eISSN: 2469-2778


Case Report Volume 1 Issue 3
1Department of Laboratory Medicine, National Cancer Center, Korea
2Hematologic Oncology Clinic, National Cancer Center, Korea
3Translational Epidemiology Research Branch, National Cancer Center, Korea
4Department of Laboratory Medicine, Seoul National University Hospital, Korea
5Green Cross Laboratories, Yongin, Korea
Correspondence: Sun Young Kong, Department of Laboratory Medicine, National Cancer Center, 323 Ilsan-ro, Ilsandong-gu, Goyang-si, Gyeonggi-do, 410-769, Republic of Korea, Tel 82-31-920-1735
Received: June 23, 2015 | Published: July 28, 2015
Citation: Lee N, Lee H, Sohn J, et al. A patient with philadelphia-negative acute lymphoblastic leukemia with a FISH-negative cryptic BCR-ABL1 rearrangement detected by PCR and sequencing analysis. Hematol Transfus Int J. 2015;1(2):60-63. DOI: 10.15406/htij.2015.01.00014
The BCR-ABL1 rearrangement found in hematologic malignancies such as chronic myeloid leukemia (CML) and acute lymphoblastic leukemia (ALL). About 5-10% of patients with CML and ALL lack cytogenetic evidence of the Ph chromosome detected only by fluorescence in situ hybridization (FISH) and/or reverse transcription-polymerase chain reaction (RT-PCR) without any cytogenetic evidence of Ph chromosome. Here we describe a patient with Ph-negative ALL and a FISH-negative cryptic BCR-ABL1 rearrangement, as confirmed by RT-PCR and sequencing analyses. A 20-year-old female with Down syndrome and relapsed ALL was referred to our hospital. All 20 metaphase cells analyzed had a karyotype by conventional methods of 47, XX, +21 and FISH analysis yielded a signal for BCR-ABL1 consistent with a normal pattern. However, multiplex RT-PCR revealed an atypical band indicating the possibility of BCR-ABL1 translocation, which was confirmed by Split-out PCR, real-time PCR and direct sequencing. We revealed that this patient has a dual transcription of typical b3a2 and atypical b2a2 resulted from partial duplication of BCR exon 13, combined with ABL1 exon 2. Although cryptic BCR-ABL1 rearrangements are rare, they affect treatment regimens, making them clinically important. Precise molecular work up along with standard diagnostic tools used to detect BCR-ABL1 rearrangements are recommended for these patients.
Keywords: BCR/ABL1, RT-PCR, FISH
CML, chronic myeloid leukemia; ALL, acute lymphoblastic leukemia; FISH, fluorescence in situ hybridization; RT-PCR, reverse transcription-polymerase chain reaction; Ph, philadelphia
The BCR-ABL1 rearrangement found in hematologic malignancies such as chronic myeloid leukemia (CML) and acute lymphoblastic leukemia (ALL) results from a reciprocal translocation between chromosomes 9q34 and 22q11, and, in most patients, generates the Philadelphia (Ph) chromosome.1 More rarely, masked translocations without cytogenetic evidence of the Ph chromosome occur, with these translocations detected only by fluorescence in situ hybridization (FISH) and/or reverse transcription-polymerase chain reaction (RT-PCR). About 5-10% of patients with CML and ALL lack cytogenetic evidence of the Ph chromosome but show BCR-ABL1 translocation by more sensitive molecular studies.1,2 Nevertheless, the BCR-ABL1 fusion genes detected only by RT-PCR or sequencing analysis are extremely rare. Here we describe a patient with Ph-negative ALL and a FISH-negative cryptic BCR-ABL1 rearrangement, as confirmed by RT-PCR and sequencing analyses.
A 20-year-old female with Down syndrome and relapsed ALL was transferred to our hospital. She had been previously diagnosed with Precursor B-cell ALL with no evidence of cytogenetic abnormalities and had been treated with 8 cycles of combination chemotherapy (hyper-fractionated CVAD alternating with high-dose MTX/AraC). Her disease relapsed after 15 months, when she was referred to our institution. At referral, her hemoglobin level was 12.2 g/dL, her platelet count was 24 x 109/L, and her white blood cell count was 10.09 x 109/L, with 53% blasts, 25% segmented neutrophils, 15% lymphocytes, and 1% monocytes, and an absolute neutrophil count of 2724/µl. Bone marrow aspiration showed that small to medium sized blasts constituted more than 89% of all nucleated cells, with a reduction in trilineage hematopoiesis (Figure 1A). Bone marrow biopsy slides confirmed that her marrow was packed with immature cells (Figure 1B). Flow cytometric analysis showed high numbers of B-lymphoid lineage blasts positive for the expression of CD19, CD10, CD34, HLA-DR, and TdT (Figure 1C). All 20 metaphase cells analyzed had a karyotype by conventional methods of 47, XX, +21 (Figure 1D). FISH analysis (Abbott Vysis, Des Plaines, IL, USA), performed using commercially available locus-specific identifiers (LSI) with the BCR/ABL1 dual fusion triple color translocation probes for 22q11.2 (breakpoint cluster region) and 9q34 (ABL1 oncogene and ASS gene), yielded a signal for BCR-ABL1 consistent with a normal pattern (Figure 1E).

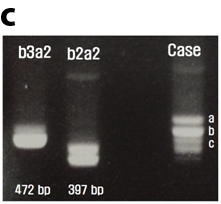
Multiplex RT-PCR using a Hema Vision kit (DNA Technology, Aarhus, Denmark) showed an atypical band in lane 6, indicating the possibility of a BCR-ABL1 translocation (Figure 2A). To confirm the atypical band in lane 6, the mRNA product was assessed by Hema Vision split-out PCR. This assay showed a positive result with three bands, of 397, 472 and 400~500 base pairs (bp) (Figure 2B). In addition, nested PCR with BIOMED-1 group primers confirmed the three bands in this patient (Figure 2C). The bands at 397 bp and 472 bp were consistent with the transcripts of b2a2 and b3a2, the products resulting from the translocations of BCR exon13 with ABL1 exon2 and of BCR exon14 with ABL1 exon2, respectively. To identify the atypical band on 400~500 bp, real-time PCR and direct sequencing were performed, with quantitative analysis by the Light Cyclert (9;22) Quantification kit (Roche Diagnostic, Mannheim, Germany). The result of normalized copy number (NCN) with IS conversion was 26.47%, which was higher than the positive control. Direct sequencing revealed that this patient had two transcripts, one of typical b3a2 derived from the translocation of BCR exon 14 and ABL1 exon 2 (Figure 3A) and the other of an atypical b2a2 resulting from partial duplication of BCR exon 13 combined with ABL1 exon 2 (Figure 3B). Figure 3C shows a schematic diagram of the suggested BCR-ABL1 transcripts. The atypical band at 400~500 bp was likely the product of dual priming on exon 13. Owing to the small size of the insertion, the BCR-ABL1 fusion transcript could not be detected on chromosomal spreads or FISH analysis, but only by RT-PCR.
In several patients, the Ph chromosome is not clearly recognizable, because of additional chromosomal rearrangements involving this chromosome that mask its typical 22q- appearance. The first masked Ph chromosome was described in 1987 in a patient with typical CML and a Ph-negative karyotype; banding studies and southern blotting using hybridization with the BglII-HindIII 5’ and 3’ bcr probe showed a standard Ph rearrangement, with secondary involvement of the 22q in a translocation with chromosome 5.3 Interphase FISH showed various patterns of BCR-ABL1 gene rearrangement, with patients having Ph-negative CML and ALL showing identical cryptic insertions of BCR at 9q34.1,4 Three patients with Ph-negative CML were found to have sequential translocations, with the initial standard Ph rearrangement followed by a second reverse translocation involving a distal breakpoint on der(22) and a proximal breakpoint on der(9).2 However, genetic rearrangements that are FISH negative but RT-PCR positive are extremely rare. Although none has been found to involve BCR-ABL1, 20 patients with PML-RARA rearrangements have been reported to date.5–7 The chromosomal translocation in our patient could not be detected by conventional cytogenetic analysis or by FISH but only by multiplex RT-PCR. Direct sequencing analysis revealed a small cryptic insertion in ABL1 exon13, resulting in a BCR-ABL1 fusion transcript. To our knowledge, this patient is the first to present with a FISH-negative but RT-PCR positive cryptic BCR-ABL1 rearrangement.
The patient was retreated with a VPDL induction regimen combined with imatinib for 30days. A bone marrow biopsy showed that blasts accounted for <5% of total nucleated cells, and molecular analysis showed a complete molecular response with 0% of IS NCN results. Although cryptic BCR-ABL1 rearrangements are rare, they affect treatment regimens, making them clinically important. Precise molecular work up along with standard diagnostic tools used to detect BCR-ABL1 rearrangements are recommended for these patients.
None.
The author declares no conflict of interest.

©2015 Lee, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.