eISSN: 2469-2778


Case Report Volume 11 Issue 2
1Department of Dermatology, Hospital Santa Teresa, Brazil
2Department of Pathology, University Hospital Professor Polydoro Ernani de São Thiago, Brazil
Correspondence: Isadora Paula Pavei, Dermatology, Hospital Santa Teresa, Brazil
Received: April 10, 2023 | Published: May 1, 2023
Citation: Isadora PP, Almeida MP, Amorim GM, et al. Adult t-cell leukemia/lymphoma: case report in southern Brazil. Hematol Transfus Int. 2023;11(2):49-50. DOI: 10.15406/htij.2023.11.00301
Adult T-cell leukemia/lymphoma (ATLL) is an aggressive type of non-Hodgkin's lymphoma that can be primary of the skin or secondary, caused by Human T-cell lymphotropic virus (HTLV-1) infection. The prevalence of HTLV-1 infection is high in Brazil, however reports of ATLL are rare, possibly underdiagnosed and underreported. This paper presents a case report of a patient coming from the south of Brazil, a region of the country with few cited cases of this comorbidity. It shows the importance of disclosing data on infection by the virus, so that public policies for prevention can be carried out, as well as the presentation of cases that develop ATLL.
Keywords: adult t-cell leukemia/lymphoma, ATLL, HTLV-1, non-hodgkin's lymphoma
ATLL, adult t-cell leukemia/lymphoma; HTLV-1, human T-cell lymphotropic virus 1; WHO, world health organization; PUVA, psoralen plus ultraviolet A; CHOP, cyclophosphamide, doxorubicin, vincristine and prednisone; HIV-1, human immunodeficiency virus 1
Adult T-Cell Leukemia/Lymphoma is a type of non-Hodgkin T-cell lymphoma (ATLL), aggressive, with expression of CD4 and CD25, which can affect the skin, associated with human cell lymphotropic virus (HTLV-1) infection. It can be primary cutaneous, that is, when the diagnosis is restricted to the skin, or secondary. It has four variants, according to the World Health Organization (WHO), acute (60%), lymphomatous (20%), chronic (15%) and smoldering (5%). There is also a fifth form, known as primary skin tumor that is not included in the classification by Shimoyama et al. on which the WHO is based.1
The definition of the smoldering form is not very clear in this classification, it can be interpreted in two ways: one with 5% or more of atypical lymphocytes in the peripheral blood and the other with less than 5% of abnormal cells associated with malignant involvement of the skin and/or lungs. Many authors consider only this last variant,2 which still has the absence of hypercalcemia, visceromegaly and LDH elevated up to 1.5 the reference value. As in the chronic form, it has a 25% chance of transforming to the acute form.1 When updating the classification of primary cutaneous lymphomas, ATLL was included, although there is no specification about the variants.3
Female, 68-years-old, born in southern Brazil, housewife. Appearance of purplish, painful and pruritic erythematous infiltrative plaques, permeated by healthy skin, which started on the face and quickly progressed to the trunk and limbs, craniocaudal dissemination (Figure 1), 8 years ago. The patient has a family and personal history of HTLV-1 infection, in addition to being hypertensive and with coronary disease. Five years after the appearance of the skin lesions, that were previously not investigated, she presented with dyspnea, night sweats, fever and a decline in general condition.
The investigation was started with an incisional biopsy of the skin, which showed an intense monomorphonuclear infiltrate in a band at the dermal-epidermal junction, with atypical lymphocytes that lit up the epidermis, isolated and in clusters (Figure 2). In the immunohistochemical study it was possible to observe positive CD4 in practically all lymphocytes of the dermis and epidermis and positive CD25 in all atypical lymphocytes (Figure 3). Laboratory tests showed slightly elevated LDH, positive ANA 1:640, speckled cytoplasmic pattern with isolated dots, and strongly positive anti-RO (Soren’s Syndrome), in addition to the absence of hypercalcemia. The patient has no involvement of other organs and systems, being classified and treated as smoldering ALLT.
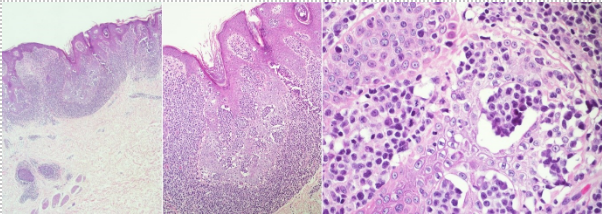
Figure 2 Intense monomorphonuclear infiltrate in a band at the dermal-epidermal junction, with atypical lymphocytes that lit up the epidermis, isolated and in clusters.
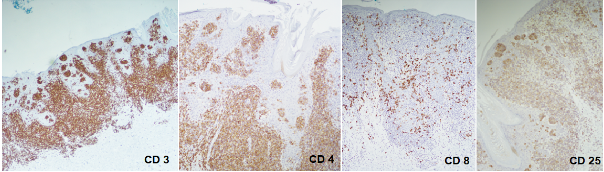
Figure 3 Positive CD4 in practically all lymphocytes of the dermis and epidermis and positive CD25 in all atypical lymphocytes.
Until the moment she has already undergone treatment with Psoralen plus ultraviolet A (PUVA), radiotherapy, oral and intravenous corticosteroids, alpha interferon associated with zidovudine, transretinoic acid, in addition to the chemotherapy regimen that associates cyclophosphamide, doxorubicin, vincristine and prednisone (CHOP). She is currently in remission of the disease.
ATLL is an uncommon type of hematologic malignancy associated with infection by the HTLV-1 virus.1 Despite the prevalence of HTLV-1 infection in Brazil being high, between 800,000 and 2,500,000, reports on ATLL are rare considering that 4% of those infected evolve to this comorbidity. Approximately 856 new patients are diagnosed each year in the country. The states of São Paulo, Rio de Janeiro, Bahia, Minas Gerais and Pernambuco register the highest number of cases.4 There are few data available on the prevalence of cases in the southern region, which includes the states of Paraná, Santa Catarina and Rio Grande do Sul, however, is known to have the lowest prevalence rates in the country. In Santa Catarina, a blood bank found a prevalence of 0.03% of donors infected with the HTLV-1 virus.5
Brazil has a similar number of people infected with the virus than Japan, therefore, the estimated occurrence of the disease is approximately 100 times greater than documented.4 Consequently, it is crucial that they be reported, especially those which occur in unconventional regions, such as the southern region of the country,4,6 so that physicians are aware of the disease and do not delay diagnosis and treatment.
ATLL is caused by the HTLV-1 virus, as already mentioned. Its transmission occurs vertically, predominantly through breastfeeding, being contraindicated in these cases, besides sexual intercourse and contamination through blood. Lymphoma is more associated with cases of transmission through breastfeeding, also, people with the expression of HLA A26, B4002, B4004, B4006 and B4801 appear to be genetically more predisposed to develop the disease.1
ATLL can be extremely aggressive with a very reserved prognosis and a mean survival of 6 to 8 months in the acute and lymphomatous form, however the patient has the smoldering form with malignant skin involvement. She was referred to several treatments, which for some time were effective, with relapse afterwards. Even when the disease is in remission after the CHOP chemotherapy scheme, it is known that the response is limited and relapse is almost certain. The patient's evolution is in line with studies performed with statistical significance, which observed that in the exclusive involvement of the skin, survival is much higher compared to patients who have other organs affected.2
For this reason it is imperative to differentiate between the types of ATLL and to include the smoldering form - in the WHO classification - with primary involvement of the skin in the forms with the best prognosis. Generally, these patients die of infections not related to the virus and not due to an evolution to the acute form of the disease, with an average survival of 4 years.2
According to the 2020 Brazilian Protocol for Sexually Transmitted Infections: human T-lymphotropic virus (HTLV) infection,6 information on epidemiology stems from old studies, which do not precisely define incidence and prevalence rates, then do not provide or enable up-to-date prevention and control measures. HTLV-1 is not part of the prenatal routine in southern Brazil, nor is it included in the list of diseases and conditions with mandatory national notification.
Thus, the importance of identifying those infected with HTLV-1 and disclosing patients who develop this type of lymphoma, a severe form of the infection, is observed. In this case, for example, the patient had almost the whole family affected by the virus, the mother and two sisters who died as a result of the ATLL, but no records were found in the country's health data.
ATLL cases are underdiagnosed and/or underreported in Brazil, hence there is little data available to perform research work. Accordingly, it is important that all reports be disclosed at the time of diagnosis, as well as when there is an infection with the HTLV-1 virus, which can also cause other dermatological alterations, such as severe forms of scabies – especially when there is co-infection by Human Immunodeficiency Virus 1 (HIV-1), ichthyosis, seborrheic dermatitis and dermatophytosis.
It is, therefore, essential to know the prevalence of the virus in Brazil, so that public health policies aimed at the condition can be implemented, and the understanding of the clinical manifestations in order that the diagnosis is not delayed and the establishment of therapy is brief.
None.
The author declares that there is no conflict of interest.
None.

©2023 Isadora, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.