eISSN: 2576-4497


Case Report Volume 4 Issue 2
1Palliative Medicine Consultant, Isabel Hospice, Alison StirtonCroft, Physiotherapist, UK
2Palliative Medicine Specialty Doctor, UK
Correspondence: Dr Sheraz Majeed, Palliative Medicine Consultant Isabel Hospice, Welwyn Garden City, Hertfordshire, UK , Tel +447787437775
Received: April 21, 2020 | Published: April 28, 2020
Citation: Majeed S, Bartlam K. A case study: highlighting the importance of multidisciplinary working in palliative care for a patient with psychological trauma. Hos Pal Med Int Jnl. 2020;4(2):46-49. DOI: 10.15406/hpmij.2020.04.00185
This case report illustrates how fundamental and powerful a true multi-disciplinary team (MDT) approach towards palliative care can be. The patient, an 88 year old lady, was transferred to the in-patient unit (IPU) from hospital having been diagnosed only 3 weeks earlier with the very poor prognosis of B-cell lymphoma with large mediastinal mass. Unfortunately this patient had a complex psychiatric history, which had resulted in a mistrust of healthcare professionals generally.Using an holistic approach, her needs and goals were identified and incorporated into her care planning. By having very open, honest advanced care planning discussions, which until admission had been avoided due to concerns of provoking a severe anxiety episode, the fears of death and dying that she carried could be demystified.Counselling and psychological support played an important role, as did the supportive and caring environment within the hospice more generally. She commented that this allowed her to feel nurtured, and the calmest and happiest she had been in her life. Thus, this holistic MDT approach had enabled her to “live” a better life even as she was dying. This case study looks in more detail about the ways in which this remarkable outcome was achieved.
Keywords: multi-disciplinary team, physiotherapy, psychological support, relaxation, rehabilitative palliative care
The multi-disciplinary (MDT) approach to palliative care is essential to ensure a genuinely holistic approach, with no one set of professionals alone being able to meet all the needs of complex palliative patients. Hospice UK’s definition of hospice care incorporates this concept,1 stating “Hospice care is provided by multi-disciplinary teams of staff and volunteers who offer expert support that places equal emphasis on someone’s clinical, physical, emotional, social and spiritual needs with the understanding that everyone will be different.”Further, as noted in the National End of Life Care Programme (2013),2 ‘an inter-disciplinary team (IDT) can be a highly effective vehicle … delivering integrated, person-centred end of life care. As well as harnessing a wide range of essential expertise, the IDT is greater than the sum of its parts and it offers its own ‘added value’ to end of life as seen in Figure 1.
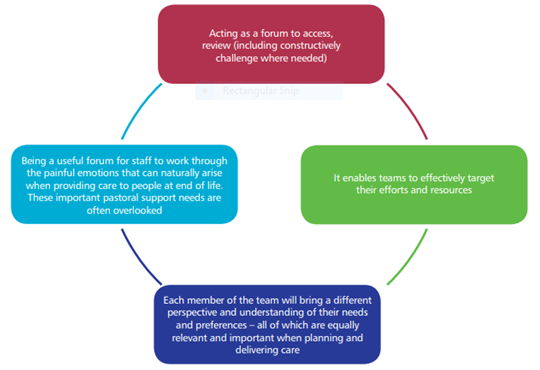
Figure 1 Benefits of interdisciplinary team working in end of life care.
Source: NHS National End of Life Care Programme (2013). (2)
The value and power of the MDT approach is illustrated in this case report, whereby a lady who has suffered for a large part of her life with severe mental health issues, is admitted to the Hospice IPU following a very recent diagnosis of B-cell lymphoma, with a mass that potentially could obstruct her airways at any point, with the associated anxiety this is likely to provoke. It can be seen how the MDT team is not only able to help support this lady, but the supportive holistic care given allowed her to flourish, even as she approached the end of her life, enabling her to feel more positive and happier than she had for many years.
Ms IC was an 88 year old lady who was transferred from a general hospital to the hospice for symptom control and possible end of life care, following a diagnosis only three weeks earlier of “B-cell lymphoma with large mediastinal mass”. She had suffered from progressive weight loss and night sweats for a couple of months prior to being admitted to hospital with stridor and shortness of breath. The CT scan showed a large mediastinal mass with narrowing of the tracheal lumen and proximal superior vena cava (SVC). The biopsy confirmed B-cell lymphoma. She declined any oncological treatment, but regardless she had also been declared not fit enough.She was at high risk of airway obstruction, had declined rapidly and her prognosis by the palliative care team at the hospital was short weeks.
On admission to the hospice, it became clear that Ms IC had a very complex psychiatric history which included ECT for depression and hospitalisation for severe anxiety, which had unfortunately led to a distrust of healthcare professionals generally. She had minimal other co-morbidities of significance. She lived alone with her dog, and was a proudly independent lady, who had worked until her mid-70s. We felt this lady was likely to require a huge amount of psychological support, and to this end we referred her to our clinical psychologist, also to family support. Given this, we applied for funding for her to stay in the unit as in addition, we felt her prognosis was likely to be short and the hospice was her preferred place of death.Our initial management, in addition to psychological and spiritual support, also included low dose oxycodone for shortness of breath, benzodiazepines as needed for anxiety, physiotherapy, complementary therapy and a crisis pack in the event of tracheal obstruction.
Ms IC improved significantly with the care and support she received from the MDT team in the hospice and within two weeks she felt less short of breath, had been weaned off oxygen and felt much less anxious. Her improvement continued such that she went on to regain her independence with a good daily routine. She even managed to visit her husband’s grave which was a huge achievement given she had been virtually bedbound for three weeks when in hospital. She had a very good Christmas and said she had “never felt more nurtured”. She plateaued for another couple of weeks before she began to deteriorate as the disease advanced.She was put on the “end of life protocol” and appeared very comfortable. She died peacefullythree days later, over ten weeks after her admission, with her two daughters by her side.
Multi-disciplinary patient management
Within the palliative care field an holistic approach to care is essential. There are a wide variety of professionals working within the in-patient unit, all playing a special and unique role in the management of a patient approaching the end of their life. From doctors and nurses, physiotherapists, occupational therapists, counsellors, complementary therapists, PET therapy, chaplaincy, ward clerks, kitchen staff, domestic staff and volunteers each will establish a different but important relationship with a patient. It is then coming together for weekly multi-disciplinary meetings that then enable professionals to share interactions and decision making to ensure any issues are addressed and a common goal is achieved. It has been recognised that blurring of boundaries is inevitable3 which is therefore why multi-disciplinary collaboration is essential to provide seamless care.
Non-pharmacological approaches
Within the MDT frequently breathlessness can be difficult to manage, therefore non-pharmacological management approaches by allied healthcare professionals must be considered, and are effective, especially for the mobile patient.4 Due to the breathlessness this lady experienced, different techniques were used such as positioning, fan therapy, and guided imagery to aid relaxation. This not only helps with the management of breathlessness but also helps focus on reducing the psychological distress caused by breathlessness for a lady who had extensive psychological history.
When using positioning as a management technique ideally the patient should adopt an upright position, and check their posture. This lady was very keen to remain active, independent and out of bed which will have aided her. Appropriate support with pillows under the arms in sitting will help to reduce the tension which can be caused by straining accessory muscles. Taylor5 reminds us of the importance of extending the distance from groin to chin as a good rule to help with managing breathlessness through positioning.
Some positions such as forward leaning were also taught to this lady, and the concepts of rectangular breathing. The aim of these techniques is to ensure efficiency of the diaphragm and reducing hyperinflation through elongating expiration.
Relaxation and guided imagery were very helpful for this lady. It enabled her to be transformed back to enjoyable holidays with her late husband which bought great joy and pleasure to talk about.
The lady whilst an inpatient had limited access to her beloved dog, however where possible seeing him was facilitated. There are no restrictions on having pets in the hospice (within reason) in fact, at times it is actively encouraged to aid psychological comfort. There are many documented benefits of pets, including suggestions by psychologists that gloom of individuals with reactive depression can be lifted with animals.6 At the hospice a PET therapy dog visits on a weekly basis. This lady was able to have joy in seeing this dog when her dog was unable to come in. She was also able to build a rapport with the therapist attending with the dog.Geisler7 notes that ‘pets in nursing homes have been associated with decreased psychotropic medication usage’. This can be thought to be particularly helpful when rationalising medications at the end of life, especially if a patient is compromised in ability to take prescribed medications.
Rehabilitative palliative care
Whilst the phrase rehabilitative palliative care may seem at odds with the ideas of end of life care this is not a new concept. There is much documented about the benefits of maintaining strength and independence for palliative care patients including reducing the burden for the caregiver, improving overall quality of life satisfaction, pain management, anxiety reduction, and breathlessness management as well as other benefits.8
For this lady who described herself as fiercely independent, maintaining control over her life was extremely important.Whilst at times having episodes of stridor and severe shortness of breath due to the tumour compressing the trachea, this lady persevered and made active decisions about her daily activities.
The lady expressed her routine of having a lay in, getting up daily, washing and dressing and accessing the day room and choosing her time for turning out the light at night time. This lady had a deep rooted distrust of healthcare professionals due to long history of institutionalisation for mental health disorders and ECT treatment at a younger age so maintaining independence and facilitating control was essential in building a trusting relationship with her.
Through working in partnership with the MDT and the patient her wishes and needs could be voiced and upheld.This aided increased trust and relaxation within the hospice setting.
The lady was provided with a 4 wheeled walker to aid her mobility, pacing, decreasing the difficulties with carrying an oxygen cylinder and providing her with the chance to use the seat on the walker to recover any breathlessness.
As the patient progressed through her stay in the in-patient unit her decline in function was apparent. This led to the lady at times displaying anger as a direct result.However, it is also felt that when a patient is allowed to experience a natural decline in function this can aid acceptance of condition change and approaching death.
Psychological history at end of life
This lady had an extensive history of struggles impacting upon her mental health. From intra utero abuse, to witnessing abuse towards her mother from an alcoholic father this patient reported she never had a happy life.
Growing up in the war and being evacuated the patient voiced that she did not like her childhood, and did not like occasions such as Christmas. As a young adult the patient had been sectioned and endured ECT treatment, then latterly (3-4 years prior to IPU admission) she had been readmitted to a mental health institute and experienced further trauma from this admission.It led over the years to a deep distrust of the health professionals and a fierce independence.
Whilst reporting a happy marriage the patient struggled with the death of her husband whilst he was in hospital.The patient was able to have an outing whilst in the IPU and went to visit her late husband’s grave on their wedding anniversary.
The removal of her wedding ring approximately a week before she died had bought about further calm. The ring was to be joined with her husbands as a gift for her granddaughter.
As her admission progressed the patient was able to increase trust in those who were caring for her. She reported she felt nourished and the happiest she had felt throughout her life. Her daughters were able to have open conversations and the patient could share things which they had never known. The neutral environment and diminished daily responsibilities of life whilst being supported in the IPU were enabling for honesty and open communication. The daughters were filled with mixed emotions, upset that it had taken such a long time in life for their mother to be happy, however pleased for her that at least this could be found.
As the patient exhibited a decline in function and death was approaching the frustrations and limitations that she was faced with became apparent leading to aggression toward staff trying to provide care for her. By working closely as an MDT the different professionals were able to share this and the behaviour of the patient was not tolerated. The lady recognised that her behaviour was unjust, however being exhibited due to fear and lack of control.
Due to the historical complexities of the mental health problems this patient had in the past a clinical psychologist was sought, however unable to be accessed in the local setting. The patient could access local counsellors, plus the nurturing and time taken by the palliative care team however show the importance of good psychological care in this setting. The value of the interventions provided by all can therefore never be underestimated and whilst seemingly small gestures they can have a profound effect on enabling a patient to feel at peace.
Advance care planning
Establishing individual wishes of a patient in relationship to escalation plans as medical status change, preferred place of care and wishes in dying are extremely important. It is reported by Detering et al.9 that advance care planning and end of life discussions reduce stress, anxiety, and depression in surviving relatives. This is always the aim to be addressed within the IPU setting.
Hospices can be approached with a massive stigma and preconceived ideas of what might happen. Frequently these are myths and it is essential to establish clear and open dialogue with the patient and those who they consent to have their wishes discussed.
Due to the historical fragile mental health of this lady her daughters were keen to shield any end of life conversations with her. They were concerned that this might evoke anxieties which had been present for most of their mothers’life.
Exploring the patients’ fears of death enabled professionals to understand fears she had of being buried alive, and the fear of feeling as though she was drowning when dying.
Whist prognostication is difficult to be exact, discussions of how the end of life may be experienced alleviates some of this anxiety.
Through maintaining open channels of communication in a non-judgemental and safe environment the patient was able to relax. She expressed feeling calm and the happiest she had been in her life. The patient was able to speak openly with her daughters and they felt they were given the opportunity to talk about things they didn’t even know.
As discussed above, the importance of the MDT on the psychological wellbeing of the patient should never be underestimated. By enabling a patient to express their wishes, maintain activity levels and feel nourished by the MDT then even when a patient has had complex mental health issues the supportive palliative care environment can help to bring peace where there was none, even at the end of life. It can also be seen that non-pharmacological interventions including relaxation, maintaining daily activities and open advanced care planning are also incredibly valuable in the holistic care of the patient. It is the consistent, positive contribution from everyone, however small, within the caring hospice environment that when combined, is ultimately what makes the difference.
The authors of this paper have no conflicts of interest to declare.
None.
None.

©2020 Majeed, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.