eISSN: 2469-2778


Case Report Volume 7 Issue 2
1Department of Pediatrics, King Fahd Armed Forces Hospital, Jeddah, Saudi Arabia
2College of Medicine and Surgery, King Abdulaziz University, Jeddah, Saudi Arabia
Correspondence: Housam Almadani, Department of Pediatrics, King Fahd Armed Forces Hospital, Jeddah, Saudi Arabia, Tel 966504685495
Received: March 18, 2018 | Published: March 22, 2019
Citation: Almadani H, Mirza ZT, Alghufaili SK, et al. A retropharyngeal Ewing sarcoma in 7-year-old child with single kidney. Hematol Transfus Int J.2019;7(2):31-33. DOI: 10.15406/htij.2019.07.00201
Ewing sarcoma is a well-known primary bone tumour and it is extremely rare to be found in the retropharyngeal area. We report a 7 years old boy with retropharyngeal Ewing sarcoma and single kidney.
Keywords: retropharyngeal mass, single kidney, small round blue cell tumor, Ewing's Sarcoma, chemotherapy
Ewing sarcoma (ES) is one of the famous small round blue cell tumour family members that considered the second most common bone tumour in paediatric age group and makes up about 10-20% of all primary malignant bone affecting this population.1 ES most commonly affecting lower extremity, while Skull area affection is rare account for only 1% of all ES cases. Primary ES, affecting nasopharyngeal/retropharyngeal area is by far extremely rare.2 We are reporting a retropharyngeal ES tumour in a 7years old boy with a single kidney.
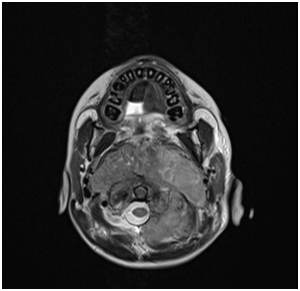
7 years old boy presented with history of left neck mass, headache and weight loss for 1-month duration, with limited range of motion of the neck and increasing pain in that region for 5 days before he was referred to our hospital. Physical examination revealed left upper cervical swelling measuring 5x6 cm in diameter, firm in consistency and attached to the underlying structures, no neurological deficit of signs of respiratory compromise was observed. His initial laboratory results are shown in Table 1. Cervical lymph node biopsy revealed reactive lymph nodes, negative for granulomata and negative for malignancy. Magnetic resonance imaging (MRI) of the neck (Figure 1) showed evidence of perivertebral/retropharynegal large multilobulated soft tissue mass measuring about 7.9x8.7x6.9 cm in transverse, craniocaudal and at the posterior dimensions respectively, extending in the nasopharyngeal region, and extending opposite to the skull base, clivus and upper cervical vertebra body posteriorly with the extension through the neural foramina of C1 and C2 vertebrae and causing bony erosions, extending into the spinal canal, however the signal intensity of the spinal cord was preserved, with narrowing of the right vertebral artery and questionable tumour involvement at the level of C1. Superior extension of the mass is seen obstructing the nasopharynx, anteriorly the mass is seen compressing the nasopharynx and exerting mass effect on the oropharynx with no patent airway seen around endotracheal tube. Infiltration of the hard palate and palatine tonsils were seen, laterally the mass seen compressing the carotid vessels bilaterally with suspicion of marked compression and occlusion of the left jugular vein, however the carotid arteries were patent. The patient underwent incisional biopsy of the retropharyngeal mass and bilateral bone marrow aspiration & biopsy. During surgery patient was electively intubated and due to difficulty in extubating and critical obstructed airway a tracheostomy tube was inserted to ensure patent airway. Histopathological examination of the retropharyngeal mass showed small blue cells with scant cytoplasm (Figure 2). Immunohistochemical studies showed that tumor is positive for CD99 and Vimentin, negative for Myogenin, TTF-1, Pankeratin, Desmin, Chromogranin,CD45, Synaptophysin, SMA, MSA ,CK7,EMA,CD56, CD34, and PAX5. Fluorescence in situ hybridization (FISH) study showed fusion of the ESWR1/FLI1 genes associated with the translocation t(11;22)(q24.3;q12.2) Thus radiological, histological and immunohistochemical finding were confirmatory of Ewing sarcoma of the retropharyngeal space. Bone scintigraphy showed no evidence of bone metastasis. As incidental finding on CT abdomen revealed a single hypertrophied right kidney with mild hydronephrosis. Renogram was done and showed partial obstruction, Later patient developed acute renal injury and anuria, ultrasound kidney showed severe hydronephrosis with obstruction. His case was discussed with the infectious disease and nephrology physicians and the decision was made to insert double J stent under interventional radiology, signs of renal function recovery were seen in the next 2 days. Patient started on European Ewing tumour Working Initiative of National Group 99 (EURO-E.W.I.N.G99) protocol, ended first cycle of chemotherapy that contained vincristine, ifosfamide, doxorubicin and etoposide and supported with G.C.S.F (VIDE), with acceptable tolerability. Planned for evaluation after 2 cycles for the local control option.

Result |
Reference range |
|
WBC |
7.46x109 |
(4.5-14.5)x109 |
RBC |
5.45X1012 |
(4-5.2)x1012 |
Hemoglobin |
12.7g/Dl |
(11.5-15.5)g/Dl |
Hematocrit |
39.70% |
(35-45)% |
Platelet count |
394X109 |
(150-500)x109 |
C reactive protein |
59mg/L |
(0.4-5)mg/L |
Erythrocyte sedimentation rate |
51MM/HR |
(0-10)MM/HR |
PTT |
31.8sec |
(29.98-40.39)sec |
Prothrombine time PT |
13.8sec |
(12.6-14.61)sec |
INR |
1.02 |
(0.9-1.15) |
Ferritin |
223.42ug/L |
(7-140)ug/L |
Lactate dehydrogenase |
324U/L |
(135-225)U/L |
Urea |
5mmol/L |
(1.8-6)mmol/L |
Creatine |
51.5umol/L |
(39-57)umol/L |
Sodium, serum |
140mmol/L |
(135-145)mmol/L |
Table 1 Initial laboratory investigation results.
Osseous and extra osseous Ewing sarcoma, peripheral neuroectodermal tumours (PNET) and Askin’stumours of the chest wall are collectively known as Ewing’s sarcoma family of tumours (EFT). EFT are heterogenous group of tumours that encompasses members who share the same histological, immunohistochemical and non-random translocations, however, differ in their clinical features.3
EFT collectively by far are rare entity accounts for 10-20% of primary malignant bone tumours. Most of the primary tumours occur in the lower extremity long bones (47%), pelvis (19%), or ribs (12%).4 Noteworthy head and neck region affection occur in only 1-4% of all cases mainly comprising of ES/PNET with predilection to adolescent and young adult group and male predominance.5,6 the most affected site are mandible and base of the skull7 followed by the orbit, and nasal cavity with or without the paranasal sinuses respectively.8
We screened the literature for cases that reported Ewing sarcoma affecting retropharyngeal in children aging from 2-14 years, no single case was found, we also screened the cases that reported the association of Ewing’s sarcoma and single kidney, no association was found.
In our case the primary site was retropharyngeal; an extremely rare site for Ewing sarcoma in an unusual age with single kidney is making the case quite unique and challenging in the context of chemotherapy protocol that contain one of the most nephrotoxic drug (ifosfamide).
In literature review we managed to find some of the cases that was reporting Ewing sarcoma in the head and neck region in sites considered rare in children aging 0-14 years old (Table 2)
First Author year(ref) |
Age(years) |
Gender |
Site |
Treatment modality |
Meer et al., 20179 |
12 |
M |
Retro-tracheal |
Chemo/radiotherapy |
Wine land et al., 201810 |
2 |
M |
Tracheal |
Chemotherapy |
Binnetoglu et al., 201611 |
2 |
M |
External ear canal |
Chemotherapy/surgery |
Table 2 Rare sites of Ewing sarcoma in head and neck region in children.
Ewing sarcoma usually responsive to multimodality therapy consisting of chemotherapy, radiotherapy and/or surgical resection for local control. Complete or even near complete surgical resection was not feasible in our case due to the sensitive site, so we decided to follow chemotherapy treatment strategy and follow up the mass conservatively for the time being and re-discuses surgical/radiotherapy option according to treatment response.
Ewing sarcoma of the head and neck particularly retropharyngeal site is a disease of a rare incidence with clinical controversy in the optimum local therapy, and whether an association of Ewing and kidney anomalies dose exist or not needs further studies in the future.
The authors have no conflicts of interest to disclose.

©2019 Almadani, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.