuscular volume; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; Plt, platelets; WB, whole blood; WBp, WB from phlebotomy
Blood glucose, aspartate aminotransferase (AST), lactate dehydrogenase (LDH), sodium, and potassium levels were measured. However, these results are not shown. The results after the blood transfusion simulation were obtained and compared with the findings obtained at the beginning of the experiment: AST, LDH, and potassium levels increased, while the sodium levels decreased. The AST and LDH levels paralleled each other. The results of analyses of hemolysis under each condition are shown in Table 3, with LDH findings as a representative.
|
Index |
Study |
WB and Task |
Before trip |
After trip |
`After filtration |
|
LDH (U/L) |
First study |
WB-1 |
|||
|
Days after phlebotomy |
12 days |
15 days |
15 days |
||
|
Stored in the laboratory |
377±9 |
454±1 |
474±10 |
||
|
No flight |
381±4 |
528±4 |
548±8 |
||
|
Flight |
387±2 |
523±2 |
572±3** |
||
|
WB-2 |
|||||
|
Days after phlebotomy |
8 days |
11 days |
11 days |
||
|
Stored in the hospital |
221±4 |
315±14 |
309±12 |
||
|
No flight |
214±5 |
321±3 |
333±14 |
||
|
Flight |
217±5 |
382±7* |
393±10 |
||
|
Second study |
WB for the second study from phlebotomy |
||||
|
Days after phlebotomy |
3 days |
6 days |
6 days |
||
|
WBp |
142.8±5.1 |
None left |
None left |
||
|
Stored in the laboratory |
WBp-derived |
185.6±3.1 |
175.0±12.2 |
||
|
WB -3 Flight, with bending |
WBp-derived |
180.5±3.4 |
182.0±4.8 |
||
|
WB -4 Flight, without bending |
WBp-derived |
191.3±4.9 |
195.0±7.9 |
||
|
aPTT (s) |
First study |
WB-1, with bending |
|||
|
Days after phlebotomy |
12 days |
15 days |
15 days |
||
|
Stored in the laboratory |
51.8±0.9 |
60.3±3.4 |
61.4±0.7 |
||
|
No flight |
54.1±3.2 |
64.2±0.6 |
66.1±1.0 |
||
|
Flight |
53.1±1.3 |
65.2±0.7 |
68.1±1.1*** |
||
|
WB-2, without bending |
|||||
|
Days after phlebotomy |
8 days |
11 days |
11 days |
||
|
Stored in the hospital |
45.8±0.4 |
49.9±0.4 |
51.1±0.8 |
||
|
No flight |
45.2±0.3 |
50.8±0.7 |
51.9±0.4 |
||
|
Flight |
45.2±0.5 |
52.6±0.5 |
52.7±0.3 |
||
|
Second study |
WB for the second study from phlebotomy |
||||
|
Days after phlebotomy |
3 days |
6 days |
|||
|
WBp |
36.1±0.4 |
None left |
Not performed |
||
|
Stored in the laboratory |
WBp-derived |
38.2±0.7 |
Not performed |
||
|
WB-3, Flight, with bending |
WBp-derived |
36.5±0.9 |
Not performed |
||
|
WB-4, Flight, without bending |
WBp-derived |
36.4±0.6 |
Not performed |
||
Table 3 LDH and aPTT measurements
* Flown (WB-2) is highly significant, longer with significant difference after filtering by the flow (WB-1) at a 5% rejection rate
LDH, lactate dehydrogenase; aPTT, activated partial thromboplastin time; WB, whole blood; WBp, WB from phlebotomy
Changes in LDH levels with and without transportation and by drone flight to the experimental site
In the first study, for WB-1, there were no significant differences in the changes in LDH levels before and after the experiment (Table 3). The levels of LDH showed a significant difference after filtration. For WB-2, a significant difference was observed in the changes in LDH levels before and after the experiment. However, there were no significant differences after filtration. In the second study, there were no difference in LDH levels regardless of whether the WB packs were flown or stored in a laboratory.
Changes in aPTT and other coagulant factors with and without transportation and drone flight to the experimental site
For WB-1, the prolongation of aPTT showed a significant difference after filtration; however, no other significant changes were observed (Table 3). For WB-2, there was no significant difference in the aPTT. Unlike the first study, the aPPT results showed no changes after passage through the filter; there appeared to be little change in coagulation factors due to transport. There were no significant differences, however, the aPTT appeared to be prolonged in specimens stored in the laboratory. The flight did not seem to affect the aPTT (Table 3).
The effect of the drone flight on WB was evaluated. The WB packs showed no gross hemolysis due to transport, and they showed a mild increase in LDH levels. However, gross evaluation indicated no major hemolytic findings, and there was no clear flight-induced change in aPTT. Although the data are not shown, the prothrombin time (PT) and fibrinogen level were also measured, and the results were similar.
WB transported in a gentle way with temperature control will typically not undergo hemolysis and can be expected to show optimal retention of coagulation factors. Although temperature can be maintained at approximately the right level, the vibration during multicopter drone flight can also cause deterioration of the blood. Our results suggested that vibrational effect by the M1000 caused little deterioration in the quality of the WB.
Although we did not use a vibrometer during the flight, based on several flight experiments with the RBC solutions, the effect of the vibration during flight was probably greater than that during car transportation. However, we supposed that the vibration of M1000 has a peak frequency of approximately 60 Hz from 3600 to 3800 rpm; thus, the high-frequency vibration associated with high energy levels exceeding 100 Hz, which is said to be caused by the DJI MARICE 600,11 did not might happen in gentle flight. The vibration of the M1000 may not cause a high level of blood hemolysis.
In Japan, RBC solutions and FFP are used to meet the demand for blood in emergency situations such as trauma. These blood products are produced by the Japan Red Cross, and the distribution of blood products is based on component transfusions. Data from the FY2020 Survey on the Use of Blood Products showed that the use of WB in Japan was low, and its use was skewed toward small medical institutions.12 We do not think that these choices are necessarily based on the indications for WB clotting factor content. They could also be related to the ability of large medical institutions, which deal patients bleeding, to control the temperature of FPP and easily obtain FFP.
Blood transport in Japan, at least in urban areas, is based on established methods of express delivery by automobiles; however, considering the occurrence of traffic disruptions, drone transport has been shown to yield significant time savings by Homier et al.6
The limitations of this study should be noted. We used LDH measurements to evaluate hemolysis. Although free hemoglobin measurements are a superior index of hemolysis, we could not measure free hemoglobin because of a lack of companies performing such measurements in Japan. Thus, we used LDH measurements based on our experience. Although we were able to confirm that the ATR700 can cope with low temperatures for prolonged periods, we were also unable to completely solve the problem of temperature management. During the drone flight, we were able to prevent the blood from deteriorating under outdoor temperatures of approximately 0 °C by using temperature-buffering materials, and we did not conduct these tests at lower temperatures. Moreover, while RBC solutions have been tested at outdoor temperatures of approximately 30 °C.4, we do not know the results for WB at very high temperatures.
The mechanical performance of drones for transport of medical supplies has been demonstrated in Spain. However, the transport capacity of the DJI MARICE 300 RTK used for this purpose is approximately 2 kg.13 We aimed to transport blood in a temperature-controlled environment, and the M1000 permitted load of 24.9 kg, which means that it can carry a load of more than 10 kg after subtracting its own weight. However, for safety reasons, drones such as M1000 are too large for practical use. On the other hand, while temperature control for WB is essential to retain blood quality, strict temperature control will increase weight. Nevertheless, for immediate blood operations, smaller drones such as the DJI MARICE 300 may be useful. Considering the 1-hour grace period for deviation from the appropriate temperature range of 2–6 °C under current Japanese rules.14, it may be possible to use short drone flights within 1 hour. However, for long-distance transportation, out-of-sight satellite links remain the only option.
We transported WB using drones and found that the WB samples showed no deterioration. The aPTT prolongation caused by drone transport of WB was minimal, and drone transport caused no other problems. Furthermore, while we have focused on drone transportability, we also believe that WB transfusion for cases of massive bleeding needs to be considered in the future in Japan.
None.
The authors declare no conflicts of interest.
This study received no external funding.

©2021 Yakushiji, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.