eISSN: 2576-4497


Case Report Volume 6 Issue 2
Professor at University of São Paulo, Medicine School, Occupational Therapy, São Paulo, Brazil
Correspondence: Marilia Bense Othero, Professor at University of São Paulo, Medicine School, Occupational Therapy, São Paulo, Brazil, Tel +55 11 30917453
Received: April 19, 2023 | Published: June 22, 2023
Citation: Othero MB. Occupational therapy and end-of-life care: development of high-density foam orthosis as comfort measure. Hos Pal Med Int Jnl. 2023;6(2):32-36. DOI: 10.15406/hpmij.2023.06.00214
An orthosis is a rehabilitation device applied to a body segment (with one or more joints), whose function is to stabilize, immobilize, prevent, or correct deformities, and maximize patient functionality.However, in end-of-life care and palliative rehabilitation, changes are needed for orthosis prescription, once the main objective is comfort and symptom management. The aim of this article is to present a specific model of high-density foam orthosis developed in a Brazilian hospice for terminally ill patients, and discuss about the roles and strategies in palliative rehabilitation. This orthosis model is proposed for patients with advanced disease and no prognosis of functional recovery. It is manually made with high-density foam, cotton fabric, board velcro, EVA (ethylene vinyl acetate), hot glue, folding or electric knife. The foam is cut with the folding knife according to the required orthosis model, then covered with fabric and EVA. Board velcro is added to place the device on the patient. Positive results can be described: adherence to the use of the orthosis, minimal discomfort reported, muscular relaxation/tonus regulation, pain management and reduction of edema. Rehabilitation is an integral part of Palliative Care, and in case of terminally ill patients, comfort is the main objective of the care plan. The intervention of Occupational Therapy and the use of foam orthosis is an important strategy to achieve this goal.
Keywords: orthosis, occupational therapy, end-of-life care, assistive technology, palliative care, rehabilitation, low-cost rehabilitation device
OT, occupational therapy; AOTA, american occupational therapy association; EOL, end-of-life; EVA, ethylene vinyl acetate
Occupational Therapy (OT) intervention promotes independence and autonomy for people with disabilities, functional limitations or social exclusion.1 According to American Occupational Therapy Association (AOTA), the OT uses everyday life activities (occupations) to promote health, well-being, and your ability to participate in the important activities in your life. Occupational Therapists believe that engaging in occupations underlies quality of life and qualifies to the occupation to promote health and welfare.2 The relationship between Palliative Care and Rehabilitation has been grown in last decades3-6 with emphasis on quality of life, symptom control, relief of suffering and better use of the remaining time at end of life.3,5
The main objectives of OT in Palliative Care are:7–10 maintenance of meaningful activities for the client and their family; promotion of sensory and cognitive stimuli to enrich everyday life; implementation of comfort measures and symptom management; functional rehabilitation for autonomy and independence at activities of daily living; indication of assistive technology equipment and environmental adaptations; promotion of social interaction through group strategies and community activities and care/guidance to the family member and/or caregiver. These topics refer especially to the Brazilian context, in which a well-founded practice of OT in Palliative Care has been developed since the mid-2000s.
At the end of life, the symptom burden of a patient may worsen and require more intensive palliation. The care is based on exclusive comfort measures11 and physical, mental, cognitive, sensory and emotional wellbeing should be considered as the top priority of interventions and the OT has a major role: adequate positioning, indication of orthoses and other assistive technology devices, symptom control (such as pain, fatigue and dyspnea,) and, in addition to the use of expressive and creative activities (painting, writing, music and others)to promote quality of life and sense of self efficacy.9,12,13
An orthosis is a device applied to a body segment, covering one or more joints and whose function is to stabilize, immobilize, prevent, or correct deformities, as well as protect against injuries, assist in healing or maximize function.14,15 In Brazil, orthoses are usually made of thermoformable plastic, a rigid and hard material, which – despite excellent results in the functional rehabilitation of patients – can cause discomfort, pressure points and skin wounds in the case of terminally ill people.
The orthoses’ prescription is a role in OT intervention, and they are commonly used in orthopedics and neurological rehabilitation. In Palliative Care, the orthosis is prescribed by OT in a more cautious way, because, in practice, it is possible to observe that the most common orthoses can bring discomfort to the patient, especially at the end of life.
Cheville et al.16 mention that orthotics is underused in palliative care, with exception of control back pain devices. The authors also mention that there is little evidence base to direct the orthosis prescription, and the clinical decision making is done with palliative care principles guidance. Other studies about orthosis and palliative care mention the use of this device for functional rehabilitation17 or pain control (breakthrough pain also).18 But there is no study about this type of treatment in end-of-life care.
At this point, the orthosis can be used to promote comfort and control symptoms (not just pain, but also fatigue, and edema).8,9,12 Since 2009, a protocol has been developed for high-density foam. orthosis prescription at a Brazilian hospice, particularly for with patients with non-oncological diseases. The aim of this article is to present a high-density foam orthosis, its indications and confection/use prescriptions. It is also a way to initiate some discussion about end-of-life rehabilitation techniques.
All PC interventions require a thorough assessment from the therapist, with very well-defined objectives. Unfortunately, these are common situations: critically ill and bedridden patients; deformities that are already installed; little possibility of mobilization in bed; bone metastases; bad skin conditions (edema, anasarca, dryness, wounds); few financial resources, especially in the Brazilian reality.12 Rome et al.11 complete the description of end-of-life symptoms: skin mottling and cool extremities, mouth breathing with hyperextended neck, respiratory pattern changes, periods of deepening somnolence. Therefore, for patients with advanced or terminal illnesses, comfort is the priority of the care plan. Considering all the above arguments, it is proposed a specific positioning orthoses made of high-density foam, for patients with advanced disease and no prognosis of functional recovery.
This orthosis is manually made with the following materials: high-density foam, cotton fabric, board velcro, EVA (ethylene vinyl acetate), hot glue, folding or electric knife. The figure 01 shows the materials to be used. For spastic patients, its also used a rigid material placed behind the foam, such as thermoplastic, thin wood board or cardboard (Figure 1).
OT assessment for orthosis indication includes sensitivity, mobility, motor function, edema, tonus, pain, joint instability or limitation (such as stiffness or deformities), skin conditions and cognitive conditions. The use of board Velcro must be very strict, especially due to the association between the bad skin conditions usually found and the hot climate of Brazil. It’s suggested the board velcro use only when there is active movement of the body segment. The figures 02 to 06 show some clinical cases in which such orthoses were used (Figure 2–6).

Figure 2 Alzheimer’s elderly patient at end-of-life care. These orthoses were used for comfort, edema reduction and prevention of skin lesions on the palm hand. (Photo by author).

Figure 3 Advanced Parkinson’s disease patient. All orthosis were made with high density foam, preventing hand and deformities and also comfort positioning. (Photo by author).
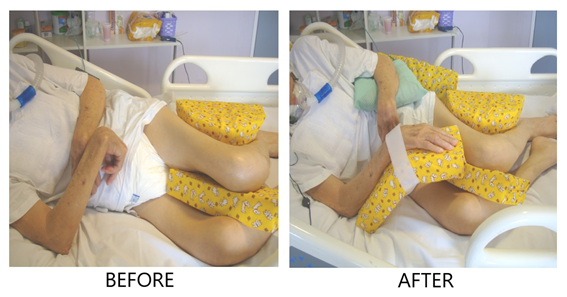
Figure 4 The same Parkisons’ patient of figure 03, showing before and after OT orthosis intervention. Pay attention at board Velcro use at hand orthosis: one is enough to maintain proper positioning. (Photo by author).

Figure 5 Stroke elderly patient, with no prognosis of functional recovery. This device were made to prevent feet deformities, but with no discomfort for the person. (Photo by author).

Figure 6 Patient with disseminated bone metastases, with humerus fracture. A Sarmiento’s orthosis was made with thermoplastic and adapted with foam for comfort measure. (Photo by author).
The protocol for using the orthosis follows some criteria, approved by the Hospital Infection Control Committee: positioning should always be done at the person's pain threshold; prioritization of nightly use; day use just be needed in severe cases, with periods of rest; pay attention to weather conditions (especially because Brazil climate, as mentioned), periodic change of coating (cotton fabric), maximum attention should be given to bony prominences, avoiding wounds and discomfort.
The occupational therapist must assess the patient on an ongoing basis. People with communication difficulties or cognitive deficits deserve special attention, with analysis of discomfort non-verbal signs. All steps to manually made the high density foam orthosis are described below, with corresponding figures. These are just sample steps, for a hand-wrist orthosis; but the high-density foam can be used to any orthosis model. The first step is cut the foam at size needed for that patient's orthosis. The respective body segment is measured in detail by the OT (Figure 7 & 8). The foam must be hollowed out or cut, and the body segment can be accommodated at the orthosis (Figure 9). The OT measures the orthosis again, check how it fits and completes the cut foam. After that, the device is covered with cotton fabric, glued or sewn only on the sides without contact with the patient's skin (Figure 10).
For finishing, the orthosis back is covered with EVA glued in the same way (Figure 11). The board velcro is attached to the side of the orthosis in its appropriate place (Figure 12). As mentioned before, attention should be paid to days in hot weather to avoid skin damage. At some cases, thermoplastic orthosis can be used, mainly in bone metastases or other kind of bone fracture. But, even in these cases, the foam can cover all equipment for maximum comfort (Figure 13). High-density foam is cheaper than specific orthoses foam, which are not accessible in Brazil.
With this intervention at the hospice, it was possible to observe several positive results in patients at the end-of-life care: adherence to the use of the orthosis, minimal discomfort reported or observed (even in cases with hypersensitivity), muscular relaxation and tonus regulation, pain control, reduction of hand/arm edema and even some cases of small range of motion gain. The high-density foam orthosis has been routinely used in the service ever since.
OT intervention at the end-of-life is very important, with numerous intervention strategies and the indication of orthoses in one of them. There are just a few studies that mention orthosis at palliative rehabilitation, but clinical experience shows that it is possible to use it with good results for the patients.
The high-density foam orthosis, following detailed criteria, can be used to promote comfort measures at end-of-life. They are prescribed, made and/or adapted by the OT for each patient, through continuous evaluation and follow-up.
High-density foam positioning orthoses have proven to be an efficient approach to prevent problems and promote comfort measures for people with advanced disease and no prognosis for functional recovery. High-density foam is also a low-cost material, allowing wide access to this device in the context of development countries such as Brazil.
It is essential to consider that occupational therapists need to make specific clinical reasoning for terminally ill patients, considering both references of rehabilitation/assistive technology and palliative intervention. This is a challenged faced by all rehabilitation professional that work in palliative care field: motor and cognitive function recovery is one of the treatment aims. Comfort, problems prevention, skin integrity and symptom management are also possible in the palliative care intervention.
High-density foam orthoses are a relevant resource for Occupational Therapy in Palliative Care. They are a viable and effective alternative to promote quality of life for terminally ill patients. As comfort measures are the priority in end-of-life care, more studies are needed to develop specific rehabilitation strategies for terminally ill patients. The proposal presented in this article is just a step towards the systematization of a more careful practice in palliative rehabilitation, focused on the real needs of users, with the affirmation of their dignity and autonomy. But its an initial one, with empirical results. More research is needed regarding orthoses in end-of-life care.
This article is the result of a orthosis prescription protocol developed by the author since 2009 as an occupational therapist in Palliative Care in Brazil. The author is responsible for all this article. The author has the copyright for all photos published here.
The author declared that there are no conflicts of interest.

©2023 Othero. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.