eISSN: 2576-4497


Case Report Volume 7 Issue 1
Universidade de Uberaba, Uberaba, Minas Gerais, Brazil
Correspondence: Giovanna Schroden Rodrigues, Universidade de Uberaba, Uberaba, Minas Gerais, Brazil
Received: January 30, 2024 | Published: February 12, 2024
Citation: Rodrigues GS. Clinical presentation and therapy for Epiphrenic diverticulum - Case report. Hos Pal Med Int Jnl. 2024;7(1):12-15. DOI: 10.15406/hpmij.2024.07.00231
Epiphrenic diverticulum is a rare pathology characterized by anomalous protrusions in the esophagus resulting from an increase in intraluminal pressure which leads to herniation of the mucosal and submucosal layers. Although the clinical picture is insidious, patients can manifest symptoms such as dysphagia and chest pain. We therefore present a literature review and a case report of a symptomatic patient whose case was resolved by surgery.
Keywords: diverticulum, esophagus, epiphrenic, therapeutics
Esophageal diverticula are divided into cervical (pharynx esophageal) and middle and lower third (epiphrenic). Epiphrenic diverticula are abnormal saccular protrusions of the esophageal lumen through the muscular layer, caused by an increase in intra esophageal pressure, and are commonly linked to esophageal motor disorders. They are considered false diverticula because they only affect the mucosa and submucosa, and are very rare.1 The incidence of esophageal diverticulum can vary between 0.001 and 0.11% in the population, with Zenker's being the most common, accounting for 90% of cases. It is three times more prevalent in women. The pathology presents itself from the 6th decade of life onwards, with a higher incidence between the ages of sixty and ninety. Due to the large number of undiagnosed patients, its prevalence estimate is prejudiced, and it is more common in the United States, Canada and northern Europe.2 The prevalence of epiphrenic diverticulum in the United States is 0.0015% and in Europe 2%, but its true incidence is unknown since the majority of affected patients are asymptomatic, around 80%, and are diagnosed randomly through radiographs and endoscopies performed for other reasons.3 The etiology of the diverticulum is associated with motor disorders of the HAZ (high pressure zone), i.e. hypertonia of the HAZ leading to increased internal pressure, favouring herniation of the mucosa at any insertion point of vessels in the lower esophagus.4 Esophageal diverticula are classified according to their location and pathophysiological characteristics into three different types: Zenker's diverticula, Rokitanski's diverticula and Epiphrenic diverticula. Zenker's diverticula, also called pharynx esophageal diverticula or pharyngeal pouches, affect the proximal region of the esophagus and are pseudo diverticula, as they have no evaginated muscle layer, only the mucosa and serosa. Rokitanski's diverticula occur in the middle third of the esophagus and manifest themselves as true diverticula, since they are evaginations of all the muscular layers of the esophagus.
Layers of the esophageal wall. Epiphrenic diverticula, also known as supradiaphragmatic diverticula, are located in the distal third of the esophagus and appear as pseudo diverticula, i.e. without a muscular layer.4 Zenker's diverticula are pulsing diverticula related to an increase in intraluminal pressure in the esophagus associated with a reduction in the compliance of a segment of the organ wall. Rokitanski's diverticula, on the other hand, are traction diverticula caused by previous thoracic inflammatory processes, which adhere to the organ and pull it, generating the diverticulum.5 Epiphrenic diverticula are pulsion diverticula, resulting from dysfunctions in the motility of the esophagus.4–6 Epiphrenic diverticulum is diagnosed by the sum of several factors, such as the patient's clinical history, contrast radiography, manometry which indicates motor alterations, and upper digestive endoscopy which will serve to rule out other diagnoses.7 In addition, the best way to confirm the presence of this diverticulum is by contrast radiography of the esophagus, which will also show the presence or absence of alterations in the patient's esophageal motility.8 Treatment of this type of esophageal diverticulum depends on the presence of severe symptoms or complications, such as inflammation, fistulas, perforations into the mediastinum and bleeding.1 So, when we have a symptomatic patient or with the presence of any of these complications, surgical treatment can be performed, with a left or right thoracotomy (depending on the projection of the diverticulum), performing its resection. In addition, if there is dysmotility, an anti-reflux Nissen valve can be performed to prevent gastroesophageal reflux disease.8 Another possible approach is through a laparotomy, a less invasive technique with less morbidity than a thoracotomy.4 This case report aims to report in the literature a case of herniation that preferentially affects the distal part of the esophagus, named Epiphrenic Diverticulum, in order to provide guidance and more information on the pathology.
This is a report of a 53-year-old woman who sought medical attention complaining of progressive postprandial regurgitation for a month, with recurrent choking. She reported precordial pain when coughing and regurgitating. He also reported dysphagia and dyspepsia at the same time. The regurgitation worsened during the night at bedtime when he felt acid reflux, which improved when he stood up. The patient reported starting with simple eructation’s, followed by frequent regurgitation and choking after eating. Finally, the patient reported worsening obstructive sleep apnea, which was more frequent in the left lateral decubitus position. She denied vomiting or nausea, asthenia, headaches or any other complaints. He had been taking acetyl salicylic acid 100 milligrams once a day after lunch due to a diagnosis of polycythaemia since 2014. As for her other personal history, the patient reported a caesarean section and a tubal ligation, both without complications, and denied blood transfusions. She denies smoking and reports social drinking at weekends. Her father had a history of surgery for a stomach ulcer.
On physical examination, the patient was in good general condition, self and Self-oriented, mucous membranes red, hydrated, anicteric and a cyanotic, with no palpable lymph nodes in the submandibular, cervical or other chains, a normal palpable thyroid, with a fibro elastic consistency and painless on palpation. Respiratory system with preserved vesicular murmur without adventitious noises, preserved lung expansion and tympanic percussion. Cardiovascular system with rhythmic, normal-sounding sounds in two clicks with no murmurs or crackles. Carotid, radial, femoral, pedicle and popliteal pulses were broad and symmetrical with no alterations. Gastrointestinal tract with preserved hydro aerial sounds, painless on superficial and deep palpation. Lower limbs without edema. Physical examination without noteworthy alterations. After the consultation, laboratory and imaging tests were requested for further diagnostic elucidation in the suspicion of Gastroesophageal Reflux Disease (GERD), the presence of a diverticulum or gastric ulcer. These included video upper digestive endoscopy, esophageal manometry, pH monitoring, total abdominal ultrasound, digital chest X-ray and abdominal X-ray.
An upper digestive endoscopy was carried out one month after the first consultation, in which the presence of a diverticulum 35 cm from the incisors (in the lower third), with food content, was observed in the esophagus. The mucosa was unchanged and the vascular pattern was preserved. In addition, the esophago gastric transition, located 40 cm from the incisors, coincided with diaphragmatic clamping and was within normal limits. The results for the stomach showed a normal shape, volume and distensibility of the organ. There was also a small amount of hyaline stasis fluid in the usual colour. The mucosal fold and antral peristalsis were preserved. The retro vision manoeuvre showed the hiatus adjusted in relation to the endoscope and visualized some flat erosions in the gastric antrum mucosa, with a centered and patent pylorus. In the duodenum, the bulb had a preserved lumen and mucosa, and the second portion had intact folds and mucosa. A biopsy of the gastric mucosa was also taken for urease testing, with negative results for Helicobacter pylori. Diagnostic impression: esophageal diverticulum with food content at 35 cm from the incisors and mild erosive antral gastritis (Figure 1). Esophageal manometry, a test that assesses the pressure tone and motility of the esophagus, was carried out 2 months after the first visit and showed the upper esophageal sphincter situated 17 to 20 cm from the nostril with an extension of 3 cm, a mean respiratory pressure at rest of 35.3 mmHg and normal relaxation. The body of the esophagus showed asynchronous peristalsis. The average amplitude was 10 wet swallows at 03 cm above the IES of 81.7 mmHg. The lower esophageal sphincter, located between 39.5 and 45.5 cm from the nostril, was 6.0 cm long, with a PIP of 42.5 cm from the nostril, and was predominantly intra-abdominal. In addition, mean respiratory pressure (MRP) at rest was 33.5 mmHg and relaxation was normal.
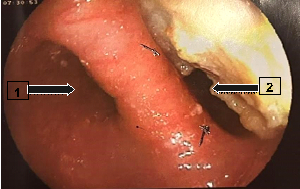
Figure 1 Upper digestive endoscopy findings. Arrow (1) Esophageal lumen, Arrow (2) epiphrenic diverticulum in the esophageal lumen.
Manometric examination within normal standards. pH-metry, a test that captures any reflux episodes, assesses the pH, intensity, duration and time of occurrence, generating a Meester constant that is above 14.72, indicating GERD. In this test, the patient scored 85.2 on the Meester table, and was diagnosed with orthostatic predominant mixed reflux. In the abdominal ultrasound requested after the first consultation, no alterations were found, as well as in the chest X-ray performed after 2 months. An X-ray of the esophagus, stomach and duodenum (Figure 2), taken the following month after the first consultation, showed the presence of a bulky distal para esophageal diverticulum with debris inside and constant diverticulum esophageal reflux. The stomach and duodenum emptied normally, with no signs of organic damage. After analysing the tests, the patient returned to the office to discuss her diagnosis and treatment. With regard to the treatment of this pathology, surgical treatment is not only indicated due to the presence of the diverticulum, it must be weighed up against the potential risks and benefits of surgery, taking into account the severity of the patient's symptoms and the complications associated with the disease.9 Surgical treatment, when indicated, should focus on motor dysfunction and resection of the diverticulum. The approach should be laparotomy, a less invasive technique with lower morbidity compared to thoracotomy. In addition, a myotomy should be performed to reduce esophageal motor disorders and a partial fundoplication in order to avoid esophageal reflux disease.4
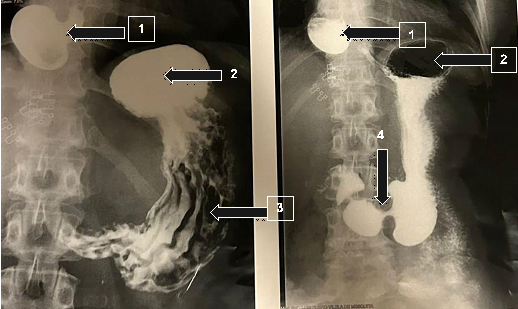
Figure 2 Contrast-enhanced radiography of the esophagus, stomach and duodenum. Arrow (1) epiphrenic diverticulum with contrast inside, Arrow (2) Gastric fundus, Arrow (3) Gastric folds, Arrow (4) Pylorus.
Once the patient's case had been discussed, with an indication for surgical treatment, the procedure was carried out using laparoscopy, which is usually used to approach the Esophagogastric transition, to correct the patient's diverticulum, without any complications 3 months after the case was first investigated, at the São Marcos Hospital in Uberaba, Minas Gerais, with a satisfactory result and a significant improvement in obstructive sleep apnea and gastrointestinal symptoms. The procedure involves making small incisions in the abdominal wall, through which surgical instruments and the laparoscope are inserted. The surgeon uses the laparoscope to visualize the area to be operated on, and after dissecting the diverticulum, it is resected using a linear endo grammar. The year after the procedure, the patient returned for a follow-up visit, reporting a significant improvement in her previous symptoms. She only complained of persistent heartburn in the epigastric region, which led to a request for a new upper gastrointestinal video endoscopy (Figure 3), which again showed a negative result for H. Pylori (using the urease test), a linear scar at 35cm from the incisors, and a persistence of erosive antral gastritis, identified in the previous year's examination, before the surgical procedure, which led to the conclusion that the erosive antral gastritis was not related to the presence of the diverticulum. As a result, clinical treatment with a proton pump inhibitor was prescribed, with a satisfactory result in the patient's clinical improvement (Figure 4, Figure 5).
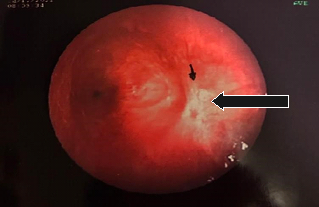
Figure 3 Post-operative upper digestive endoscopy findings. Arrow: scar where the diverticulum was repaired.
After studying the case and reviewing the literature, we realized that epiphrenic diverticula are being seen less and less. This is due to the fact that they often go unnoticed due to the absence of a clinical picture, with asymptomatic patients, or the occurrence of a mild picture that is not noteworthy. The patient in question stood out for her exuberant clinical condition, which interfered with her daily activities. Her symptoms were typical: regurgitation, dysphagia, cough, chest pain and/or epigastric, but no vomiting or halitosis.1 However, this case was relevant due to the presence of obstructive sleep apnea, more frequent in the left lateral decubitus position, which improved after definitive treatment with video laparoscopic diverticulectomy surgery, a factor previously not commonly described as a sign present in patients with epiphrenic diverticulum. Furthermore, when the patient was investigated using upper digestive endoscopy and manometry, she did not show thickening of the distal esophageal muscles or an increase in intraluminal pressure, nor did she show hypertonia, signs often found in the diagnosis of the disease.7 With regard to the patient's findings, a predominantly orthostatic reflux was diagnosed based on pH monitoring, which scored 85.2 on the Meester table. The score in question is based on the number of prolonged refluxes, number of refluxes, presence of the longest episode, total time of acid exposure, time of acid exposure while standing and lying down.10
The diagnosis was characterized by the patient's clinical signs, including dysphagia, dyspepsia, postprandial eructation and frequent choking. Given the presence of diagnosed reflux, it is understood that erosive antral gastritis on upper gastrointestinal video endoscopy was a finding, but that it is not related to the diverticulum. On the other hand, this was not the case after the surgery, since after the operation the patient reported a complete improvement in her reflux and its symptoms, with only a persistence of heartburn and a finding on an imaging test that still showed gastritis one year after the operation, making it possible to infer that this was just a condition that did not correlate with the diagnosed reflux or the epiphrenic diverticulum. With regard to this condition found through the complaint of continuous heartburn associated with persistent erosive antral gastritis, it was necessary to use medication to relieve the symptom, using a proton pump inhibitor, whose mechanism of action is to act on the H+/K+ ATPase enzyme, blocking acid secretion from the stomach. Because of this, the outcome of most patients complaining of heartburn due to an acidic pH ceases after using the medication indicated, as well as being a drug that, associated with behavioural and dietary changes, prevents gastritis from developing, as in the case of the patient in question.11
Therefore, this study deals with a case of epiphrenic diverticulum, which is a rare pathology with few cases described in the literature. Of these few, most correspond to patients over 60 years old, asymptomatic and whose esophageal alterations result from esophageal motility dysfunctions. Thus, the present case is highlighted, given that the patient was 52 years old, manifested not only the typical clinical picture, but also obstructive sleep apnea as a result of the diverticulum and had a manometric examination within normal standards, with no changes characteristic of the disease, such as hypertonia, thickening of the distal esophageal musculature or increased intraluminal pressure. Therefore, after the diagnosis was clarified, he received the appropriate indication and benefited from laparoscopic surgical treatment of the condition, showing an improvement in his symptoms and quality of life.
We declare that the patient approved the study by signing an informed consent form and the study followed the ethical guidelines established by the Declaration of Helsinki.
None.
The authors declare that there are no conflicts of interest.

©2024 Rodrigues. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.