eISSN: 2576-4497


Introduction: The misuse of drugs among students has become a serious problem. In economically deprived countries most episodes of illness are treated by self medication. Major problems related to self medication are: wastage of resources, increased resistance of Pathogens, and generally entails serious health hazards such as adverse reaction and prolonged suffering.
Objective: To assess the prevalence and associated factors of self medication practice among non health professional students of university of Gondar, Northwest Ethiopia.
Methods: Institutional based cross sectional study was carried out on 607 non health professional students of university of Gondar; Stratified systematic random sampling technique was employed. A structured and pretested self-administered questionnaire was used to collect data, the collected data were entered using Epi-info version 3.5.3 and SPSS version 20 were used for data entry and analysis respectively.
Results: A total of 607 students were participated giving a response rate of 98.02%. From the respondents 226(38%) practiced self medication. The common perceived illnesses reported were headache/Fever 127(56.19%), abdominal pain 59(26.10%) and respiratory tract infections 35(15.48%). Males were two times more likely to practice self medication (AOR: 2.00, 95% CI: 1.41-2.86) than females.
Conclusion: The prevalence of self medication among non health professional students is high. In the bivariate and multivariate logistic analysis males were two times more likely practiced self medication than females, and being students from college of Business and economics are 61.5% less likely to practiced self medication than Technology students.
Self-medication is defined as the selection and use of non-prescription medicines by individuals’ own initiatives to treat self-recognized illnesses or symptoms. This includes acquiring medicines without a prescription, resubmitting old prescriptions to purchase medicines, sharing medicines with relatives or members of one's social circle or using leftover medicines stored at home. Medicines for self-medication are often called as non-prescription medications or over-the-counter (OTC) drugs. These medicines can be obtained through pharmacies and are also available in supermarkets or any convenience stores in some countries.1,2
In most illness episodes, self-medication is the first option which makes it a common practice worldwide. In the treatment of minor illness, when problems are self-limited, self-care can be used. The criteria for considering health problems as a minor illness include having limited duration and being perceived as nonthreatening to the patients. For government institutions, this can reduce costs while allowing health professionals to focus on more serious health problems.3
Major problems related to self medication are wastage of resources, increased resistance of Pathogens, drug resistance and generally entails serious health hazards such as adverse reaction and prolonged suffering. Antimicrobial resistance is a current problem worldwide particularly in developing countries; easy availability of wide range of drugs including antibiotics coupled with inadequate health services result in increased proportions of drugs used as self-medication compared to prescribed drugs. There is also the potential for misuse and abuse of such products and there is much public and professional concern about the irrational use of drugs.4–6
The type and extent of self -medication and the reasons for using it may vary from country to country. The prevalence rates are high all over the world; up to 68% in European countries, while much higher in the developing countries with rates going as high as 92% in the adolescents of Kuwait, 59% in Nepal and 31% in India. In majority of economically deprived countries, nearly 60-80% of health related problems are treated through self-medicated as lower cost alternative.7,8
To our best of knowledge, there is no research conducted to reveal the extent of this problem among non-health professional students of university of Gondar. Therefore, the main objective of the current study is aimed to assess the prevalence of self medication and its associated factors among non health professional students of university of Gondar, Northwest Ethiopia. Because we believe that this research may show the magnitude of the problem so as to initiate intervention by the concerned authorities. Thus, the purpose of this study is to assess self- medication practice and associated factors among non-health professional students of university of Gondar who represent a large proportion of the community. Adequate education and information on self medication can be conveyed effectively once the objectives of this study are accomplished. Furthermore, issues of medications abuse and misuse can be prevented. To help improve health care, it is important to have baseline data regarding self-medication so that future interventions can be planned and regulations be implemented.
Study area
The study was conducted at four campuses of University of Gondar (Maraki, Atse Theodros, Atse Fasil and Miles Zenawi). University of Gondar located in the oldest and historic town of Gondar, northern part of Ethiopia in Amhara National Regional State, North Gondar Zone at a distance of 747 km from Addis Ababa and 170km from the Regional capital Bahirdar. University of Gondar is one of the oldest and most well established higher education institutions in the country established in 1954 as a Public Health College and Training Center (PHC & TC).Currently the University is made up of the College of Medicine and Health Sciences, the Faculties of Agriculture; Veterinary Medicine, Business and Economics Social Sciences and Humanities and Natural and Computational Sciences, and the Schools of Law, Technology and Education. There are 56 undergraduate and 64 postgraduate programs in the regular, extension, distance and summer programs including a Public Health PhD program offered by the University.9
Study design and period
Institutional based descriptive cross sectional study was conducted to assess self medication practice and its associated factors among non health professional students of University of Gondar from May 7–May 21, 2017.
Population and sampling
Source population: All regular non health professional students of University of Gondar
Study population: All regular non health professional students of University of Gondar
Sample population: Randomly selected students from each department
Inclusion and exclusion criteria
Inclusion criteria: All regular undergraduate non health professional students of university of Gondar
Exclusion criteria: Students who were not able to fill questionnaires due to serious illness.
Sample size determination
Sample size was calculated by using single population proportion formula with a source population >10,000.We have used a confidence level of 95% with 5% marginal error. As there was no previous study conducted in the study area 50% expected prevalence of self-medication was used to get the maximum possible sample size.
The sample size was calculated based on the following assumption:
Z-value of 1.96
Marginal error 5%
Prevalence 50%
Sample size was calculated as follows:
Where; Z α/2 (Standard value for 95% confidence interval) =1.96
CI (confidence interval) =95%
d (marginal error) =5%
P (single population proportion) =50%
n (sample size)
n= (1.96)2(0.5x0.5)/ (0.05)2
n=384.5≈385
nf = n final
We multiplied “n” by using design effect (1.5), 385×1.5=577.5≈578.
With 5% non-response rate the final sample size was six hundred and seven, nf =607.
Sampling technique
In this study stratified sampling technique was employed on field of study, that means natural science students(at Atse Theodros, Atse Fasil and Meles Zenawi campus) as stratum 1 and social science students(at Maraki campus) as stratum 2. Then systematic random sampling method was used to select the required number of sample size from each department. Since we had two strata, we had to divide the final total sample size (n=607) in to each stratum by using proportional allocation formula.
n1=n*N1/N Where N=Total number of study population
=12162
N1=Total number of students in stratum 1(Natural science students)
=7707
n=Total number of sample size
=607
n1=Total number of sample size from stratum 1(Natural science students)
n2=Total number of sample size from strata 2(Social science students)
n1= (607*7707)/12162
=385
n2=n-n1 607-385=222
Variables
Dependent variable
Self-medication practice
Independent variables
Age
Sex
Religion
Ethnicity
College/Faculty/School of study
Advice from friends/families/relatives
Mild illness/ non-seriousness of the illness
Emergency cases
Previous good experience with the drug
Avoidance of long waiting at health facilities
Data collection tools
Data was collected by using structured and pretested self-administrative questionnaire which was developed by adopting previous similar studies.10 Regarding data collection process we had 10 data collectors and 2 supervisors. Undergraduate nursing students were recruited and trained focusing on the study objectives and importance of keeping confidentiality and privacy.
Data quality assurance
Questionnaires were pretested for completeness and appropriateness to the local context on 30 students of Gondar Teacher Training College. The result of the pretest was discussed then important correction and changes made on the questionnaire. Every day filled questionnaires were checked in the field for completeness by all data collectors and supervisor before they return from field. Every questionnaire was checked by principal investigators every day after data collection. To keep the quality of the data, structured questionnaire was developed in English version and translated in to Amharic and then back to English to ensure its consistency of meaning.
Data processing and analysis
Data was checked for its completeness, coded and entered into computer by using Epi info Version 3.5.3 then transfer to SPSS version 20 for analysis. Descriptive statistics was used to analysis and described using percentage. The results of the study were presented by text, tables, figures and charts. P-value < 0.05 in the multivariate analysis was considered as statistical significance.
Ethical consideration
Before conducting the research ethical clearance was obtained with formal letter from the ethical review committee of the school of Nursing, College of Medicine and Health Sciences, University of Gondar, to ensure ethical acceptance of the research process some academic and administrative staffs bellow the Deans of each Colleges, faculties and schools was also communicated about the study.
Informed consent was obtained from each study subject prior to provision of self administered questionnaire after the purpose of the study had been explained to the respondents. Confidentiality of the information was assured and privacy of the respondents was maintained.
Socio demographic data of the respondents
From the total 607 planned study participants about 595 were filled the questionnaire completely, giving a responses rate of 98.02%. More than half of respondents 382(64.2%) were male, 338(56.8%) were within the age group of 21-24 years. From the mentioned ethnic group and religion more than half were from Amhara ethnicity 327(55%) and Orthodox follower 464(78%) respectively. From the respondents; School of Technology 176(29.6%), College of Natural and computational science129 (21.7%) and College of social sciences and humanities108 (18.2%), were able to completely respond our questioners (Table 1).
Variable |
Frequency |
Percent |
|
Age |
18-20 |
215 |
36.1 |
21-24 |
338 |
56.8 |
|
>=24 |
42 |
7.1 |
|
Sex |
Male |
382 |
64.2 |
Female |
213 |
36.8 |
|
Religion |
Orthodox |
464 |
78 |
Protestant |
63 |
10.6 |
|
Muslim |
57 |
9.6 |
|
Catholic |
6 |
1.0 |
|
Other |
5 |
0.8 |
|
Ethnicity |
Amhara |
327 |
55 |
Oromo |
98 |
16.5 |
|
Tigre |
68 |
11.4 |
|
SNNP |
71 |
11.9 |
|
Others |
31 |
5.2 |
|
College of Business and Economics |
79 |
13.3 |
|
College of Natural Computational science |
129 |
21.7 |
|
Faculty/school/college |
College of social science & humanities |
106 |
17.8 |
Faculty of Veterinary Medicine |
26 |
4.4 |
|
Faculty of Agriculture |
41 |
6.9 |
|
School of Education |
16 |
2.7 |
|
School of Law |
21 |
3.5 |
|
School of Technology |
177 |
29.7 |
|
Table 1 Socio demographic characteristics of non-health professional students of University of Gondar, North West Ethiopia, June 2017
Self medication practice assessment data of the respondents
Out of 595 students 226(38%) of them had taken self-medication within the past twelve month prior to the study (Figure 1). From those who had taken self-medication 159(70.35%) of them checked expiry date. Self-medication use explained to have different results among students who had used self-medication; 134(59.3%) report as their illness was improved, 37(16.37%) were cured from their illness, 25(11.06%) of them show that there illness was prevented, 20(8.85%) no change on their illness and the rest 10(4.42%) were with aggravation. Among students who practice self-medication 71(31.42%) were faced with the side effects and 155(68.58%) not faced with side effects.
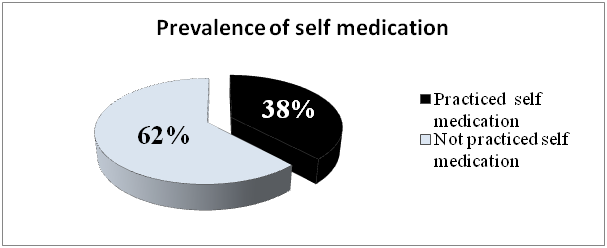
Figure 1 Prevalence of self-medication in non-health professional students of University of Gondar, North West Ethiopia, June 2017.
Reasons of study participants about self medication practice
The most commonly encountered reasons for self-medication as reported by students were Mild illness/non seriousness of the illness 77(34.07%), previous good experience with the drug 56(24.77%) and for emergency use 36(15.92%). Whereas Fear of side effects 119(32.4%), Fear of drug abuse and dependence 89(24.11%), Fear of misdiagnosis of illness 81(21.95%) and Fear of using wrong medication 73(19.78%) were the most common reasons for those who did not practiced self medication (Table 2).
Variable |
Frequency |
Percent |
Mild illness/non seriousness of the illness/ |
77 |
34.07 |
Previous good experience with the drug |
56 |
24.77 |
Emergency use |
36 |
15.92 |
Advice from friends families relatives |
32 |
14.15 |
Seeking quick relief |
24 |
10.61 |
Avoidance of long waiting at health facilities |
15 |
6.63 |
Lack of time |
10 |
4.42 |
Distance to health facilities |
8 |
3.53 |
Embarrassed of discussing own symptom |
5 |
2.12 |
Less expensiveness |
5 |
2.12 |
Other |
10 |
4.42 |
Table 2 The reasons for self-medication given by respondents who practiced self-medication in University of Gondar, North west Ethiopia, June 2017
NB: Some questions had multiple options respondents could select hence the sum of percentage is not always 100%
Common illnesses to have practiced self medication by respondents
From a total of 226(38%) respondents who took self-medication, Headache/Fever 127(56.19%) and Abdominal pain 59(26.10%) were the most frequently reported causes of illness which results in a self-medication practice (Figure 2). Our study participants agree with the fact that professional help is needed, but they mention different reasons to seek for professional help. Of those who had used self-medication, 75(33.18%) believe professional help is needed when there is severe pain, 72(31.86%) when they think the problem is so serious and 79(34.96%) need professional help when illness symptoms are worsening
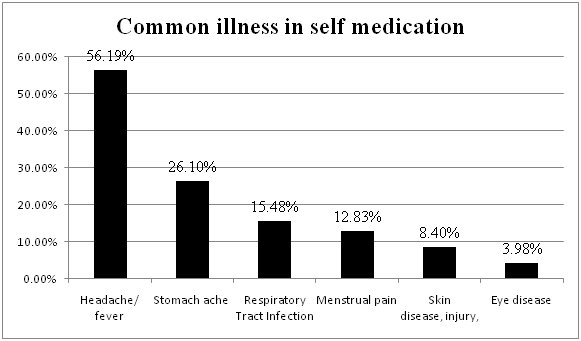
Figure 2 Common types of illness/symptoms of illness for which respondents reported to have practiced self-medication in University of Gondar, North West Ethiopia, June 2017.
Commonly used drugs for self medication by respondents
The most common drug group used in self-medication was antipyretics/analgesics that are 159(70.35%). Antibiotics and Gastrointestinal drugs were the second and third most frequently used drug groups used in self-medication with a frequency of 75(33.18%) and 31(13.71%) respectively. From seventy five (33.18%) students who used antibiotics 36(48%) of them do not have information about bacterial drug resistance. Most of the students used the drugs for less than 5 days 190(84.07%), 25(11.06%) of them had used to the duration of 5 days to 2 weeks (14 days) and the rest had used for more than 2 weeks. One hundred ninety-six (86.73%) of the study participants use self- medication only sometimes, 24(10.62%) used often and 6(2.65%) were used very often (Figure 3).
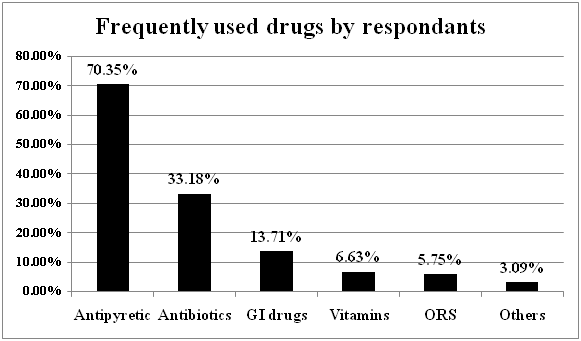
Figure 3 Frequently used drugs or drug groups for self-medication by the respondents who practiced self-medication in University of Gondar, North West Ethiopia, June 2017.
Information and drug sources for self medication
Among the students who took self-medication, the main information source for self-medication reported was previous exposure 109(48.3%) followed by Friends 74(32.30%), Pharmacist 38(16.81%),Internet or books 12(5.30%),Media9(3.98%) and 6(2.65%) were other sources. Of the total respondents those who used self-medication 134(59.29%) and 79(34.95%) have got drugs for self-medication from pharmacy and friends respectively. Students who had been using self-medication had different methods or ways of requesting drugs at pharmacy; from those 147(65.04%) got by mentioning drug names, 69(30.53%) by mentioning the symptoms of their illness, 10(4.42%) by showing old drug package which was left out, 9(3.98%) of them got the medication by mentioning the shape or any other physical characteristics of the drug and 5(2.2%) of them use other ways (Table 3).
Factors associated with self medication practice
Variables |
Frequency |
Percent |
Pharmacy |
134 |
59.29% |
Friends |
79 |
34.95% |
Family |
22 |
9.73% |
Relative |
9 |
3.98% |
Table 3 The reported sources of drugs for those who practiced self-medication in University of Gondar, North West Ethiopia, June 2017
NB: Some questions had multiple options respondents could select hence the sum of percentage is not always 100%
In the bivariate and multivariate logistic analysis we entered eight variables and finally only two variables were significantly associated with self medication practice (Table 4).
Variable |
Self medication practice |
COR (95%CI) |
AOR(95% CI) |
P-value |
||
Yes |
No |
|||||
Sex |
Male |
123(32.2%) |
259(67.8%) |
1.972(1.39-2.78)* |
2.00(1.41-2.86)* |
0 |
Female |
103(48.4%) |
110(51.6%) |
1.000 |
|||
Age |
18-20 |
82(13.8%) |
133(22.4%) |
1.000 |
||
21-24 |
123(20.7%) |
215(36.1%) |
1.078(.757-1.354) |
|||
≥24 |
21(3.5%) |
21(3.5%) |
.617(.317-1.198) |
|||
College/ Faculty/School/Of Study |
College of Business and Economics |
27(4.5%) |
52(8.7%) |
.394(.157-.988)* |
.385(.152-.974)* |
0.044 |
College of Natural Computational science |
58(9.7%) |
71(11.9%) |
2.27(.625-8.30) |
2.47(.670-9.143) |
0.174 |
|
College of social science & humanities |
37(6.2%) |
69(11.6%) |
.552(.278-1.097) |
.565(.282-1.133) |
0.108 |
|
Faculty of Veterinary Medicine |
8(1.4%) |
18(3%) |
1.18(.487-2.877) |
1.106(.450-2.714) |
0.826 |
|
Faculty of Agriculture |
20(3.4%) |
21(3.5%) |
.981(.592-1.626) |
1.12(.668-1.878) |
0.668 |
|
School of Education |
3(0.5%) |
13(2.2%) |
.644(.404-1.025) |
.695(.433-1.115) |
0.132 |
|
School of Law |
12(2%) |
9(1.5%) |
1.01(.579-1.771) |
1.064(.603-1.874) |
0.831 |
|
School of Technology |
61(10.3%) |
116(31.4%) |
1.000 |
|||
Advice of friends |
19(3.2%) |
|||||
Reason for self medication practice |
Avoid long waiting |
19(3.2%) |
||||
Emergency use |
59(9.9%) |
|||||
Mild illness |
79(13.3%) |
|||||
Previous good experience |
50(8.4%) |
|||||
Table 4 Bivarate and multivariate analysis of factors on self medication practice among respondents in University of Gondar, North West Ethiopia, June 2017
Self-medication among non-health professional students seems to be a common practice (38%) with a similar prevalence of previously reported study done in GCMHS campus of UoG, Ethiopia. Result of the present study indicates that the prevalence of self-medication amongst university students is lower than studies done in other countries, Slovenia 91.9%, west utter Pradesh college India 91.3%, Gujarat India 88%, Ghana 70%, UAE 59% and almost similar to the study done in health professional students of GCMHS UoG, Ethiopia (38.5%).Thus prevalence of self medication in current study seems reduced as compared to other previously reported studies this may be due to the reasons mentioned by respondents like fear of side effects and fear of drug dependence, differences in disease exposure and availability of student clinics in each campus.
After multivariate logistic regression analysis, it was observed that males were two times more likely to practice self medication than females (AOR: 2.00, 95% CI: 1.41-2.86). This may be due to difference in decision making for self medication use. Students from college of Business and economics are 61.5% less likely to practiced self medication than Technology students (AOR: 0.385, 95% CI: 0.152-0.974).
Most respondents use self-medication for a period of less than 5 days (84.07%) and about 5% of respondent who used self-medication took the drugs for longer than 14 days. Even though less percent of students use self medication longer than 14 days, this may be due to possibilities of miss diagnosis of perceived illnesses and utilization of wrong medication for wrong diagnosis.
Respondents also asked to report their reason that forces them to use self medication; they replied that, mild/non seriousness of the illness/ were the most common reason (27.7%). This finding is almost consistent with the findings of the study conducted in GCMHS UoG, Ethiopia (30.5%)11 they preferred to use self medication due to the less severity of the illness. The reason behind self-medication in the current study has inconsistency with study done in Slovenia Because in Slovenia study their major reason is not relate to perceived lesser severity rather it is related to reducing the burden that comes on the physician.12
In the current study illnesses or symptoms of illness for which self-medication was practiced include; headache/fever/ (56.19%) and abdominal pain (26.1%) were the most common. This finding is consistent with the findings in studies conducted in UAE10 and GCMHS UoG,11 Ethiopia, in which head ache was the most common followed by Gastric problems, eye and ear symptoms, cold, fever and allergy. In contrast, study done in Ghana show that cough/common cold was the most common symptoms followed by fever and abdominal pain.13 This may be due to the respondents’ difference in attention giving to the illness/symptoms of illness.
The main sources of information for self-medication in the current study were previous exposure (48.23%) and advice from friends (32.3%) followed by pharmacist, internet/books/, media and traditional healers. This finding is consistent with study conducted in India, in which previous exposure (83.12%) was the most common source of information for self-medication,5 While in study done in Pakistan the major source of information mentioned was from advertisements (35.7%).8 This may be due there is high drug advertisement in Pakistan than that of Ethiopia. Reading material with a percentage of (30.5%) was the most common source of information in the study done in GCMHS UoG, Ethiopia which had contradiction with the current study.11 This may be due to medical knowledge of students regarding illnesses/symptoms of illnesses and drugs.
In the current study the most common classes of drugs used for self-medication were antipyretics which was reported by 159(70.35%) of the respondents followed by antibiotics 75(33.18%). In consistent with this study analgesics and antipyretics were the most common classes of medication used in the self-medication practices in Gujarat,14 India and GCMHS UoG, Ethiopia.11 This is due to the fact that these types of drugs used to treat minor illnesses/symptoms like headache, fever and mild pain. In this study antibiotic was the second most commonly used class of drug with the percentage of 33.18%. In contrast with studies done in Gujarat India 7.72%,14 UAE (11%)10 and UoG Ethiopia (4.8%)11 had different reports about antibiotics use.15–17 These differences from the current study may be due to the differences in information about bacterial résistance of the drugs. Nearly 50% of the students who used antibiotics as self medication did not have an information about bacterial resistance.18–21
The prevalence of self medication among non health professional students of UoG was found to be 38%. In this study headache/fever, abdominal pain and respiratory tract infections were the most commonly reported conditions for self medication practice. Male students are more exposed for self medication practice as compared to female students.
Based on this finding we recommend the North Gondar health bureau to develop strategies to prevent the illegal supply of prescription and to take an appropriate action to prevent erratic use of antibiotics at university level. We also would like to recommended university of Gondar to arrange health education program to students about proper use of drugs and their effect if utilized without in consultation with health care workers.
We would like to forward our heartfelt thanks to our study participants who spend their golden time and share their experience genuinely. Our special thanks also go to our data collectors and supervisors. Finally we would like to acknowledge university of Gondar for funding.
Mengistu Mekonnen Kelkay was involved in all steps of the study from its commencement to write-up as a principal investigator; Degefaye Zelalem and Nega Tezera were co-investigators and involved in proposal write-up, data analysis and write up. All authors have reviewed and approved the submission of the paper.
The authors declare that they have no competing interests.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.