eISSN: 2373-6372


Mini Review Volume 15 Issue 5
1Richard Semelka Consulting, PLLC, Chapel Hill, USA
2Department of Radiology, Hospital da Luz, Portugal
Correspondence: Richard Semelka, MD. Richard Semelka Consulting, PLLC, 3901 Jones Ferry Road, PLLC, Chapel Hill, North Carolina Chapel Hill, NC 27516, USA
Received: November 17, 2024 | Published: November 28, 2024
Citation: Semelka RC, Ramalho M. Mesenteric Panniculitis: A comprehensive review of imaging, clinical associations, and treatment approaches. Gastroenterol Hepatol Open Access. 2024;15(5):147-149. DOI: 10.15406/ghoa.2024.15.00592
Mesenteric panniculitis (MP) is an uncommon inflammatory condition centered on the root of the mesentery. Modern MRI is the optimal imaging technique for MP, and the sequence that most consistently demonstrates it is 3-D out-of-phase T1 gradient echo imaging. MP is invariably seen in the setting of inflammation of the upper digestive tract, most notably the jejunum. At least 10% of individuals with the (Splanchnic) Metabolic Syndrome possess MP, and it is also observed with less advanced inflammatory conditions of the upper digestive tract, including irritable bowel syndrome.
In this report, we describe the state of the knowledge on mesenteric panniculitis, including imaging findings on MRI. We also report the clinical picture, focused on patient aspects. MP is much more common than previously thought, reflecting the higher imaging resolution available on modern MRI.
Mesenteric panniculitis (MP) has been traditionally considered a rare inflammatory condition of the fat in the mesentery of unknown cause.1,2 Recent clinical reports on the (Splanchnic) Metabolic Syndrome have described that MP is not infrequently present in this pan-Splanchnic system inflammatory process. Most recently, the Splanchnic Inflammatory Syndrome (SIS) entity has been described.3,4 This has been defined as the imaging features of inflammatory conditions that affect the splanchnic system. A central component is inflammation of segments of the upper digestive system tract combined with hepatosteatosis.4 In subjects with inflammation of the upper digestive tract and co-existent hepatosteatosis, MP is present in approximately 10% of these individuals.5 The digestive system and liver findings have been reported as the essential imaging features of the (Splanchnic) Metabolic Syndrome.
This report focuses on describing the entity of mesenteric panniculitis, both imaging and clinical, to provide state-of-the-knowledge information.
Imaging
CT has been the traditional imaging modality to evaluate MP. The high speed of image acquisition results in relatively breathing artifact-free and bowel peristalsis motion artifact-free image quality. These motion artifacts are the most common and essential confounding aspect for reliable demonstration of MP. MRI on modern MR systems employing 3D gradient echo imaging has overcome the aforementioned artifacts and much of the air-soft tissue susceptibility artifact from bowel gas due to very short echo times. With the control of the major artifacts that MRI is subject to, optimal demonstration of the mesentery is achievable. Presently, MRI is best suited to demonstrate MP. The most effective sequences are 3-D non-contrast out-of-phase T1-gradient echo and the combination of late arterial phase and 5-minute post-contrast GBCA enhanced images. The noncontrast out-of-phase images are the most reliable, and in settings where the use of GBCA is contraindicated, this can suffice. The postcontrast images show progressively intense enhancement of the fibrous tissue of MP.
There are several appearances of MP which reflect the phases of evolution, and are as follows:
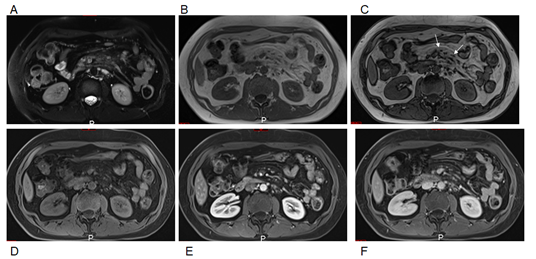
Figure 1 Moderate mesenteric panniculitis. Axial T2-weighted fat suppressed images (A). Axial T1-weighted in-phase (B) and out-of-phase (C), pre-contrast (D),arterial phase (E) and interstitial phase (F) GRE images. Moderate duskiness of the mesentery with clear demarcation with a demarcated fibrous tissue boundary (arrows, C). There is no clear tethering of the bowel.
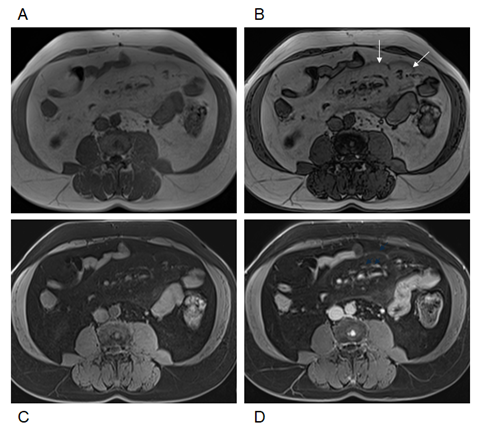
Figure 2 Severe mesenteric panniculitis. Axial T1-weighted in-phase (A) and out-of-phase (B), pre-contrast (C), and interstitial phase (D) images. Out-of-phase images (B) exhibited the greatest clarity for depicting mesenteric panniculitis. On out-of-phase images, the mesenteric fat is mild gray in signal (arrows, B) and has definable margins with a thick fibrous band. Multiple lymph nodes are present. Note the increased enhancement of mesenteric panniculitis and adjacent jejunum over time.
At 5 minutes post-contrast, pronounced enhancement of the jejunal serosa is evident in all stages. This also tends to increase in severity, especially in moderate and severe disease.
Clinical
MP is present almost exclusively when inflammatory changes of the jejunum are identified. The jejunal inflammation is best shown on 3-D 5-minute post-contrast T1-weighted gradient echo imaging. Upper digestive tract inflammation is more comprehensively reported in this prior study.3 MP, therefore, represents an extension of inflammation from the jejunum into the mesentery. Abdominal pain is a frequent clinical finding in individuals with MP. However, it is unclear if the pain is secondary to MP or the primary abnormality, upper digestive tract inflammation. It probably reflects a combination of both, with bowel inflammaton being the more dominant cause.
The clinical significance of MP is not fully understood. Minimal inflammation likely carries no additional clinical implications beyond bowel inflammation; however, it does reflect that inflammation is not isolated to the bowel but has spread beyond the serosa. However, the presence of MP is a marker that the extent of inflammation of the jejunum is relatively severe and very severe in more advanced MP. Severe MP appears to relate mainly to the duration that MP has existed, with severe disease reflecting MP's presence for many years. No doubt, severe MP can also reflect shorter-duration disease with greater inflammatory impetus.
Treatment
Treatment of MP initially must focus on treatment of the associated inflammation of the upper digestive tract. Upper digestive tract inflammation usually reflects some type of food intolerance, food allergy, or toxicity due to infective organisms or other toxins. Most cases are due to food intolerance or allergy and scrutiny of potential dietary causes by trained dieticians and gastroenterologists. As many sufferers are obese, the starting point of treatment is an overall plan of eating healthy foods and increasing physical activity. Focusing on eliminating the most common causes of intolerance and allergy is often critical. The largest category by far is removing/ minimizing ultra-processed foods.
Decreasing or limiting other well-recognized allergies/ intolerances would be the next logical step: removing gluten and excess dairy intake, eliminating smoking, and reducing alcohol intake.4,6-8 Likely, this manages 95% of afflicted cases. 5% of individuals may have more uncommon allergies/ intolerances, such as due to lecithin, as found in tomatoes. Nickel allergy has been recently reported as a possible cause of Inflammatory bowel disease (IBD) and Irritable Bowel Syndrome (IBS), with a reported incidence of 30% of sufferers of IBD and IBS having this allergy.9,10
The above approach would decrease/eliminate minimal and mild MP. Presently, it seems doubtful that dietary changes alone would improve moderate and certainly severe MP.
MP has been considered an inflammatory condition of unknown etiology. Our experience with modern MRI has shown that MP is virtually uniformly associated with inflammatory changes in the jejunum. Furthermore, rather than being rare, MP is not uncommon in individuals with a clinical history of (Splanchnic) Metabolic Syndrome or with an imaging diagnosis of SIS. MP essentially represents inflammation from the digestive tract extending into the mesentery. A fibrous demarcated margin is an interesting, consistent observation in mild to severe MP.11,12 This presumably represents a host response to containing the inflammation.
Severe MP can have a very impressive and worrisome appearance with multiple enlarged lymph nodes. It is not uncommon that individuals with this appearance undergo repeat imaging studies as the enlarged nodes raise the specter of lymphoma.13 Our experience suggests that for the entirety of cases where a dark fibrous ring encapsulates mesenteric dusky tissue, the underlying cause is nonmalignant MP. However, it is not unreasonable to think that, as with other conditions of chronic inflammation, malignancy may arise from severe, longstanding MP. We have not, however, observed it.
MP is not uncommon. The condition is shown on CT and best optimally visualized on modern MRI. Appreciation is most consistently observed on non-contrast out-of-phase T1 weighted imaging. The entity is virtually uniformly associated with inflammation of the upper digestive tract, especially the jejunum. Initial treatment is attention to diet modification.

©2024 Semelka, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.