eISSN: 2576-4497


Case Report Volume 6 Issue 1
Universitary Children´s Hospital José Luis Miranda, Cuba
Correspondence: Miguel Ángel Cruz Díaz, Neurosurgery, Universitary Children´s Hospital José Luis Miranda, Villa Clara, Cuba , Tel +53649647
Received: June 07, 2023 | Published: June 21, 2023
Citation: Díaz MAC, Camacho-Gómez AS, Rivero CJA, et al. Intraosseous meningioma of the orbital roof. Hos Pal Med Int Jnl. 2023;6(1):29-30. DOI: 10.15406/hpmij.2023.06.00213
Primary intraosseous meningioma is a rare variety of meningioma that represents about 1% of all meningiomas Intraosseous or intradiploic meningioma of the pediatric orbital roof is reported in case reports in very isolation.. The following article is carried out with the objective of describing a case of primary intraosseous meningioma of orbital roof in a pediatric patient as well as reviewing the literature in this regard. It was concluded that intraosseous or intradiploic meningioma of the orbital roof is a rare entity. They are more frequent in males and the common age of presentation is at the beginning of the second decade of life. They usually only present with ipsilateral proptosis, without impaired visual acuity or pain. Most are histologically of the psammomatous variety and the treatment of choice is total surgical excision.
Keywords: intraosseous meningioma, intradiploic meningioma, extradural meningioma
Meningiomas are common intradural lesions that arise from cells of the arachnoid layer. In contrast, primary extradural meningioma is a relatively rare entity, accounting for less than 2% of all meningiomas.1–4 They can arise from other places, such as the skin, orbit, nasopharynx, and neck. Primary intraosseous meningioma, which arises in bone, is a subset of primary extradural meningioma, and only a few cases have been described.5
The minimal or complete absence of dural involvement in primary intraosseous meningioma makes establishing an accurate diagnosis challenging, where differential diagnosis may include fibrous dysplasia, Paget's disease, and other lesions.6 Intraosseous or intradiploic meningioma of the pediatric orbital roof is reported in case reports in very isolation.These tumors are mostly seen within the first two decades of life and histologically are usually of the psamomatous variety.7–12 The following article is carried out with the objective of describing a case of primary intraosseous meningioma of orbital roof in a pediatric patient as well as reviewing the literature in this regard.
Male patient, 12 years of age, health history. He comes referring to having started a month before the consultation with protrusion of the right eyeball, painless and that does not cause loss of visual acuity. Examination revealed right ocular proptosis, without affecting ocular motility or visual acuity. Fundus without alterations.
CT scan of the skull and orbit is performed where it is reported: towards the right orbital roof, with a wide dural and intraosseous base, there is a homogeneous hyperdense [250 UH] occupant lesion with well-defined, regular contours, showing peripheral calcification [588 UH] inside and center of lower density, measuring in axial cut 30x25mm, with craniocaudal extension of 23 mm. This lesion shows superior growth, with ipsilateral basal fronto extension, as well as intraconal, refines the cortical of the orbital medial wall without eroding it, contacts the superior rectus muscle, as well as with the upper edge of the eyeball and the optic nerve at its upper end, without infiltrating them. It causes protosis of the right eyeball (Figure 1).
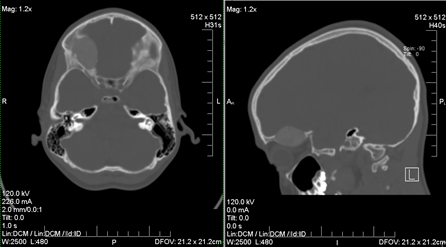
Figure 1 Computed Axial Tomography image shows where it can be seen in axial slices and sagittal reconstruction intradiploic occupative lesion of the right orbital roof.
It is decided to indicate MRI where it is reported: Space occupying lesion in the right extraxial orbital roof with wide dural base that behaves isointense to the white matter in T1, hypointense in T2 and FLAIR, with small area of signal cancellation towards its external portion, in relation to calcification at this level, of well-defined contours, regular measuring in axial cut 24x26mm, with caudal skull extension of 21 mm. This lesion shows superior extension towards the right frontobasal region, as well as inferiorly towards the intraconal region, occupying the retrobitary fat, contacts the posterosuperior portion of the eyeball, the superior rectus muscle and optic nerve preserving interfaces with them, causing profusion of the right eyeball. Other normal structures. After clinical and imaging evaluation, it was decided to intervene surgically performing total excision of the lesion. Histological report is received that reports: Psammomatous meningioma (Figure 2).
Primary intraosseous or intradiploic meningioma is a rare variety of meningioma that accounts for about 1% of all meningiomas.13,14 Marwah et al.15 defined a meningioma that develops in the skull as a primary intraosseous meningioma and the diagnostic criteria included lesions which have the histological features of a meningioma; lesions located in the epidural or skull region; and without involvement of brain, arachnoid or dura mater tissue.15,16
Lang et al.17 classify primary extradural meningioma into three categories. Type 1 (purely extra-calvary), Type 2 (purely calvary), and Type 3 (calvary with extra-calvary extension). Types 2 and 3 can be subclassified into B (convexity) and C (skull base). According to this classification system, the case presented in this article is classified as Type 2C.1,5,14,17
The exact origin of these tumors is controversial, and many hypotheses have been proposed. The most acceptable is the entrapment of meningocytes or arachnoid cells in cranial sutures during molding of the skull at birth and neural embryogenesis. Other theories also accepted are cellular dedifferentiation of abnormal cells in the diploic space and the implantation of arachnoid cells during mechanical trauma. In most cases there is no history or demonstrable cause.1,5,12,14 Within the variety of intraosseous meningiomas, those that develop in the orbital roof are infrequent; the few cases reported in the literature are more frequent in males and in young people, and the common age of presentation was at the beginning of the second decade of life which agrees with the case presented in this article.12 All the cases described, including this case were presented only with exophthalmos on the side of the tumor; no pain or impairment of visual acuity was reported at diagnosis of the disease.12,14
Coronal and lateral tomography images are necessary to clearly demonstrate intradiploic involvement of the roof of the orbit. Radiologically, intradiploic meningiomas may be osteoblastic or osteolytic; however, mixed versions have also been reported. It usually shows an osteoblastic or hyperostotic reaction in the form of granular or mottled calcification involving the roof or wall of the orbit. Osteolytic lesions typically cause thinning, expansion, and disruption of the internal or external tables of the skull, and these lesions also enhance homogeneously after contrast administration. However, computed tomography can reveal the intradiploic location of the meningioma but MRI may show better delimitation of the extent of the meningioma and involvement of adjacent soft tissues.14,18
Intradiploic meningiomas should be considered in the differential diagnosis of patients presenting with osteoblastic or osteolytic cranial lesions. Intradiploic orbital roof meningioma differs from intraorbital meningioma in clinical presentation and radiologic features. In addition to proptosis, visual loss is also a common presenting feature in intraorbital meningioma. Common differential diagnoses would include fibrous dysplasia and osteoma .The osteoblastic variety causes hyperostosis, which can mimic fibrous dysplasia and solitary osteoma. Another lesion to take into account in the differential diagnosis is chondrosarcoma, the latter progresses rapidly, sometimes it canoccur in the orbital wall, it is known for its aggressive behavior with a high recurrence rate and causes distant metastasis.12–14,18 Most of these tumors are benign but malignant transformation is also described. The histological picture in most of the cases reported so far, including this case, revealed a psammomatous meningioma with invasion of the bone by meningiomatous tissue.12 The treatment of choice is total surgical excision, which is generally possible since these tumors are enclosed in a bony shell.15
Intraosseous or intradiploic meningioma of the orbital roof is a rare entity. They are more frequent in males and the common age of presentation is at the beginning of the second decade of life. They usually only present with ipsilateral proptosis, without impaired visual acuity or pain. Most are histologically of the psammomatous variety and the treatment of choice is total surgical excision.
None.
The authors report no conflicts of interest.

©2023 Díaz, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.