eISSN: 2469-2794


Review Article Volume 6 Issue 2
Department of Science and Technology Nottingham Trent University, United Kingdom
Correspondence: Andrew O’Hagan, Department of Science and Technology Nottingham Trent University, Clifton Lane, Nottingham NG11 8NS, United Kingdom, Tel +447-950-875-563
Received: March 28, 2019 | Published: March 28, 2018
Citation: O’Hagan A, Wilson M. Women and substance abuse: gender-specific social, biological and psychological differences and treatment considerations. Forensic Res Criminol Int J. 2018;6(2):90–98 DOI: 10.15406/frcij.2018.06.00189
Until recently, substance abuse research focused almost entirely on men – leaving women underrepresented or overlooked entirely. Traditional methods of treatment were developed on the findings of purely male-centric research which was applied to the entire population. Research has since identified a number of gender-specific variables which limit the application of these approaches and present a case for the universal implementation of treatment-types developed specifically for women. This article represents an exploration of the cultural expectations, trauma and adverse life experiences together with comorbidity of psychiatric disorders and the role of ovarian hormones in the onset and treatment of substance abuse in women.
Keywords: Comorbidity, Women, Gender-specific, Substance abuse, Substance abuse treatment, Addiction
Substance abuse and addiction incurs huge costs to society every year - more than £15 billion in the UK alone. The bulk of this expense comes from drug-related crime and death, but close to £500 million is spent annually by the NHS to treat all manner of physical and mental conditions directly related to substance misuse.1 Drug addiction is considered a ‘disease of the brain’ because prolonged substance abuse (SA) can result in permanent changes to its physical structure and neurochemistry2 – and until recently, it was largely treated as a problem specifically reserved for men. Research surrounding substance misuse and treatment has historically focused on men and male drug-abuse - due in large part to the outdated view that, women are far less affected by the disease.3 More recently, science and society are beginning to acknowledge that females also frequently fall victim to drug use and addiction; but researchers recognise that there is variation in the substances which are more commonly abused between the sexes4,5 and the underlying causality. Increasingly, research is beginning to recognise sex-differences in all phases of abuse and across a variety of different substances – highlighting the importance of specifically tailored treatment types. Studies show that men and women tend to fall into abuse for different reasons, which offers an explanation as to why they often respond so differently to treatment. Marked differences have been noted across human and animal models6 and these variances extend beyond initiation and effectiveness of treatment. Gender-specific differences are also observed in patterns of criminal behaviour, involvement with dealing and levels of traditional employment, to name but a few.7
This paper will outline the impact of societal pressures, psychological burdens and biological influences on women and substance abuse, (Figure 1). It will also consider the implications of these underlying sex differences on substance abuse treatment and makes suggestions regarding the approaches taken to treating addicted women. Many different types of treatment are available, but individuals can fall into a cycle of substance abuse for numerous different reasons. The causation, and trigger-factors that lead to SA can heavily impact the effectiveness of certain treatment types.8 All three factors are not mutually exclusive and frequently cross-over and intertwine. Biological differences between the sexes include elements such as pharmacokinetics, hormonal variations and metabolism but also neurochemical and structural differences which closely relate to the psychological variances. Societal and cultural pressures also affect women psychologically, as the series of unattainable ideals placed upon them begin to manifest in self-objectification and subsequent mental disorders. The prevalence of these co-occurring disorders is often a triggering factor for abuse, therefore these also need to be addressed and treated simultaneously for SA treatment to be successful.
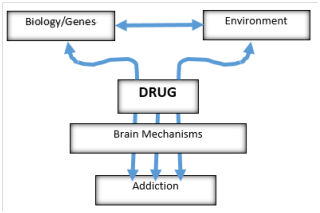
Figure 1 a simplified breakdown of the main risk factors associated with drug addiction. Adapted from National Institute on Drug Abuse.2
Societal stresses and support systems
It has been documented that reports of pre-treatment sexual abuse and trauma earlier in life are considerably higher in women than men,9,10 and links have been made between the sexual objectification (SO) of women and drug misuse in all guises.11 Sexual objectification is a broad-term, used to describe a variety of behavior’s - ranging from the relatively ‘mild’ and extending to cover sexual harassment and assault.12 In 1997, Fredrickson and Roberts developed the “Objectification Theory” which postulates reasonable linkages between SO and disproportionately high instances of mental-health disorders including disordered eating and sexual dysfunction. This study summarises how SO affects women at each life-stage, and speaks about elevated feelings of shame and increased risk of depression and anxiety.12 The theory has since been revisited and extended to suggest that instances of objectification may increase the risk of drug use and misuse in women (Figure 2).11

Figure 2 the relationship between, and pathway from, sexual objectification to substance abuse. Adapted from Carr et al.11
Patriarchal culture: Generally, modern-society is still distinctly patriarchal; which offers some explanation as to why SO is still such a prevalent issue for women. However, sexual objectification is just one of many factors and societal pressures which may be contributing to the observable rise in addiction among women. First-world attitudes towards women are slowly changing – allowing them the opportunity to be increasingly ambitious and successful in their careers. But even career-driven women often remain the main care-providers within their families, expected to always place the needs of their loved ones ahead of their own - mounting enormous pressure and increasing stress and anxiety.13 This trend has been observed and research has confirmed that women are at substantially higher risk of suffering with depression and anxiety disorders14 and are more likely to abuse prescription drugs, specifically.15
Sexual objectification within the media: Figure 2 is demonstrative of the pathways from SO to substance abuse, but also refers to self-objectification – another factor which affects women’s mental health and can ultimately lead to SA. Syzmanski’s 2011 study extends beyond ‘direct’ sexual objectification/victimisation; and suggests that cultural messages and those perpetuated by the media also impact the likelihood of women resorting to drugs. Specifically, the effects of living within cultures where objectification of the female body is the norm, and singular-ideals of what it means to be a woman and to be considered attractive are constantly reinforced in the media.16 These pressures lead to self-objectification and demoralising attempts to fulfil these cultural ideals. There is even a suggestion of a relationship between SA and the perception of ‘sexiness’, and constant body surveillance and self-deprivation.
Home life and support: Other research has indicated that drug abuse which is initiated during adolescence, is likely to be worsened by a weak family support system, or at least a perceived lack of support.17 The same study also established a strong positive correlation between familial conflict or stresses and increased levels of substance abuse. Both findings signify the importance of strong family relationships and external support-systems, and show that the absence of either can have negative implications for substance abusers. Interestingly, not all societal factors seem to influence men and women’s drug use differently - studies have concluded that there is generally no difference in the sociodemographic of male and female drug abusers.18 However, it is reported that the initiation of drug-use in women can often be influenced by and attributed to a partner who already abuses a given substance.19 Similarly, drug-using women are far more likely than men to be romantically or sexually involved with a partner who also abuses illicit drugs and less likely to be with a man who does not use drugs at all.20 These conclusions indicate that home-life stresses and support-systems continue to impact drug abuse into adulthood.
Domestic violence and substance abuse: One particularly severe and troublesome example of this, is the correlation between domestic violence and substance abuse. Reports of domestic violence against women are worryingly high, and research suggests that survivors of domestic abuse may be up to 5 times more likely to fall into patterns of alcohol and drug abuse than women that have not suffered the same experiences.21 A number of hypotheses have been developed in an attempt to rationalise or explain these statistics; some literature suggests that women may self-medicate22 as a means to deal with the trauma caused by the violent episodes which correlates with explanations relating to various other forms of trauma and suffering. A study by Macy et al.21 discusses the co-occurrence of violence inflicted by a partner, substance abuse in women and the effect each variable may have on the other. A suggestion is made that some women feel unable to remove themselves from the violent setting, as the individual inflicting the violence may be the same individual who facilitates their access to any given substance.21 This research relates back to the work of Miller20, who proved that women who abuse drugs are very likely to also have a substance-abusing partner.20 The same study also included accounts of verbal, psychological, emotional and sexual partner-violence as well physically violent experiences. It also addresses complicating factors including; incidences of violence in earlier life and childhood, substance initiation as a direct result of a violent partner, drug use that preceded partner-violence, and a reluctance to seek protection and treatment through fear of the repercussions – particularly in relation to children and child custody.21
Psychological Impact
As previously discussed, research-material focusing on female substance abusers and addicts is distinctly lacking, and findings from studies using male-only samples are frequently applied to the whole population.23 Previous research has suggested sex-differences in many of the biological and psychological responses associated with drug use and more recently, research has begun to emphasise the importance and impact of psychological differences and gender-specific experiences16 on SA. Many of the experiences and variables that have been addressed in the previous section, must also be considered in terms of the mental damage they inflict. For example, societal pressures such as sexual objectification can culminate in a number of psychological implications. In these instances, it is the abnormal thinking associated with the mental disorders which will ultimately trigger the onset of substance abuse. However, sexual objectification and abuse in adolescence or adulthood is only one predictor of psychological harm which may cause women to turn to illicit substances.
Adverse childhood experiences: Trauma in the earlier stages of life is more frequently reported by female substance-abusers than male.10 Studies as far back as the 1980’s have postulated a link between sexual-abuse in childhood, and the un-resolved issues relating to it, with a propensity for addictive behaviours in later life.24 Fernández-Montalvo et al.,25 proposed three possible explanations for the strong association between physical, sexual and psychological mistreatment and the development of SA. Firstly, that the impact of the abuse is severe enough to result in the development of post-traumatic stress disorder (PTSD) and that in these instances substance abuse is used to relieve the symptoms of the condition. The second explanation proposes that individuals who abuse drugs are more vulnerable to distress and traumatic ordeals; and that PTSD can be brought about as a result of the drug-related trauma. And the final proposition suggests that addiction and abuse often co-exist within abnormal family situations.25 Without question, there are long-lasting effects of childhood trauma of any sort – and research has shown that instances of childhood sexual abuse (CSA) are elevated in individuals with alcohol and drug abuse issues.26,27 Research has also suggested that CSA is frequently co-occurring alongside other traumatic and damaging measures,28 increasingly the likelihood of psychological damage. In 2000, a study by Kendler et al.,29 was able to prove that exposure to sexual abuse in childhood lead to increased instances of both psychological conditions and substance abuse in adult women. This suggests that drugs or alcohol may serve a functional role for survivors of childhood sexual abuse, as a means to cope with the psychological trauma caused by these early life experiences.29 Lifetime abuse seems to have detrimental consequences across a number of variables, with negative effects beyond the increased propensity for substance abuse. A comparison of treatment seeking abused and non-abused drug addicts, found that the implications of abuse penetrated all areas of the individual’s life. Addicts who had suffered abuse had a greater number of familial problems, were less likely to be able maintain permanent employment, had more problems with friends and peers and suffered more frequently and severely with psychological disorders25 (Table 1).
Lifetime abuse |
|||||
|---|---|---|---|---|---|
|
All |
Yes(n=115) |
No(n=135) |
|
|
|
n |
n(%) |
n(%) |
n(%) |
χ2 |
Family maladjustment |
|||||
Problems with |
|||||
Mother |
247 |
75(30.4%) |
42(37.2%) |
33(24.6%) |
4.6* |
Father |
239 |
76(36.0%) |
50(45.9%) |
36(27.8%) |
8.5** |
Sibiling |
239 |
78(32.6%) |
46(41.1%) |
32(25.2%) |
6.8** |
Partner |
237 |
46(61.6%) |
85(76.6%) |
61(48.4%) |
19.8*** |
Son/Daughter |
120 |
15(12.5%) |
10(18.2%) |
5(7.7%) |
3 |
Social maladjustment |
|||||
Problems with |
|||||
Intimate friends |
242 |
63(26.0%) |
42(38.2%) |
21(15.9%) |
15.5*** |
Neighbors |
247 |
31(12.6%) |
18(15.8%) |
13(9.8%) |
2 |
Work Colleagues |
247 |
71(28.7%) |
40(35.4%) |
31(23.1%) |
4.5* |
Labor maladjustment |
|||||
Without permanent job during the last 3 years |
252 |
38(15.1%) |
22(19.1%) |
16(11.9%) |
2.6 |
Psychological maladjustment |
|||||
Depressive Problems |
250 |
130(52.0%) |
77(67.0%) |
53(39.3%) |
19.1*** |
Anixety Problems |
250 |
152(60.8%) |
83(72.2%) |
69(51.1%) |
11.6** |
Violence problems |
250 |
99(39.6%) |
60(52.2%) |
39(28.9%) |
14.1*** |
Suicide ideation |
250 |
99(39.6%) |
56(48.8.2%) |
43(31.8%) |
7.4** |
Suicide attempt |
247 |
40(16.2%) |
24(21.3%) |
16(11.9%) |
3.9* |
Table 1 A comparison of maladjustment variables between abused and non-abused individuals seeking treatment for SA25
*p<0.05, **p<0.01, ***p<0.001
Comorbidity of substance abuse disorders and mental disorders: The relationship between psychiatric disorders and SA disorders has been addressed, to a certain extent, in relation to PTSD, depression and anxiety. Comorbidity of the two conditions is well-established throughout literature, and suggests linkages between a number of disorders; ranging from depression and mood-disorders to anti-social personality disorder and ADHD.30,31 Substance abuse among sufferers of mental illness is undeniably prevalent, but the explicit nature of the relationship is debated by different researchers. Many studies suggest that specific psychiatric disorders are a key trigger-factor for the subsequent misuse of substances,32 while others demonstrate that these mental disorders are in-fact a direct result of substance abuse.33 Merikangas30 suggested that previous research had been unsuccessful in establishing a single mechanism to explain the comorbidity of these disorders due to the extensive number of comorbid diseases that exist. Moreover, the way psychiatric disorders are expressed can be affected by the substances that are abused and similarly, SA may manifest differently in association with mental disorders.30 Comorbidity needs to be carefully considered when treating either disorder, as interventions for both are necessary for successful recovery.8 When the two types of disorder are examined separately, gender-specific variances are frequently observed and reported.34 However, research is generally inconclusive when attempting to establish the presence, or absence, of sex-differences in relation to comorbidity.
It is estimated that substance abuse increases the chances of developing depression by a factor of 4.78 – making substance abusers almost 5 times more likely to suffer from depression than non-abusers. Many of the environmental and social factors discussed earlier which are shown to increase the probability of substance abuse, such as a disruptive home life and elevated stress levels, are also associated with depression. Research has also shown that women are more likely to suffer from depression than men,14 and may therefore turn to a number of different substances in an attempt to self-medicate. This hypothesis has been investigated and the findings demonstrate that several illicit drugs stimulate responses from the neurotransmitters, which are affected by depression and mood disorders. In some cases, these pharmacological responses can temporarily combat Serotonin and Dopamine deficiencies, which are observed in individuals suffering from depression.35 This study perfectly encapsulates the crossover between psychological and biological factors by demonstrating how variances in one element can affect the other.
Biological impact
Substance-related gender differences have been observed in the findings of numerous studies – the suggestion being that woman are more susceptible to drug addiction than men, with a greater vulnerability particularly in the earlier stages of use that precede and lead to addiction.3 There is evidence to support a number of sex-differences, which are observed beyond psychological and cultural variances, which are based in physiology and add an additional dimension to gender-related research in this field. Studies have shown pharmacokinetic differences in the way drugs are processed by the two sexes. In 2014, Rambousek et al.36 applied this theory to an animal model and could demonstrate that, following exposure to amphetamine and methamphetamine, females displayed considerably higher levels of both substances in the brain and blood plasma. The results of this study suggested that females are at a greater-risk of toxicity and dependence.36 A number of biological causes for these differences has been suggested; with evidence generally supporting the impact of ovarian hormones and menstrual-cycle fluctuations on behavioural and neurochemical responses to illicit drugs.5,37,38
Hormonal influences: The three phases of the human menstrual cycle which are the focus of most substance-abuse research are; follicular, periovulatory and luteal. A study by Lynch in 2002, established a positive correlation between increased oestrogen levels and enhancement of the “positive” effects and behavioural responses associated with psychostimulants, such as methamphetamine.5 There is also evidence to suggest that the relative levels of oestrogen and progesterone throughout the menstrual cycle can affect the pharmacokinetic response of the body to a number of different drugs. The same heightening effect can be seen when progesterone-levels are comparatively low and the effects of oestrogen are rather uninhibited.5 These hormonal influences affect all amphetamine-type drugs which may indicate why they are among the substances most commonly abused by pregnant women.39 Other studies have reported similar findings in relation to cocaine and a greater ‘high’ during the follicular phase of the menstrual cycle.5 In contrast, progesterone seems to have the opposite effect and has even be associated with a reduction of cravings in female cocaine users.40 However, Quinones-Jenab and Jenab suggest that the diminishing effect of progesterone on the pleasant stimulation is potentially dangerous. They speculate that women may be at a higher risk of overdose if they attempt to reach their usual high during the luteal phase of menstruation when progesterone levels are at their lowest.41 Menstrual-cycle fluctuations have also been shown to affect the pharmacokinetic properties of a number of different drugs; from rates of absorption to gastrointestinal motility of orally administered drugs and bioavailability.5,42 These changes are not purely due to hormonal variation; physiological changes that occur throughout the menstrual cycle can also affect some of pharmacokinetic effects of drugs. Basal metabolic rate, heart rate, blood pressure, water retention and immune function all undergo variation through the menstrual cycle, in-line with hormonal fluctuation.42
Stigmatisation
A number of studies have acknowledged elevated levels of stigma and social disapproval towards female drug users when compared to men,5,43 which offers an explanation for the lack of research focusing on female drug use and addiction. Two reasons for this imbalance have been postulated; one rooted in the societal views and expectations of ‘female virtue’ and the other based upon traditional gender roles and the perception of women as nurturers and care-givers.43 However, a study by Nicolaides in 1996 suggested that as societal attitudes towards women are slowly changing, so too are opinions surrounding their drug use – the findings suggest that stigmatisation towards women is beginning to decrease and that female SA is becoming more ‘acceptable’ in the eyes of society.44 Other research suggests that the sex-differences in frequency of drug use can be attributed to differences in opportunity rather than fear of judgement or criticism.5
Drug acquisition
Drug acquisition, and participation in any level of the drug market, is determined by opportunity. A 1993 survey on drug abuse revealed that men have far greater access to marijuana, cocaine, hallucinogens and heroin than women do.45 Research has shown that there are distinct gender-differences in the opportunities that are presented and the strategies used by men and women to obtain drugs – the general consequence of which is that women have limited involvement in the profitable activities, such as distribution, and often utilise different routes of acquisition.46 Griffin and Rodriguez describe ‘sexist and segregated’ systems of drug-distribution where women occupy purely subsidiary roles and are governed by men. The same study also suggests that familial ties, such as being married or having children, will likely affect men and women’s ability to expand their social networks differently.46 This is relevant because a strong association has been established between social networks and access to all types of illegal opportunities, including drug market participation – which may explain why women are less likely to acquire drugs in face-to-face cash transactions than men.46 This may be one of a number of factors fuelling the increasing popularity of alternative routes of acquisition; in particular, the growing use of the internet to facilitate drug procurement.
Drug accessibility: Online pharmacies: Although the majority of research around the area is relatively recent, drug use itself is not a modern concept. Drugs have been used and abused historically across many different cultures and countries – with the first known record of Opium made more than 5400 years ago.47 However, it is not necessary to delve so far into the past to be able to observe the changes that the modern world has had on the attainment and use of illicit substances. Since the 1990’s, the internet has become an increasingly integral part of our daily lives and it is now possible to purchase products and services of all types quickly and conveniently. With this, has come the ability to acquire a large number of medicines and medical supplies – including those, which are usually reserved for patients with a medical prescription from a registered healthcare professional.48It is now easier than ever to obtain a huge number of different pharmaceutical products, a service that has the potential to be enormously advantageous by increasing convenience and lowering costs.49 Unfortunately, the access to controlled drugs via the internet provides endless opportunities for its misuse – including the illicit sale and acquisition of pharmaceuticals.50,51 The scale of which has been demonstrated by a study carried out by the National Centre of Substance Abuse (CASA), which suggests that ~85% of internet pharmacies are distributing controlled medication without requiring the customer to provide proof of prescription.52Table 253 shows the availability of 11 different controlled drugs at 175 online pharmacies, and how many required proof of prescription before purchase. These “pharmacies” assist substance abusers, from every socioeconomic group and of all ages54 to access substances which feed their dependency. In the past 15 years there has been a substantial increase in the abuse of prescription drugs55 – a timeline which corresponds with the growth and prevalence of internet pharmacies.56
|
All Ops, N= 175 |
Prescription Ops, N=39 |
No-Prescription Ops N=136 |
|||
|---|---|---|---|---|---|---|
|
n |
% |
n |
% |
n |
% |
Sidenafil |
161 |
92 |
37 |
94.9 |
124 |
91.2 |
Fluoxetine |
144 |
82.3 |
38 |
97.4 |
106 |
77.9* |
Tramadol |
128 |
73.1 |
31 |
79.5 |
97 |
71.3 |
Amitriptyline |
116 |
66.3 |
33 |
84.6 |
83 |
61.0* |
Valproiv acid |
58 |
33.1 |
25 |
64.1 |
33 |
24.3* |
Alprazolam |
39 |
22.3 |
13 |
33.3 |
26 |
19.1 |
Codeine/hydrocodone |
36 |
20.6 |
12 |
30.8 |
24 |
17.7 |
Phentermine |
26 |
14.9 |
9 |
23.1 |
17 |
12.5 |
Methylphenidate |
10 |
5.7 |
6 |
15.4 |
17 |
12.5 |
Stanozolol |
7 |
4 |
4 |
10.3 |
3 |
2.2* |
Amphetamine |
4 |
2.3 |
4 |
10.3 |
0 |
0† |
Table 2 The availability of 11 controlled substances at online pharmacies, with and without a prescription53
*Fisher’s test: p<0.05.
†Fisher’s test: not performable
Counterfeit pharmaceuticals: Hidden beneath the cover of the legitimate online trade of regulated substances, is a large and rapidly expanding ‘black-market’, which facilitates the trade of unapproved and counterfeit pharmaceutical products.51 Leading drug manufacturers have proposed that around 2 million. UK residents purchase prescription medication online every year.57 Estimates suggest that imitation drugs make up over 50% of this online market,53 meaning that less-than-half of these consumers are receiving genuine pharmaceutical products and could be ingesting any potentially fatal chemical-cocktail. The impact of which will affect individuals seeking to use the drugs for recreational or non-medical purposes as well as those treating genuine medical conditions.58 Even discounting the counterfeit products, it’s abundantly clear how these internet sales can enable an individual to exploit and misuse prescription drugs which they would otherwise have limited, or no, access to.
Online pharmacies and women: The three types of prescription drug most commonly misused are; opioids, sedatives and stimulants.59 For a number of reasons, online access to these classes of drug are likely to have a greater impact on women than men. Generally, women are at a considerably higher risk of suffering with insomnia, depression and anxiety disorders14 and are therefore more likely to turn to drugs in order to cope with anxiety and periods of stress.60 Consequently, it would be reasonable to assume that the number of women in possession of legitimate prescriptions to treat these disorders is greater than the number of men. However, the possession of a valid prescription does not guarantee that the recipient is using the drugs for their intended purpose. A 2014 study by Worley and Thomas exposes the phenomenon known as “doctor-shopping” – where women obtain medication from several different prescribers for non-medical use.61 Other studies have shown that women are more likely to abuse
Online pharmacies and women: The three types of prescription drug most commonly misused are; opioids, sedatives and stimulants.59 For a number of reasons, online access to these classes of drug are likely to have a greater impact on women than men. Generally, women are at a considerably higher risk of suffering with insomnia, depression and anxiety disorders14 and are therefore more likely to turn to drugs in order to cope with anxiety and periods of stress.60 Consequently, it would be reasonable to assume that the number of women in possession of legitimate prescriptions to treat these disorders is greater than the number of men. However, the possession of a valid prescription does not guarantee that the recipient is using the drugs for their intended purpose. A 2014 study by Worley and Thomas exposes the phenomenon known as “doctor-shopping” – where women obtain medication from several different prescribers for non-medical use.61 Other studies have shown that women are more likely to abuse drugs obtained with a legitimate prescription than men - proving that this behaviour is not uncommon, and rather characteristic, of women who abuse prescription medication.62 Research has confirmed that doctor-shopping is one of the most common routes for diverting prescription drugs away from the legal market,63 proving that even ‘legitimate exposure’ to these substances can lead to both deliberate and unintentional misuse.
Gender specific substance abuse treatment
Mechanisms to access and acquire drugs are not the only element of substance abuse to have changed and adapted with modern life. We are now also beginning to see a shift in the manner with which substance abuse treatment is administered to sufferers – including a greater sensitivity towards the unique needs of women.
Unique health concerns: The differences between male and female substance abusers are far-reaching and fundamental to the development of effective treatment plans. Physiology and hormonal variation must be considered, but the lasting effects of gender-specific experiences, co-occurrence of physical or psychological disorders and cultural pressures are equally as important. This was concisely summarised in 2009 by the US Department of Health and Human Services, who released a document stating that; “differences between women and men in genetics, physiology, anatomy, and sociocultural expectations and experiences lay the foundation that women have unique health concerns related to substance use disorders as well as elevated risk for certain co-occurring physical and mental issues or disorders”.39 A large proportion of women entering substance-abuse treatment have experienced abuse or trauma of some kind throughout their lives – be that physical/domestic, in childhood, psychological or sexual abuse. They are also far more likely have a partner that also abuses drugs20 but frequently have children and other dependent family members to consider when initiating treatment.21 For this reason, women’s recovery tends to be heavily associated with repairing relationships and the development of a healthy support system.64 Substance abusing mothers require greater attention still and additional considerations must be made, particularly regarding access to childcare.65 Studies show that when provision is made to allow a woman’s children to be present with her during treatment, retention rates are higher, and the integration of a family dynamic is generally beneficial.64
Pregnancy: In the same way that it is important to tailor substance abuse treatments specifically to the needs of addict-mothers,64 a family-centric approach to recovery is equally critical for pregnant women. Additional medical risks and complications when substance-abuse occurs during pregnancy. Prenatal drug use is incredibly dangerous for the unborn child and is associated with miscarriage, premature delivery, cognitive problems and neonatal abstinence syndrome to name but a few.66 However, studies suggest that participation in prenatal treatment for substance abuse can improve the health and outcomes for both the mother and offspring.67,68 Unfortunately, the negative consequences for the children do not end at birth – postnatal substance abuse is heavily associated with instances of child abuse and neglect and if abuse persists, authorities will most-likely intervene and the child may be removed from their care.65 The first barriers to treating pregnant women arise when attempting to identify those in need and then successfully encouraging them to seek help. Women who use drugs or suffer from addiction generally face substantially more criticism than men.5 The disapproval and judgement increases exponentially if the woman in question is pregnant - women may be reluctant to come forward because they are ashamed, fear losing custody or risk of prosecution.65
Interventions for co-occurring conditions: Many women turn to substance abuse to cope with a number of cultural, societal and personal pressures.11 The internal stress caused by these mounting burdens and pressures, has been associated with the development a number of psychological disorders. Comorbidity influences substance abuse and treatment in a number of ways, and these vary with the associated disorders and the way they interact with one another and manifest in the individual.30 Research has shown substantially increased incidences of a large number of psychiatric disorders in substance abusers; and both conditions will require simultaneous intervention for treatment of either one to be entirely successful.8 Relative to the general population, mood and anxiety disorders are more common in women for a number of reasons. In combination with the elevated rates of depression and anxiety seen in substance abusers, this needs to be carefully assessed and considered before attempting to treat female addicts. Across their lifetime, women are far more likely to be subjected to abuse and trauma than men.#ref10 These experiences can be incredibly damaging to an individual, and if they are not properly processed or addressed can develop into various psychiatric problems;25 even as severe as post-traumatic stress disorder. The co-occurrence of these two conditions is particularly challenging to treat.69 It has been suggested that women who have suffered to this extent, use substance abuse as a form of self-medication to remedy the adverse symptoms that are associated with the condition.25 In cases like this, substance use is elicited as a coping mechanism. Therefore, it is imperative that the underlying trauma is treated and rectified – without making this a priority, it will not be possible to successfully treat the associated addiction.
Exploiting biological differences to develop novel treatment types: Studies investigating the impact of gonadal and ovarian hormones has revealed the attenuating effects of elevated progesterone levels on cocaine use and cravings, particularly in women.3,40 This discovery has prompted some researchers to consider the possibility of developing progesterone-based medications to treat cocaine addiction.3,38,41 Early data suggests that applications to men may be limited but that higher concentrations would need to be tested to confirm this.40
Recommendations: The main adjustments that should be made to female-specific substance abuse treatment, are rooted in causation and environment. Because, in women specifically, substance abuse is frequently caused or aggravated by past experiences of trauma and unbalanced lifestyles which culminate in psychiatric disorders.25,29 All of which are complicating factors that impact treatment and need to form a part of the original treatment-plan. Comorbidity should always be considered in substance-abusers, but it is so prevalent in women that it is even more imperative that it is addressed in the earliest stages of assessment and treatment. Home life and family situations are more influential factors in women’s substance use than men’s. Routes of acquisition should be considered, and an attempt should be made to establish who or what is the main source of access in the women’s life. Female drug use is frequently facilitated by men21 – specifically sexual and romantic partners.19,20 If a woman is placed back into a situation where she is surrounded by substance abuse, the risk of relapse is hugely increased. Women need to be assisted in improving their social networks and home lives - and where appropriate, helped to remove themselves from abusive and dangerous environments. Mothers and pregnant women should be treated without judgment and with compassion; the emphasis should be placed upon improving health and family life, rather than adopting a threatening or confrontational approach. And critically, women’s mental health should always be considered as a primary cause for substance abuse initiation and these aberrations should be treated simultaneously. Improving mental health and addressing repressed trauma are critical to recovery.
Much of the time, women who suffer with substance abuse disorders are simultaneously suffering with at least one other condition. Regardless of the specific comorbid disorder that exists alongside the addiction, the implications for treatment are very similar. In order to fully recover from a substance abuse disorder, the underlying causation and trigger-factors need to be established and addressed.8 Sometimes, drugs and alcohol are exploited to block out other sources of pain or hurt. Histories of trauma and abuse are incredibly prevalent in female substance-abusers.64 If women are resorting to drugs as a means to cope with anxiety, depression, stress or trauma then the substance abuse really only exists as a symptom of that condition.22 In this case, treating only the drug-related issue would mean removing the coping mechanism but ignoring the cause.29 The likelihood of successful recovery would be substantially decreased; and even if it was initially effective, the chances are that the individual would quickly relapse or that the pain would manifest in another equally harmful way. The individual may, or may not, be aware of the presence of these secondary conditions. For this reason, counselling should be incorporated into all treatment programs. enabling the individual and the treatment provider to establish any other issues which need to be addressed, which in turn, will increase the likelihood of treatment retention and success in recovery.8
Mothers are often reluctant to seek help for their addiction through fear of the repercussions and authority-involvement.21 When treating substance abusing mothers, it is especially important that the treatment provider is sensitive and flexible where necessary. Women largely take on the role as the main care-provider to their families, and this is still true of substance-abusing women. Access to childcare, or lack thereof, prevents some women from seeking or staying in treatment65 - If more facilities could allow women to bring their children with them, research suggests that retention would be universally increased.64 This also helps to reinforce a family-dynamic, which is significant because home life and support systems are so critical to substance abuse. A lack of familial-support, chaotic home lives and excess stress are all associated with the onset of SA,17 and it is crucial to address these factors when attempting to treat it. A focus on social aspects such as; relationship building, improving family-relations and making ‘healthier’ choices in peers and partners would benefit treatment-seeking women greatly.70,71
None
None

©2018 O’Hagan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.